Headache Management in Community Pharmacies
EM O'Sullivan, Br Sweeney, E Mitten, C Ryan
Headache Clinic, Department of Neurology, Cork University Hospital, Wilton, Cork
Abstract
Many headache patients self-medicate and choose their preferred analgesic from a range of acute analgesics available on the high-street and from community pharmacies. Little is known about their presenting symptoms, headache diagnosis and their preferred treatments. A questionnaire was distributed to community pharmacies in the Munster region of Ireland and was administered to patients requesting treatment for headache. A total of 1023 completed questionnaires were received, 76.7% (n=765) were female and 51.8% were aged 18-39 years. 53.3% (n=542) were not previously diagnosed by a GP and 49.6% (n=502) had never sought advice from a pharmacist. According to the symptoms described, 32% (n=327) had episodic migraine and a further 15.2% (n=155) had probable episodic migraine. 30.3% (n=310) had tension type headache. 10.7% (n=105) had chronic daily headache. Codeine based products were the preferred treatment choice for 43.1% (n=441). Triptans were the most effective, 68.6% (n=166), in those for whom they were previously prescribed. 11.8% (n=121) had medication-overuse. The community pharmacist is an important resource in headache management. An expanded role incorporating best practice management guidelines has the potential to improve the outcomes for many headache sufferers.
Introduction
Benign headache disorders are associated with high levels of disability, with 46% of the adult population suffering from an active headache disorder. Tension type headache is the most common form of headache and affects 42% of all headache sufferers, followed by migraine (11%) and chronic daily headache (3%)1. The mainstay of treatment for all headache types is the use of appropriate pharmacotherapy, tailored to the individual, considering the type and severity of his/her symptoms2. Headache sufferers frequently self-medicate with a wide variety of analgesics, ranging from paracetamol, aspirin and ibuprofen available for purchase on the high-street, to exclusive pharmacy only preparations e.g. paracetamol/codeine. Epidemiological studies on
highlight that only half of migraneurs and one-sixth of tension type headache sufferers consult their general practitioner (GP) for guidance with their management3, and it is not known what proportion of patients consult with their community pharmacist when selecting an analgesic product. It is therefore not known if this patient group is being managed appropriately. This study therefore aimed to describe the cohort of patients who present to community pharmacies requesting treatment for a headache, establish a diagnosis of their headache type based on symptoms described, and assess the appropriateness of each patient’s management.
Methods
A questionnaire was developed and distributed to 75%, random sample, of all community pharmacies in the Munster region of Ireland, and included a mixture of urban, sub-urban and rural community pharmacies. Of those initially contacted, 43% (n=158) agreed to take part in the study (32% of total Munster numbers). Each pharmacy was supplied with ten questionnaires and a stamp addressed envelope to return the completed questionnaires to the chief investigator. Pharmacists were asked to recruit ten consecutive patients presenting to their pharmacy requesting an analgesic for headache, and invite them to complete a self-administered questionnaire. Patients had to be aged 18 years or older. The questionnaire contained three main sections: demographics, presenting symptoms and preferred treatments. The demographics section detailed patient’s age, sex and medical card status (indicative of free GP access in the Irish healthcare system)4.
The symptoms section of the questionnaire asked patients to provide details of the: time (years/months) since onset of first attack, frequency and duration of untreated attacks, location of pain, severity, and presence of associated symptoms. Patients were also asked if he/she had been previously diagnosed by a GP and if he/she had ever sought advice from a pharmacist. Within the “preferred treatments” section, patients were asked to outline the list of medication(s) they previously used to alleviate headache symptoms, identify their preferred choice and detail the time taken to gain relief. Patients were also asked to note how confident they were in their ability to manage their headaches. All questionnaire data was inputted into SPSS version 21 and univariate statistical analysis was performed using SPSS. Data was summarised using frequencies and percentages and statistical significance was determined using Chi-square tests. Results were considered significant of p < 0.05. Ethical approval was granted for the study by the Clinical Research Ethics Committee of the Cork Teaching Hospital, University College Cork.
Results
1580 questionnaires were distributed and 1023 (65%) were returned. The majority of respondents were female, 76.7% (n=765), and over half (51.8%, n=527) were aged between 18 and 39 years. Nearly a third of participants (29.2%, n=298) had a medical card. More than half (53.3%, n=542) did not have a previous physician diagnosis and those more likely to have an official diagnosis considered their headaches severe (p<.0001), suffered from vomiting concomitantly with headache (p<.0001) and those with chronic daily headache i.e. >15 headache days per month. 50.4% (n=511) had previously sought advice from the pharmacist when choosing an acute therapy and was independent of headache type.
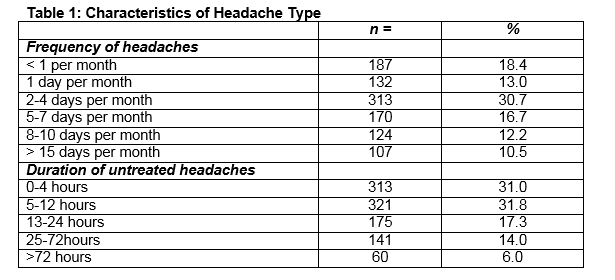
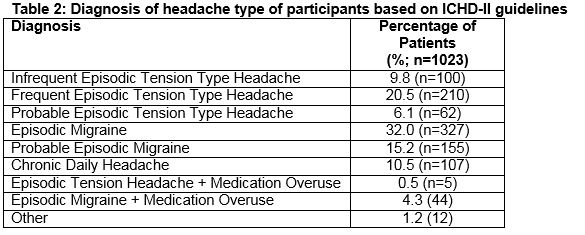
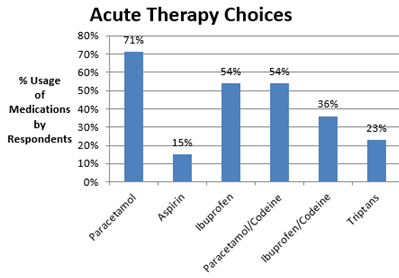
The frequency of acute headaches in days per month, as estimated by participants were: <1 per month: 18.4% (n=187), 1 day per month: 13 % (n=132), 2-4 days per month: 30.7% (n=313). The duration of untreated headache episodes were: 0-4 hours: 31% (n=313), 5-12 hours: 31.8% (n=321) (Table 1). The clinical interpretation was assessed by a GP and migraine specialist in accordance with the ICHD-II guidelines5. 30.3% (n=310) had episodic tension type headaches. 32% (n=327) had episodic migraine attacks with a further 15.5% (n=155) having probable episodic migraine (Table 2). Medication-overuse headache (defined as consuming combined analgesics or triptans on > 10 days per month or simple analgesics on >15 days per month) was identified in 11.8% (n=121) of the study population. The frequency which patients treated acute attacks with analgesics was: always: 26.2% (n=267), often: 27.8% (n=283), sometimes: 43.9% (n=447) and never: 2.1% (n=21). Preparations chosen by individuals at any time in the past were: paracetamol (71.3%, n=729), aspirin (15.5%, n=158), ibuprofen (54.2%, n=551), paracetamol/codeine (55.4%, n=554) and ibuprofen/codeine (36.7%, n=374). Triptans, available as a prescription-only medications were previously dispensed for 23.8% of patients (Figure 1).
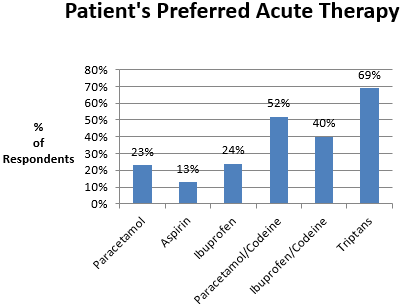
Patient preference identifies the medication considered to be the preferred treatment option in providing headache relief. 52.3% (n=290) who used paracetamol/codeine preparations (n=554), found them to be their preferred choice. 40.4% (n=151) choose ibuprofen/codeine (n=374). These were followed by ibuprofen, 24.3% (n=134), paracetamol, 22.6% (n=165) and aspirin, 12.7% (n=20). The triptans prescribed previously for 23.8% (n=242) were identified as the preferred choice for 68.6% (n=168) (Figure 2). Headache relief was achieved in 46.9% (n=473) of patients within 60 minutes and a further 28% (n=282) within 1-2 hours. 13% (n=128) got relief in 2-4 hours. 10% (n=105) in > 4 hours and 2% did not find analgesics effective. The majority of patients, 82.9% (n=827), were satisfied with their ability to self-medicate, but 17.1% (n=171) were not confident in their ability to effectively manage their headaches.
Figure 1
Figure 2
Discussion
This is the first study that has been conducted to describe the cohort of patients who attend community pharmacies requesting over-the-counter analgesics for the management of headache symptoms in Ireland. Half of the participants had not consulted a GP for an official diagnosis and only half had ever sought advice from the pharmacist with regards to selecting an appropriate analgesic to alleviate symptoms. The most frequently uses analgesics were the simple analgesics (paracetamol or ibuprofen) whilst the preferred treatment choices were codeine based products which is a key finding as they are recommended second line and are an important risk factor for medication-overuse headache6. A substantial proportion of patients reported that they did not receive complete alleviation of symptoms, suggesting that the management of this patient group could be improved. The importance of receiving an official diagnosis of headache from an appropriately trained healthcare professional e.g. GP/neurologists cannot be overlooked. A consultation based on the ICHD-II guidelines enables a correct diagnosis to be made and recommendations for appropriate acute therapies based on the diagnosis, disability and severity of attacks can follow in line with the most up to date clinical guidelines. Furthermore, community pharmacists can have a central role in counselling patients, particularly in relation to potential side effects of headache therapies and the concomitant use of headache therapies and other chronic medications in patients with significant morbidities. Additionally, pharmacists can identify patients who require referral to their GP.
With regards to the choice of analgesics, the demand for codeine based analgesics was frequent, and that for aspirin was lowest (Figure 2). The usage of codeine based products was highest amongst those who suffer from episodic migraine, probable episodic migraine and chronic daily headache. Chronic daily headache was more common in this study than in the wider community (10.5% versus 3-4%), suggesting that whilst this patient group do not request advice from the pharmacist, they visit the pharmacy to purchase “stronger” analgesia than is available for purchase on the high street. Whilst patients did not request advice from pharmacists, the finding that codeine based products were a frequent choice of analgesic is important as codeine based products carry risks of habituation, tolerance, dependence and the development of chronic daily headache with medication-overuse. In addition codeine products are not recommended in any of the international guidelines for tension type headaches7. Medication-Overuse-Headache has a community prevalence of 1%-2% and a 3:1 female to male ratio. Its peak prevalence is in mid-life. Risk factors for the disorder are a progressive increased frequency from episodic migraine attacks or episodic tension type headaches to near-daily headaches (>15 days per month) with the concomitant overuse of analgesics, particularly codeine-based products. Other risk factors include co-morbid psychiatric disorders (depression and anxiety states) and obesity8. It is therefore important that these patients receive the appropriate advice and counselling from pharmacists to ensure they are aware of the potential for harm. In pharmacies, since August 2010, the sale of codeine based analgesics is restricted, considered second line and limited to short term use. The relative lack of use of aspirin is notable, particularly as it is recommended as first line treatment for both tension type headache and migraine9. This low usage may perhaps reflect either a relative lack of awareness of aspirin as a worthwhile analgesic amongst the patient group, or possible fear of side effects10.
Time to achieve headache relief after treatment, was reported by the majority of patients to occur within two hours, which is a good clinical outcome. This illustrates that many patients can confidently self-medicate. Nevertheless, for several of the participants, it took longer than four hours to achieve relief of symptoms, which signifies a lack of efficacy11. These patients are therefore not optimally managing their headaches, reflecting the hidden disability and un-met needs of many headache sufferers12. The majority of patients in this study did not have a medical card. This may suggest that the cost of accessing a GP was a barrier to consulting, although this was not explicitly determined as part of the study. Whilst several patients were confident at self-management and received appropriate benefit, this study highlights that there is a cohort of headache suffers who have not received an appropriate diagnosis and are not managed accordingly. As these patients present to community pharmacy, the community pharmacists has a role to play in their management, and development of this role should be further explored. Future studies in community pharmacies focusing on headache disability using patient reported outcome measures(PROMS), health related quality of life(HRQoL) and the MIDAS (Migraine Disability Assessment) questionnaire will quantitatively and qualitatively measure the personal impact, time lost from work, reduced productivity and reduced income of headache sufferers13. In conjunction with the ICHD-2 diagnostic guidelines the at risk groups, chronic migraine and medication-overuse-headache can be identified and appropriate interventions made.
The main limitation of this study is patient preference of acute therapy choices, as a determinant of efficacy, as this has none of the rigors of a clinical trial. The data in addition is retrospective with potential for bias in recall. The questionnaire only enabled a single diagnosis be attributed to each respondent.
Correspondence: E O' Sullivan
Headache Clinic, Department of Neurology, Cork University Hospital, Wilton, Cork
Email: [email protected]
Acknowledgements
All the pharmacies who participated and the patients who gave up their time to complete the questionnaire; and the Irish Pharmaceutical Union and the Migraine Association of Ireland both of whom endorsed the study. The study was partially funded by an educational grant from Menarini Pharmaceuticals.
References
1. Stovner LJ, Hagen K, Jensen R, et al. "The global burden of headache: a documentation of headache prevalence and disability worldwide." Cephalalgia 2007;27:193-210.
2. Sinclair AJ, Matharu M "Headache management: pharmacological approaches." Practical Neurology 15.6 (2015): 411-423.
3. Steiner TJ, Lainez MJ. "Recommendations for headache service organisation and delivery in Europe." The Journal of headache and pain 12.4 (2011): 419-426.
4. Nolan A. "Evaluating the impact of eligibility for free care on the use of general practitioner (GP) services: a difference-in-difference matching approach." Social science & medicine 2008;67: 1164-1172.
5. Olesen J, Steiner TJ. "The International classification of headache disorders, 2nd edn (ICDH-II)." Journal of Neurology, Neurosurgery & Psychiatry 2004;75: 808-811
6. Lipton RB. "Risk Factors for and Management of Medication-Overuse Headache." Continumm Lifelong learning in neurology. 21.4, Headache (2015): 1118-1131.
7. Maguire, T. "Community-based headache management." International Journal of Clinical Practice 69.S182 (2015): 17-20.
8. Kristoffersen ES Lundqvist C. "Medication overuse headache: epidemiology, diagnosis and treatment." Therapeutic advances in drug safety (2014): 2042098614522683.
9. Lampi C, Voelker M, Steiner TJ, "Aspirin is First-Line Treatment for Migraine and Episodic Tension-Type Headache Regardless of Headache Intensity." Headache: The Journal of head and facial pain” 52.1 (2012): 48-56.
10. Kirthi V, Derry S. "Aspirin with or without an antiemetic for acute migraine headaches in adults." The Cochrane Library (2013).
11. Lipton RB, Cady R. "Ineffective acute treatment of episodic migraine is associated with new-onset chronic migraine." Neurology 84.7 (2015): 688-695.
12. Lipton RB, et al. "Examination of unmet treatment needs among persons with episodic migraine: results of the American Migraine Prevalence and Prevention (AMPP) study." Headache:The Journal of head and facial pain. 53.8 (2013): 1300-1311.
13. D’Amico, D., et al. "Disability and quality of life in headache: where we are now and where we are heading." Neurological Sciences. 34.1 (2013): 1-5.
p373