What Proportion of Patients Meet the Criteria for Uncomplicated Sepsis in an Irish Emergency Department?
C McNevin1, R McDowell2, F Fitzpatrick3,4, P Gilligan5, A Wakai 5,6
1Royal College of Surgeons in Ireland (RCSI) Medical School, Dublin 2, Ireland.
2RCSI Department of General Practice, Division of Population Health Sciences (PHS), Dublin 2, Ireland.
3Department of Clinical Microbiology, RCSI Education & Research Centre, Beaumont Hospital, Dublin 9, Ireland.
4Department of Microbiology, Beaumont Hospital, Dublin 9, Ireland.
5Department of Emergency Medicine, Beaumont Hospital, Dublin 9, Ireland.
6Emergency Care Research Unit (ECRU), PHS Division, RCSI, 123 St Stephens Green, Dublin 2, Ireland.
Abstract
Emergency medicine plays a central role in the early recognition of patients presenting to hospital with sepsis. However, the epidemiology of sepsis in the Irish Emergency Department (ED) setting has not been described. The primary aim of this study was to determine the proportion of adult ED patients who meet the current criteria for uncomplicated sepsis. This cross-sectional study was performed in the ED of Beaumont Hospital, Dublin. The clinical records of all patients presenting to the ED over a four-week period were retrospectively screened to determine if they met the current Health Service Executive (HSE) criteria for uncomplicated sepsis. Overall, 3,585 adult patients attended the ED during the study period, with 152 patients meeting the criteria for uncomplicated sepsis. The proportion of ED patients who met the criteria for uncomplicated sepsis was 4.24% (95% CI 3.57-4.91%).
Introduction
Sepsis is a clinical syndrome resulting from a dysregulated inflammatory response to infection characterised by a generalised pro-inflammatory cascade, which may result in generalised tissue injury1. It encompases a clinical spectrum of severity, including uncomplicated sepsis, severe sepsis and septic shock. While hospital statistics do not capture the underlying cause of death data in Ireland, in 2013 up to 60% of all hospital deaths had a sepsis or infection diagnosis2. It is in this context that the Irish government has launched a new national effort to tackle sepsis, involving a new national guideline2 and the first national sepsis summit which was held in Dublin in July 2015.
Meanwhile, many patients with sepsis are admitted to hospital through the ED3, and a significant proportion of these patients deteriorate to septic shock4. Consequently, the Irish national guideline recommends that ED patients with a history suggestive of infection have sepsis screening performed2. Despite the importance of the ED in the early recognition of patients with sepsis, to the best of our knowledge, there is no published study on the epidemiology of sepsis in the Irish ED setting. The primary aim of this study was to determine the proportion of adult ED patients who met the criteria for uncomplicated sepsis (i.e. sepsis with no evidence of shock or any end-organ dysfunction). The secondary aim was to determine the demographic and clinical characteristics of these patients.
Methods
This cross-sectional study was performed in the ED of Beaumont Hospital, Dublin. The annual census of the ED is approximately 50,000. The Beaumont Hospital Ethics (Medical Research) Committee approved the study.The clinical records of consecutive patients presenting to the ED over a one-month period (July – August 2015) were screened using the HSE Sepsis Screening Form5.
The clinical records were retrospectively reviewed within 24 hours of ED arrival. Sepsis was defined as clinical suspicion of an infection together with at least two features of the systemic inflammatory response syndrome (heart rate > 90 beats per minute; respiratory rate > 20 breaths per minute; temperature <36°C or >38.3°C; altered mental status; blood glucose > 7.7 mmol/L in a non-diabetic patient; and white cell count <4000/μl or >12000/μl)2,5. Only the initial observations on ED presentation were used in this study.
Data on patient age, gender, heart rate, respiratory rate, temperature, Glasgow Coma Scale (GCS) score, blood glucose, white cell count, presence or absence of diabetes were obtained from the clinical records. Where one or more of the systemic inflammatory response syndrome (SIRS) criteria used to diagnose sepsis had not been recorded for an individual, the diagnostic criteria were applied to all available data.
Data was analysed with descriptive statistics and reported as frequencies, proportions, percentages, medians and interquartile ranges (IQR). Point estimates (p-values) and interval estimates (95% confidence intervals [CIs]) for the proportion of patients who met the criteria for sepsis and the prevalence of sepsis were calculated. The Mann-Whitney U test was used to examine whether there was a significant difference in the underlying age distributions of ED patients with and without sepsis, and whether there was a significant difference in the age distributions of the male and female patients who met the criteria for sepsis. The chi-squared test was used to examine whether gender and sepsis status were independent.
A p-value of less than 0.05 was considered statistically significant. Analyses were performed using Microsoft Excel and Statistical Package for the Social Sciences (SPSS) version 21.0 (IBM, 2012).
Results
Patients who met the criteria for uncomplicated sepsis
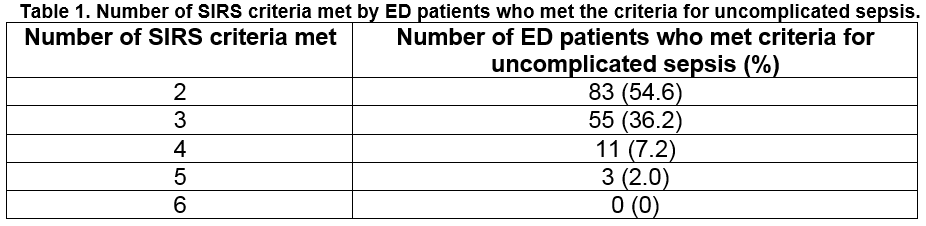
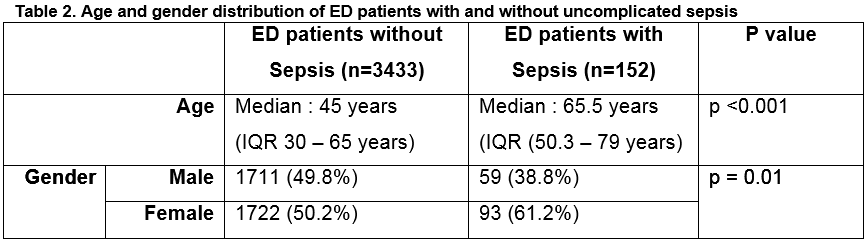
Overall, 152 of 3585 ED patients met the criteria for uncomplicated sepsis which represents 42.4 patients with uncomplicated sepsis per 1000 ED attendances or 4.24% (95% CI 3.57 - 4.91. Table 1 shows the number of SIRS criteria met by ED patients who met the criteria for uncomplicated sepsis. There was a significant difference in the age distributions of ED patients with sepsis and those without sepsis (p<0.001; Table 2); patients who met the criteria for sepsis were on average older than those who did not. There was also a significant difference in the gender distributions of ED patients with and without sepsis (p=0.01); 61.2% of patients with sepsis were female whereas 50.2% of patients without sepsis were female (Table 2). There was no statistically significant difference between the underlying age distributions of the male and female patients who met the criteria for sepsis at the 5% significance level (p=0.08).
Regarding the SIRS clinical features, the median heart rate was 104 beats per minute (IQR = 89-113 beats per minute), the median respiratory rate was 18 breaths per minute (IQR = 16-20 breaths per minute) and the median temperature was 36.7°C (IQR = 36-38°C). Twenty–two patients (14.5%) who met the criteria for uncomplicated sepsis had an altered mental status. The median blood glucose was 7.6 mmol/L (IQR = 6-9 mmol/L) and the median white cell count was 14.5 x 109/μl (IQR = 12-17.5 x 109/μl).
Suspected Source of Sepsis
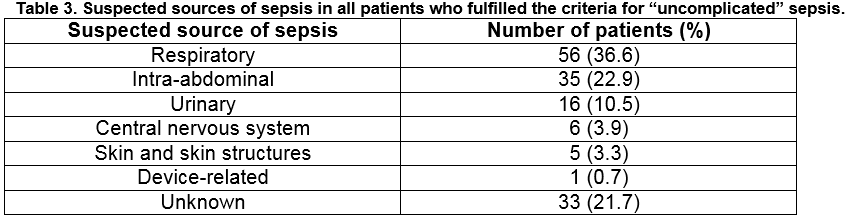
The most common suspected sources of sepsis were respiratory and intra-abdominal (Table 3).
Patients transferred to the intensive care unit (ICU)
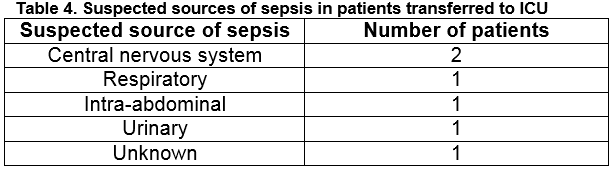
Six patients with uncomplicated sepsis and a median age of 60 (IQR = 46.5-77.8 years, range 42-80 years) were transferred to the ICU for further management. The suspected sources of sepsis in these patients are outlined in Table 4.
Discussion
There is currently no published study on the epidemiology of sepsis in the Irish ED setting. The primary aim of this study was to determine the proportion of ED patients who met the criteria for uncomplicated sepsis in an Irish hospital. We found that the proportion of ED patients who met the criteria for uncomplicated sepsis is 4.24% (95% CI 3.57-4.91or 42.4 sepsis patients per 1,000 ED attendances. Our study of 3585 patients is more than three times the number of patients required to estimate the prevalence of sepsis in the ED with 95% confidence and allowing for a 3% margin of error (1,067 patients). However, given that all the clinical measures required to diagnose sepsis had not been recorded for each patient, it is possible that our study reports a slight underestimation of ED sepsis prevalence. Of the 152 patients who met the criteria for uncomplicated sepsis, for example, 8.6% of the SIRS criteria were unavailable, of which capillary glucose was the most common missing SIRS criterion (6.3%). Approximately 12% of ED patients with sepsis develop shock within 48 hours of presentation, and of these more than half develop shock after the first 4 hours of ED arrival6.
ED patients with uncomplicated sepsis have a reported crude in-hospital mortality rate of 4.1%7. As many patients admitted to the ICU with sepsis are referred from the ED3, the ED plays a central role in the early identification of patients with sepsis, followed by risk stratification for severe sepsis and septic shock, initiating resuscitation and treatment, and ensuring the correct onward management of patients identified with sepsis. Despite this key role, only two studies have investigated the ED epidemiology of uncomplicated sepsis7,8. A UK teaching hospital ED study reported that 2.1% (123/5,832) of ED patients met the criteria for uncomplicated sepsis6, which is lower than found in our study. Meanwhile, a UK district general hospital ED study reported that 4.3% (95% CI 3.3-5.2%) of ED patients presented with sepsis8, which is similar to what we have found. In contrast to our study, the latter study was conducted over two one-week periods, six months apart8.
There is increasing interest in gender dimorphism in sepsis9. In general, males have a higher risk of developing sepsis than females, regardless of age9. However, we report a significantly higher proportion of females who met the criteria for sepsis. We found that although more females than males met the criteria for sepsis, the age distributions were similar (i.e. the results were not skewed due to a relatively larger number of elderly female patients). In the UK teaching hospital ED study, 65% of the patients with uncomplicated sepsis were males7; in the UK district general hospital ED study, more females (53%) than males (47%) met the criteria for uncomplicated sepsis8. Therefore, there seems to be an inconsistent relationship in terms of gender differences in patients with uncomplicated sepsis. We hypothesise that gender differences in this patient cohort may be due to differences in the characteristics of the local patient population within the ED catchment area or the study populations in the published literature.
An international task force recently published new definitions for sepsis10. However most of the data used to derive these new definitions were extracted from patient databases in hospitals in the United States (US), and have not been prospectively validated anywhere10. This study employed the current ED screening tool for sepsis recommended by the HSE5. The findings are hypothesis-generating (e.g., the identified gender difference in the proportion of patients who met the criteria for sepsis) and these could form the basis for future studies to investigate the pathobiology of sepsis.
This study has some limitations. Firstly, we used the original four SIRS criteria (heart rate > 90 beats per minute; respiratory rate > 20 breaths per minute; temperature <36°C or >38.3°C; white cell count <4000/μl or >12000/μl), in addition to suspicion of infection, for case finding as recommended by the national guideline. However, the SIRS criteria lack specificity for the diagnosis of sepsis in the ED setting because infections account for only a quarter of adult SIRS patients11. Secondly, our case finding was based on the clinical record documentation of a history suggestive of an infection. Therefore, any misdiagnoses by clinicians would alter the reported prevalence figures. However, by using this method we have enhanced the external validity of the study because it is reflective of actual clinical practice. Other commonly used methods of case finding patients with suspected or presumed infection in the published literature on sepsis include identifying patients who received antibiotics or identifying patients who underwent body fluid cultures12. However, a major limitation of these case finding methods is that there are certainly ED patients who are subsequently diagnosed with an infection who may not have had body fluid cultures performed in the ED or who may not have received antibiotics in the ED, and there are other ED patients without infection who receive antibiotics or undergo body fluid cultures in the ED. Thirdly, the approach we used to identify patients who met the criteria for “‘uncomplicated” sepsis (the six general variables) is just one of a suite of three approaches recommended to identify sepsis in patients with infection, namely: the six general SIRS criteria; at risk of neutropenia; and at risk of immunosuppression. It is possible that by using only one of these approaches, our study reports an underestimation of ED sepsis prevalence. Fourthly, as cross-sectional studies only provide a snapshot of the disease prevalence at a given point in time, it is possible that the ED prevalence of sepsis may be different if it were measured during another time frame (e.g., during a winter month) or over a longer time frame.
This study found that the proportion of patients in an Irish ED who met the criteria for uncomplicated sepsis was 4.24% (95% CI 3.59-4.94) which is similar to that recently reported in the UK. This finding translates to approximately one in every 25 patients attending the ED meeting the criteria for uncomplicated sepsis. Integration of sepsis recognition and resuscitation pathways into existing care escalation pathways will be critical to ensure rapid recognition and resuscitation of ED patients presenting with sepsis.
Correspondence
Dr. Abel Wakai, Emergency Care Research Unit (ECRU), Division of Population Health Sciences, Royal College of Surgeons in Ireland, 123 St. Stephen's Green, Dublin 2
Email: [email protected]
Phone: +353 1 402 2304/06
Fax: +353 1 402 2764
Acknowledgements
The data presented here are as a result of a valuable collaborative process between the ED administrative staff, hospital information and communications technology (ICT) staff, ED nursing staff and ED medical staff in Beaumont Hospital, and the RCSI Undergraduate Research Summer School 2015 Grant programme. We thank them for their help and contribution.
Conflicts of Interest:
The authors have no conflict of interest.
References
1. Bone RC. The sepsis syndrome. Definition and general approach to management. Clin Chest Med 1996;17:175-81
2. National Clinical Effectiveness Committee (NCEC). Sepsis Management. National Clinical Guideline No. 6, November 2014 [cited 2015 July 27]. Available from: http://www.hse.ie/eng/about/Who/clinical/natclinprog/sepsis/sepsis%20management.pdf
3. McIntyre LA, Fergusson D, Cook DJ, Nair RC, Bell D, Dhingra V, Hutton B, Magder S Hérbert PC. Canadian Critical Care Trials Group. Resuscitating patients with early severe sepsis: a Canadian multicentre observational study. Can J Anaesth 2007; 54(10)790-8.
4. Glickman SW, Cairns CB, Otero RM, Woods CW, Tsalik EL, Langley RJ, van Velkinburgh JC, Park LP, Glickman LT, Fowler VG Jr, Kingsmore SF, Rivers EP. Disease progression in haemodynamically stable patients presenting to the emergency department with sepsis. Acad Emerg Med 2010;17(4):383-90.
5. Health Service Executive (HSE). Sepsis. 2013. [Cited 5 August 2015] Available from: http://www.hse.ie/eng/about/Who/clinical/natclinprog/sepsis/Emergency%20Department%20Adult%20Sepsis%20Pathway.pdf
6. Capp R, Horton CL, Takhar SS, Ginde AA, Peak DA, Zane R, Marill KA. Predictors of patients who present to the emergency department with sepsis and progress to septic shock between 4 and 48 hours of emergency department arrival. Crit Care Med 2015; 435:983-8.
7. Majuran M, Clancy M. Determination of the size of the different sepsis categories presenting to a UK teaching hospital emergency department. Emerg Med J 2008; 25:11-14.
8. Cowan SL, Holland JA, Kane AD, Frost I, Boyle AA. The burden of sepsis in the emergency department: an observational snapshot. Eur J Emerg Med 2015; 22:363-365.
9. Angele MK, Pratschke S, Hubbard WJ, Chaudry IH. Gender differences in sepsis. Virulence 2014; 5:12-19.
10. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016;315(8):801 doi:10.1001/jama.2016.0287
11. Horeckzko T, Green JP, Panacek EA. Epidemiology of the systemic inflammatory response syndrome (SIRS) in the emergency department West J Emerg Med 2014;15(3):329-36
12. Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, Rubenfeld G, Kahn JM, Shankar-Hari M, Singer M, Deutschman CS, Escobar GJ, Angus DC. Assessment of clinical criteria for sepsis: for the third international consensus definitions of sepsis and septic shock (Sepsis-3) JAMA. doi: 10.1001/jama.2016.0288.
p435