A Comparison of Summer and Winter Emergency Hospitalisations in Ireland
J. Mulroe, F. Donohue, P.M. Kavanagh, S. McCarthy, H. Johnson
Health Intelligence, Strategic Planning & Transformation Health Service Executive
Abstract
There is increasing demand on the Irish health service, particularly in winter months. This study described and compared acute hospitals admissions across summer and winter periods from 2015 to 2018. The analysis used Hospital In-Patient Enquiry data accessed through the National Quality Assurance Information System – NQAIS Clinical. There were 84 additional emergency hospitalisations in winter per week compared with summer (1.2% increase). Across diagnostic categories, emergency hospitalisations reduced in winter, except respiratory conditions which increased by 379 per week representing a 40.5% increase. The profile of emergency respiratory admissions were similar in summer and winter in terms of age, length of stay, day of week and medical card status. Length of stay was approximately one day longer for weekend admissions in both seasons. This research highlights the importance of taking a whole-population approach to winter resilience planning, focussing on prevention and optimal management of respiratory conditions.
Introduction
The life expectancy of the Irish population has improved over recent decades. This ageing population coupled with an increased prevalence of chronic disease places an increasing demand on health services as outlined in The Health Services Capacity Review.1
The configuration of the Irish health system, which is characterised by hospital-centricity and weak orientation to primary and community care, is poorly placed to respond safely, effectively and efficiently to evolving population health needs.2 The recent financial crisis has impacted the resilience and capacity of health services.3 The current health system is challenged with high bed occupancy, trolley waits and waiting lists. Slaintecare has identified a need to grow capacity and shift the balance of care from hospitals to primary and community care so as to deliver timely access to health and social care.4
The strain on health system resilience is especially evident during winter months with the highest level of emergency admissions in December.5 The Health Service Executive (HSE) produces a plan each winter to address bed capacity, focusing on such issues as demand management, increasing throughput and better facilitating egress, and thereby keeping as many people as well as possible, improving patient’s access to the right care in the right place at the right time, and reducing the numbers of patients waiting to be discharged from hospital.6
While excess winter mortality is relatively well-studied, epidemiological characterisation of increased demand for health services in winter is needed to better inform planning and resilience. In the UK the winter increase in respiratory diseases has been identified as causing considerable pressure on the healthcare system, with almost a doubling of non-elective admissions in this disease group.7,8 The impact of a drop in temperature has been characterised such that for every degree drop in temperature below 5C, there is a subsequent 0.8% increase in respiratory admissions in the following weeks.9 A British Thoracic society study reported up to 40% of patients admitted with community acquired pneumonia were classified as low severity suggesting a proportion might have been suitable for treatment at home.10 Re-admission rates in the UK are reported to be high for those with chronic obstructive pulmonary disease (COPD) where they have been found to be 24% at 30 days.11 Strengthening services such as access to ambulatory emergency care, early supported discharges, rapid access respiratory clinics and alternative use of elective capacity are areas identified which may alleviate the pressure caused by this winter surge.12
The purpose of the study was to describe the underlying patterns of admission across summer and winter periods and to identify patient groups that might explain the surge in emergency admissions during winter months.
Methods
This study was undertaken using National Quality Assurance Information System (NQAIS) which provides online feedback to clinicians and managers using the hospitals’ own hospital in-patient enquiry (HIPE) data.13
HIPE data originates from the publicly funded acute hospitals. The data is collated and quality assured by the Healthcare Pricing Office (HPO) on a national basis.5 The database includes the patient’s age, gender, admission type, and date of admission and discharge, the principle diagnosis and up to 20 other diagnoses (International Classification of Diseases Tenth Revision (ICD-10-AM)14 The admission/principle diagnosis was used to classify the diagnostic category based on the Clinical Classification System (Irish modification). Data relating to adult in-patient emergency admissions to acute hospitals in Ireland from 2015-2018 was included. Patients aged less than 16 years, maternity, day cases and elective admissions were excluded.
Summer was defined as May-August (week 18-35) and winter as November-February (week 44 to week 9). The data was averaged across the three year period when appropriate. Length of stay was calculated using the arithmetic mean. The Charlson Index was used to categorise patient’s co-morbidities based on the International Classification of Diseases (ICD) diagnosis codes.15 A score of 10 or more was categorised as high complexity.16 The characteristics of patients admitted in both seasons were compared using the Chi-square test and Fisher’s Exact test as appropriate.
Results
Seasonal variation in all emergency admissions
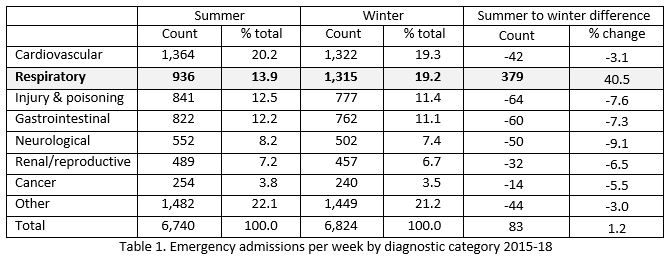
Over the previous three winters (2015-18) there was an average of 6,824 emergency admissions nationally per week compared with an average of 6,740 admissions per week in the summer; an additional 84 (1.2%) emergency admissions per week nationally in the winter. The average length of stay was similar in summer and winter. (6.5 days in summer, 6.8 days in winter)
Respiratory, cardiovascular disease (CVD), renal/reproductive disease, injury/poisoning, cancer, neurological and gastrointestinal illnesses account for 78.6% (831,918/1,057,926) of emergency admissions annually. The seasonal trend for these conditions over the past 3 years is illustrated in Table 1. There was an increase in respiratory admissions during the winter months whereas a decrease in admissions was observed in all other diagnostic categories (7df, Chi Sq 73.0, p<0.0001).
 Seasonal variation in respiratory emergency admissions
Seasonal variation in respiratory emergency admissions
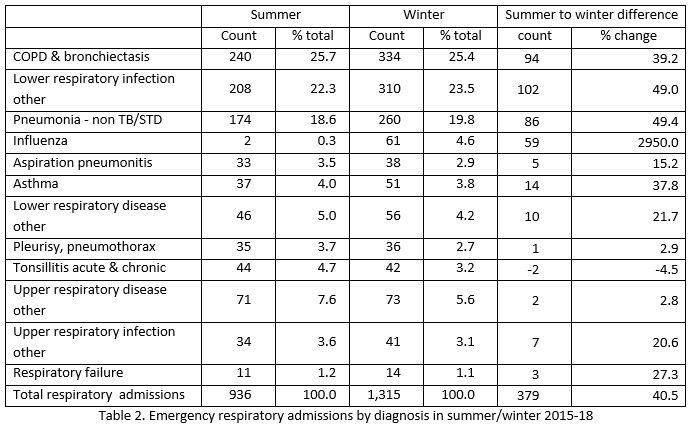
Nationally, over the three year period, an additional 379 respiratory admissions were observed in winter per week; a relative increase of 40.5% in winter compared to summer. The increase in respiratory admissions was observed in all hospitals and hospital groups.
The majority (67.8%) of emergency respiratory admissions were due to chronic obstructive pulmonary disease (COPD), lower respiratory infection and pneumonia. Albeit a higher incidence of cases was observed in the winter, the proportion in each diagnostic subgroup was similar in both seasons as shown in Table 2. During the summer months an average of two influenza admissions per week occurred compared to 61 per week in winter.
 Socio-demographic and clinical profile of respiratory admissions
Socio-demographic and clinical profile of respiratory admissions
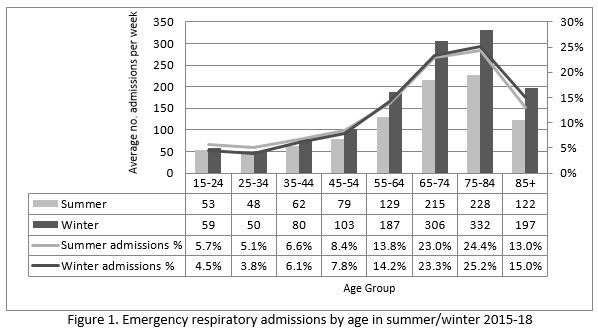
The age profile of patients admitted as an emergency with respiratory illness was similar in summer and winter. The number of admissions was greater in those aged over 55 years with the peak occurring in the 75-84 year age group in both seasons as shown in Figure 1. The proportion of patients with a medical card was similar in summer and winter at 74% and 75% respectively.
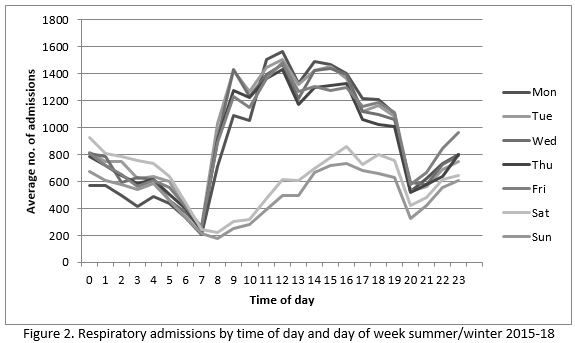
 Average length of stay (LOS) for respiratory admissions was longer in winter (7.4 days in winter versus 6.7 days in summer). The average LOS was longer for those admitted on weekends; this pattern was similar in both seasons with the difference in a weekday versus weekend LOS being 0.9 days in summer and 1.2 days in winter.
Average length of stay (LOS) for respiratory admissions was longer in winter (7.4 days in winter versus 6.7 days in summer). The average LOS was longer for those admitted on weekends; this pattern was similar in both seasons with the difference in a weekday versus weekend LOS being 0.9 days in summer and 1.2 days in winter.
The pattern of respiratory admissions by the day of the week was similar throughout the year, being consistently lowest on Saturday and Sunday. There majority were documented to take place between 8am and 7pm, peaking in the early afternoon (Figure 2).
Co-morbidities were described using the Charlson score. The majority of patients (79.3%) had a Charlson score of less than 10 during both seasons. However, in winter a slightly higher proportion had a score above 10 compared to summer (21.4% versus 18.5% respectively, p<0.001, OR 1.22 95% CI 1.62-1.28).
In terms of readmissions 4.7% of patients were readmitted within 7 days during winter compared with 5.1% in summer. (p=0.065, OR 0.92, 95% CI 0.84-1.01) The readmission rate after 30 days was 13.6% in winter compared with 13.8% in summer. (p=0.53. OR 0.98, 95% CI 0.93-1.04).
The crude mortality rate of patients admitted as an emergency with respiratory illness was slightly higher in winter at 6.1% versus 5.3% in summer although the difference was not statistically significant. (OR 1.17, 95% CI 0.81-1.70, p=0.39).
Discussion
This study has characterised the seasonal epidemiology of hospital admissions in adults in Ireland 2015-2018. Importantly, it has identified that respiratory illness was the dominant driver of increased emergency admissions during the winter season across the entire acute hospital service. Over the last three winters there was a relative increase of 40.5% emergency respiratory admissions nationally. Data from the Towards a Revolution in COPD Health (TORCH) study found a two-fold increase in COPD exacerbations during winter with approximately 20% of these people requiring hospitalisation regardless of season.17 In the UK an 80% increase in lung disease was reported in winter but this included children.18
The profile of emergency respiratory admissions in terms of age, length of stay, day of week, time of day, admission source, and discharge destination were similar in summer and winter. The proportion of patients with a medical card was the same in both seasons. The evidence in terms of the impact of deprivation on respiratory admissions is mixed. Some studies report that social deprivation did not impact respiratory admissions but a diagnosis of COPD was the principle driver as well as social isolation8 whereas other studies found an association between deprivation and respiratory admissions.19 The majority of respiratory admissions (60%) were aged over 65 years. Admissions on weekend days were associated with a longer length of stay during both seasons.
Chronic obstructive pulmonary disease, pneumonia and lower respiratory tract infections were the most common causes of emergency respiratory admissions in both summer and winter. This finding suggests that the winter surge of acute respiratory admissions to hospital is triggered through a common pathway most likely to be of infective origin (viral, bacterial or both). Air quality and extremes of air temperature can also exacerbate respiratory illness in particular COPD.20,21
There are commonalities associated with prevention and treatment of acute respiratory conditions which can be strengthened through active, planned chronic disease case management and self-management support in line with care pathways and models of care.22 The provision of ambulatory emergency care, rapid access clinics, and early supported discharges may help to alleviate the pressure on the health system.8,12 Self-management support should be optimised including access to pulmonary rehabilitation services and smoking cessation services.23 This could be supported with implementation of the “Making Every Contact Count” framework offering brief advice and interventions to patients in terms of their lifestyle risk factors.22 The uptake of influenza and pneumococcal vaccination should be optimised. There was a marked improvement in influenza vaccine uptake among health care workers in recent years but uptake among those aged over 65 years has decreased in recent years.24
The HSE winter plan6 and Slaintecare reports4 outline the importance of providing the right care in the right setting at the right time for patients. This research indicates that the prevention and management of respiratory illness in the community setting require special attention so as to minimise the winter surge in emergency admissions. The National Healthcare Quality Reporting system supports the need for attention to this area outlining that COPD admissions remain high although they have slightly reduced since 2008.24In the UK a respiratory taskforce has been established to bring an increased level of attention and organisation to respiratory illness.8
This study concludes that the increase in emergency hospital admissions during winter was explained by a marked seasonal increase in respiratory illness, primarily chronic obstructive pulmonary disease, pneumonia and lower respiratory tract infection. The demographic and clinical profile of patients with acute respiratory illness was broadly similar in summer and winter. The findings of this study imply that the winter initiative should have a strong and purposeful focus on the prevention and management of acute respiratory illness both in the community and in hospitals so as to minimise the winter surge in emergency admissions. The lessons learned may translate to all seasons.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Corresponding Author
Jacinta Mulroe
Specialist Registrar
Health Intelligence Unit
Dr. Steevens Hospital
Steevens Lane
Dublin 8
D08 W2A8
Tel: 086-4016638
Email: [email protected]
References
1. Health Service Capacity Review - review of health demand and capacity requirements in Ireland to 2031. Department of Health. Available from: https://health.gov.ie/wp-content/uploads/2018/02/71580-DoH-Dublin-Report-v6.pdf
2. European Observatory on Health Systems. Health system responses to financial pressures in Ireland - Policy options in an international context. Copenhagen: WHO Regional Office for Europe; 2014. Available from: http://www.euro.who.int/__data/assets/pdf_file/0006/260088/Health-system-responses-to-financial-pressures-in-Ireland.pdf
3. Thomas S, Keegan C, Barry S, Layte R, Jowett M, Normand C. A framework for assessing health system resilience in an economic crisis: Ireland as a test case. BMC Health Services Research. [journal article]. 2013 October 30;13(1):450.
4. Committee on the Future of Healthcare - Sláintecare Report. Department of Health. May 2017. Available from: http://data.oireachtas.ie/ie/oireachtas/committee/dail/32/committee_on_the_future_of_healthcare/reports/2017/2017-05-30_slaintecare-report_en.pdf
5. Healthcare Pricing Office (2016) Activity in Acute Public Hospitals in Ireland - Annual Report, 2015 Dublin. Health Service Executive.
6. HSE Draft Winter Plan 2017-2018. Available from: https://www.hse.ie/eng/about/who/acute-hospitals-division/special-delivery-unit/the-winter-plan-2017-2018.pdf
7. The Royal College of Emergency Medicine (2016). Why does winter in A&E get worse every year? Available from: https://www.rcem.ac.uk/docs/Policy/Why%20does%20winter%20in%20A+E%20get%20worse%20every%20year.pdf
8. Jordan RE, Hawker JI, Ayres JG, Adab P, Tunnicliffe W, Olowokure B, Kai J, McManus RJ, Cheng KK. Effect of social factors on winter hospital admission for respiratory disease: a case-control study of older people in the UK. The British Journal Of General Practice: The Journal Of The Royal College Of General Practitioners. 2008;58(551):400-2.
9. Chalabi Z, Erens B, Hajat S, Heffernan C, Jones L, Mays N, Ritchie B, Wilkinson P (2012) Evaluation of the implementation and health-related impacts of the cold weather plan for England. Policy Innovation Research Unit.
10. Daniel P, Bewick T, WelhamS, Lim WS (2015) Adult community-acquired pneumonia audit report. British Thoracic Society.
11. Stone RA, Holzhauer‐Barrie J, Lowe D, McMillan V, Saleem Khan M, Searle L, Skipper E, Welham S, Roberts CM (on behalf of the National COPD Audit Programme: secondary care workstream) (2015) COPD: Who cares matters. National Chronic Obstructive Pulmonary Disease (COPD) Audit Programme: Clinical audit of COPD exacerbations admitted to acute units in England and Wales 2014.
12. National Health Service (NHS) - British Thoracic Society. Quick guide: planning for increased seasonal demand in respiratory illness. London: NHS England and NHS Improvement; 2017. Available from: https://www.brit-thoracic.org.uk/document-library/working-in-respiratory/working-in-respiratory-documents/quick-guide-planning-for-increased-seasonal-demand-in-respiratory-illness/
13. NQAIS Clinical. Available from: https://nqaisclinical.healthatlasireland.ie/myfolders.html?view=NQAISClinical
14. National Centre for Classification in Health (NCCH), 2013: The International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification(8thEd): NCCH, Australian Health Services Research Institute, The University of Wollongong.
15. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal Of Chronic Diseases. 1987;40(5):373-83.
16. Dr Foster Intelligence (2014) Understanding HSMRs : A Toolkit on Hospital Standardised Mortality Ratios, Version 9, London. Available at: http://www.drfoster.com/about-us/our-approach/metrics-methodologies-and-models-library.
17. Jenkins CR, Celli B, Anderson JA, Ferguson GT, Jones PW, Vestbo J, Yates JC, Calverley PM. Seasonality and determinants of moderate and severe COPD exacerbations in the TORCH study Eur Respir J. 2012 Jan; 39(1):38-45.
18. British Lung Foundation. Out in the cold: lung disease, the hidden driver of NHS winter pressure. 2017. Available from: https://www.blf.org.uk/policy/out-in-the-cold
19. McAllister DA, Morling JR, Fischbacher CM, MacNee W, Wild SH. Socioeconomic deprivation increases the effect of winter on admissions to hospital with COPD: retrospective analysis of 10 years of national hospitalisation data. Prim Care Respir J. 2013;22(3):296–299.
20. Clancy L, Goodman P, Sinclair H, Dockery DW. Effect of air-pollution control on death rates in Dublin, Ireland: an intervention study. Lancet (London, England). 2002;360(9341):1210-4.
21. Hansel NN, McCormack MC, Kim V. The Effects of Air Pollution and Temperature on COPD. COPD. 2015;13(3):372-9.
22. Health Service Executive (2016). Making Every Contact Count: A Health Behaviour Change Framework and Implementation Plan for Health Professionals in the Irish Health Service. Health Service Executive. Available from: https://www.hse.ie/eng/about/who/healthwellbeing/making-every-contact-count/making-every-contact-count-framework.pdf.
23. Health Service Executive (2017). National Framework and implementation Plan for Self-management Support for Chronic Conditions: COPD, Asthma, Diabetes and Cardiovascular Disease. Available from: https://www.hse.ie/eng/health/hl/selfmanagement/hse-self-management-support-final-document1.pdf.
24. Department of Health. National Healthcare Quality Reporting System Annual Report. Dublin: 2018. Available from: https://health.gov.ie/wp-content/uploads/2018/07/2018-NHQRS-Report-1.pdf
P935
