A Descriptive Study of Antidepressant Prescribing In a Semi-Rural Practice
M Walsh, I Duffy
Swanpark Surgery, Monaghan
Abstract
Aims
Mental health conditions are increasingly encountered in general practice. The aim of this study was to review the antidepressant prescribing of this practice.
Methods
Health One analysis was used to search for patients prescribed antidepressants in the last 6 months and to generate a list of their antidepressant prescriptions over the last three years. Charts were reviewed to determine if these patients were reviewed by a GP in the last 6 months, and by psychiatry in the last year.
Results
Six hundred and two patients (7% of the practice adult population) were prescribed antidepressants in the last 6 months. Fifty-four percent (n=324) of patients have been on antidepressants for three years or more. Escitalopram was most frequently prescribed. 89% (n=535) were reviewed by a GP in the last 6 months, and 21% (n=127) were reviewed by psychiatry services in the last year.
Discussion
The majority of patients with mental health problems are being managed in primary care.
Introduction
Depression is an increasingly common condition, affecting more than 450,000 people in Ireland (1 in 10) at any one time1. It is estimated than 1 in 9 people will suffer a primary anxiety disorder over their lifetime2. According to the World Health Organisation (WHO), depression is now the leading cause of disability globally3. Mental health problems account for up to 30% of consultations with general practitioners in Europe3. The majority of patients with mood and anxiety disorders can be treated effectively in primary care4.
The National Institute for Health and Care Excellence (NICE) advises a stepped care approach to the management of mental health problems, ranging from support, psychoeducation and active monitoring to medication and psychological interventions, to crisis services and inpatient care. Along with psychological therapies, antidepressants should be offered to patients with moderate or severe depression, while for patients with mild depression, antidepressants should be considered where symptoms are persistent or unresponsive to psychological therapies alone. For patients with anxiety disorders, antidepressants should be offered to those whose symptoms have not responded adequately to psychological intervention alone, and to those who have marked functional impairment5.
Due to long waiting lists and the lack of access to counselling and psychological therapies, medication often dominates as the main or only treatment option offered in primary care6. The HSE has acknowledged that there are significant gaps in provision and access to psychological therapies in Ireland with an over reliance on medication7. Antidepressant prescribing has soared in recent years. In 2012, the state spent 40 million euro on 2.3 million prescriptions for the top 5 medications used to treat anxiety and depression, for 330,000 patients8. Selective serotonin reuptake inhibitors (SSRIs) are recommended first line, due to their favourable risk-benefit ratio, followed by dual acting serotonin noradrenaline reuptake inhibitors (SNRIs) and noradrenergic and specific serotonergic antidepressants (NaSSAs)4,5. All patients should have documented follow-up4.
Methods
Using Health One Analysis, the patient database was searched for all adult patients prescribed SSRI/SNRI/NaSSAs in the three years between 1st April 2014 and 31st March 2017. The database was again searched for all adult patients prescribed the relevant antidepressants in the 6 months between 1st October 2016 and 31st March 2017, and a list of their antidepressant prescriptions over the last three years was generated. These prescriptions were analysed for current treatment, duration of treatment, and number of different antidepressants prescribed over the last three years. A further Health One analysis was conducted to determine if these patients had a prescription issued within a consultation in the last 6 months. Chart reviews were conducted to determine if these patients were reviewed by a GP in the last 6 months, and if they were reviewed by psychiatry in the last year. The data was analysed using Microsoft Excel.
Results
Nine hundred and seventy-seven patients were prescribed antidepressants in the last three years,12% of the practice adult population. Six hundred and two patients were prescribed antidepressants in the last 6 months, 7% of the practice adult population.
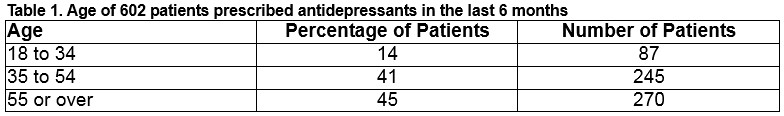
Gender & Age
Sixty-four percent (n=384) of patients are male, 36% (n=218) are female. Fourteen percent (n=87) are aged between 18 and 34, 41% (n=245) are aged between 35 and 54, and 45% (n=270) are aged 55 or over.
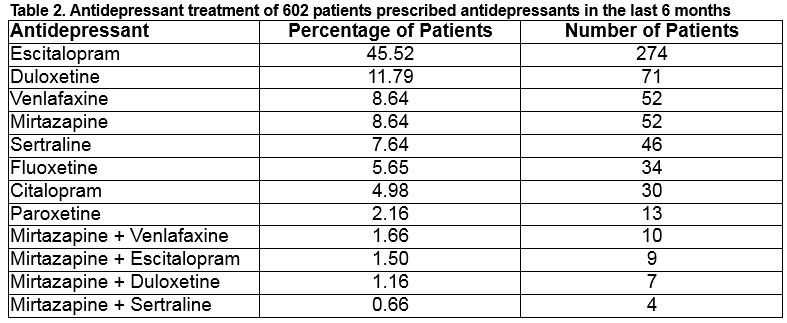
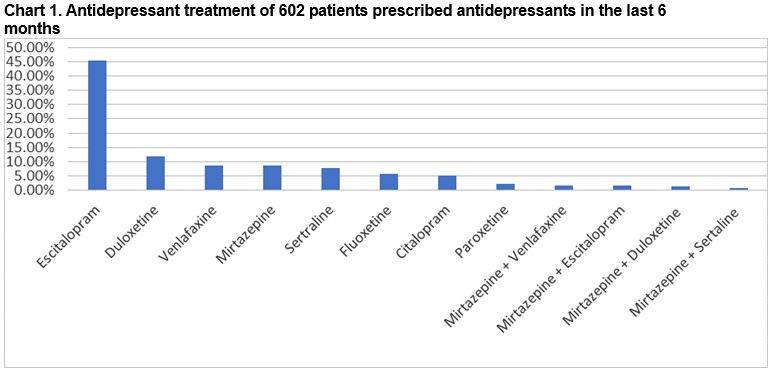
Antidepressant Treatment
Over 95% are on monotherapy, less than 5% are on dual antidepressant therapy as outlined in Table 2 and Chart 1.
Number of antidepressants
Seventy-eight percent (n=472) were prescribed one antidepressant in the last three years, 17% (n=101) were prescribed two antidepressants, 4% (n=24) were prescribed three antidepressants, less than 1% were prescribed four (n=4) or 5 antidepressants (n=1).
Duration of treatment
Twelve percent (n=71) have been on treatment for less than 6 months, 6% (n=39) for 6 to 12 months, 15% (n=88) for one to two years, 13% (n=80) for two to three years, and 54% (n=324) for 3 years or more.
Prescriptions within a consultation
Fifty-four percent (n=326) had a prescription issued within a consultation in the last 6 months.
Reviews by a GP in the last 6 months
Eighty-nine percent (n=535) were reviewed by a GP in the last 6 months, 10 of these were by phone only.
Referrals to psychiatry
Twenty-one percent (n=127) were reviewed by psychiatry services in the last year. Twenty-four of these (19%) were new referrals.
Discussion
Antidepressant prescribing is more prevalent in the older age group. Older patients are at higher risk of adverse effects due to the presence of physical comorbidities and potential drug interactions. Suitable antidepressants should be prescribed at an age appropriate dose, taking these factors into account5. More women are believed to be affected by depression than men3. However, nearly two thirds of the antidepressant prescriptions in this practice are issued to men. Of note, there is a higher male population in this practice; 53% of the patients are male and 47% are female.
Escitalopram is by far the most commonly prescribed antidepressant, accounting for almost half of prescriptions. The second most commonly prescribed is duloxetine, followed by venlafaxine and mirtazapine. Nationally, escitalopram, followed by citalopram is the most frequently prescribed SSRI, and venlafaxine is the most frequently prescribed SNRI8. Reasons for choosing a particular antidepressant may include prescriber factors (experience, up to date with current guidelines), practice culture, or patient factors (age, comorbidities, potential interactions, pregnancy or breastfeeding, patient experience or preference, and cost). Under the Medicines Management Programme, based on safety, efficacy and cost-effectiveness, citalopram is the preferred SSRI, and venlafaxine is the preferred SNRI9. In a meta-analysis comparing 12 new generation antidepressants, escitalopram, sertraline, venlafaxine & mirtazapine were significantly more efficacious than duloxetine, fluoxetine & paroxetine10. Escitalopram & sertraline showed the best profile of acceptability, leading to significantly lower discontinuations than did duloxetine, venlafaxine, and paroxetine. NICE guidelines advise using sertraline or citalopram for those with co-existing chronic physical disease, as they have a lower propensity for interactions5. Sertraline is recommended for patients with ischaemic heart disease4. Fluoxetine has the most data for safety in pregnancy, while sertraline is believed to be the safest in breastfeeding11. QT prolongation and torsade de pointes are reported more frequently with citalopram and escitalopram12. The ICGP guidelines advise consideration of dual acting SNRIs/NoSSAs if there is failure to respond to two SSRIs13. The potential for higher doses of venlafaxine to exacerbate cardiac arrhythmias and the possibility of exacerbation of hypertension with venlafaxine and duloxetine, should be carefully considered. Mirtazapine may be particularly beneficial for patients whose sleep and appetite are severely affected.
The majority of patients have been on a single antidepressant in the last 3 years. Switching to another antidepressant should be considered if there has been a poor response to treatment, only after first checking adherence and side effects, and considering increasing the dose4,5. The evidence for the relative advantage of switching either within or between classes is weak5. Less than 5% of patients are on a combination of two antidepressants. Combining antidepressant medications should only be started in primary care in consultation with a consultant psychiatrist5. Using a single antidepressant rather than combination or augmentation is associated with a lower side-effect burden5.
More than half of the patients appear to be taking antidepressants long-term. It is not known how many of these have been on continuous treatment, and how many have had gaps in treatment. Antidepressant treatment should be continued for at least 6 months after remission of depression, and at least two years in patients at risk of relapse (two previous episodes of depression or first episode after the age of 50)4,5. The Centers for Disease Control and Prevention (CDC) has reported that 60% of patients on antidepressants in the US had taken them for two years or longer, and 14% had taken them for more than a decade14. The need to continue antidepressants should be discussed with the patient, taking into account risk factors for relapse – age, comorbid conditions, number & severity of previous episodes of depression. Maintenance therapy has been shown to reduce the risk of relapse by at least 50%15. For patients with anxiety disorders, medication should be continued for 6 to 12 months before tapering to prevent relapse4,16. All patients should be advised that antidepressants should be withdrawn slowly following a gradual dose reduction over a period of at least 4 weeks5.
Sixty-seven patients were prescribed antidepressants in the last 6 months without review. In the initial months of antidepressant therapy, patients should be frequently reviewed, and thereafter should continue to be reviewed at longer intervals guided by response to treatment5. Ongoing review is important to continue to provide support, to assess response to treatment, to assess risk, and to review the treatment plan and duration of antidepressant therapy. It cannot be presumed that the 89% of patients who were reviewed in the last 6 months had their antidepressant therapy reviewed, however it is likely that the 54% of patients who were issued a prescription within a consultation had their antidepressant therapy reviewed. Improvements are needed in the monitoring of patients on antidepressants. Caution is required with repeat prescriptions. Patients should not receive prescriptions for longer than 6 months without a documented review.
One fifth of patients were reviewed by psychiatry services in the last year, though less than a fifth of these were new referrals. The majority of patients are being managed in general practice. Referral to specialist mental health services is indicated where there is a risk of harm or suicide, the presence of psychotic symptoms, or where multi-professional care or an expert opinion on treatment and management is needed4,5. The ICGP guidelines advise referring patients who fail to respond to treatment after 3 months13.
The antidepressant prescribing in this practice reflects the wide use of antidepressants in society. The majority of patients with mental health problems are being managed in general practice. We should be vigilant about repeat antidepressant prescribing and ensure that patients continue to be reviewed. Better documentation of mental health reviews and antidepressant medication reviews is needed.
Acknowledgements:
Thanks to Dr Niall Maguire, GP & Assistant Programme Director, Northeast GP Training Scheme, Navan, and Cathy McMahon, Practice Manager, Swanpark Surgery, Monaghan, for their assistance.
Conflict of interest:
There are no conflicts of interest.
Correspondence:
Maeve Walsh, Swanpark Surgery, Monaghan
Email: [email protected]
References
1. Aware: Depression Support. [Internet]. Ireland; 2016. Available from: https://www.aware.ie/about/
2. Anxiety: St Patrick's Mental Health Services [Internet]. Dublin; 2018. Available from: https://www.stpatricks.ie/mental-health/anxiety
3. Depression Fact Sheet. World Health Organisation [Internet]; 2018. Available from: http://www.who.int/en/news-room/fact-sheets/detail/depression
4. Irish College of General Practitioners, Health Service Executive. Guidelines for the Management of Depression and Anxiety Disorder in Primary Care; 2006
5. National Institute for Health and Care Excellence. Depression in Adults: Recognition and Management; updated April 2018
6. McDaid S. Mental Health in Primary Care in Ireland: A briefing paper. Mental Health Reform; 2013
7. Primary Care and Mental Health Group. Advancing the shared care approach between primary care & specialist mental health services. Naas: HSE; 2012
8. Primary Care Reimbursement Services Report. HSE; 2012
9. Medicines Management Programme: Preferred Drugs. SSRIs & SNRIs for the treatment of depression. HSE; 2014
10. Cipriani A, Furukawa TA, Salanti G, Gedded JR, Higgins JP, Churchill R, Watanabe N, Nakagawa A, Omori IM, McGuire H, Tansella M, Barbui C. Comparative efficacy and acceptability of 12 new generation antidepressants: a multiple treatments meta-analysis. Lancet 2009 Feb 28; 373(9665): 746-58
11. Taylor D, Paton C, Kapur S. The Maudsley Prescribing Guidelines in Psychiatry. Eleventh Edition 2012. 436, 449-450
12. Funk KA, Bostwick JR. A comparison of the risk of QT prolongation among SSRIs. Annals of Pharmacotherapy 2013 Oct; 47:1330-1341
13. Kelly M, Russell V. Referral of people with depression to specialist mental health services. ICGP Quality in Practice Committee; The College of Psychiatry of Ireland; 2011
14. Pratt LA, Brody JD, Gu Q. Antidepressant use in persons aged 12 and over: United States 2005-2008. NCHS Data Brief. 76; 2011
15. Spadone C. Treatment adherence in the recurrent depressive disorders. Encephale 2002 May-Jun;28(3 Pt 1):255-9
16. Locke AB, Kirst N, Schultz CG. Diagnosis and management of generalised anxiety disorder and panic disorder in adults. Am Fam Physician 2015 May 1;91(9):617-624
(P752)
