An Unusual Presentation of Sarcoidosis
Ú Lannin, J Hayes
Cavan General Hospital
Abstract
Bilateral pleural effusions are a rare manifestation of sarcoidosis. We describe here the case of a 30 year old Vietnamese man living in Ireland who presented with a 4 month history of cough, dyspnoea on exertion and fatigue. On chest CT, he was found to have bilateral pleural effusions, bihilar lymphadenopathy and multiple pulmonary nodules. Pleural biopsy confirmed the presence of non caseating granulomas. He was commenced on steroids with excellent clinical response.
Introduction
Sarcoidosis is a multisystem granulomatous disease of unknown aetiology. Pleural effusion is a rare manifestation of sarcoidosis with an estimated incidence of 1.1%1. Bilateral pleural effusions are even rarer.
Case report
The patient was a 30-year-old previously well Vietnamese gentleman who has been resident in Ireland for 10 years. He is a lifelong non-smoker and works as a chef. He presented to the medical assessment unit with a four-month history of cough productive of white sputum with intermittent haemoptysis and left sided pleuritic chest pain. He reported five kilogram weight loss in the preceding four-months He denied night sweats. He denied previous personal or contact history with tuberculosis. He did not take any regular medications. There was no significant family history reported. Physical examination found decreased breath sounds in both lung bases. Laboratory investigations revealed an elevated CRP 22. Full blood count, renal, liver and bone profile were normal. Interferon Gamma Release Assay and HIV screen was negative.
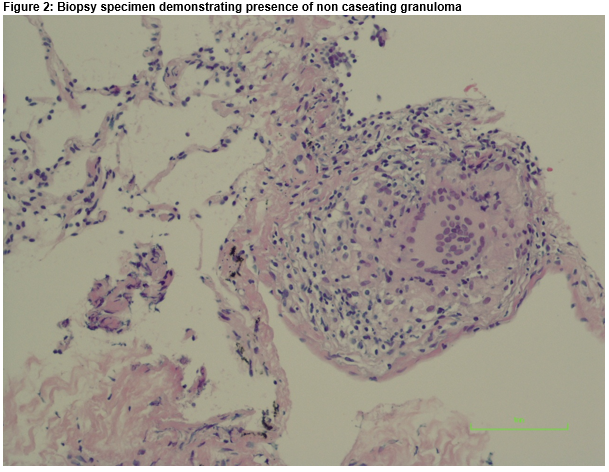
CXR revealed bilateral pleural effusion and bihilar lymphadenopathy. CT thorax showed multiple pulmonary nodules with mediastinal hilar and subcarinal lymphadenopathy, bilateral pleural effusion and left base consolidation (Fig. 1). Thoracocentesis demonstrated an exudative (protein 44g/dl), lymphocytic effusion. No acid fast bacilli or malignant cells were identified.
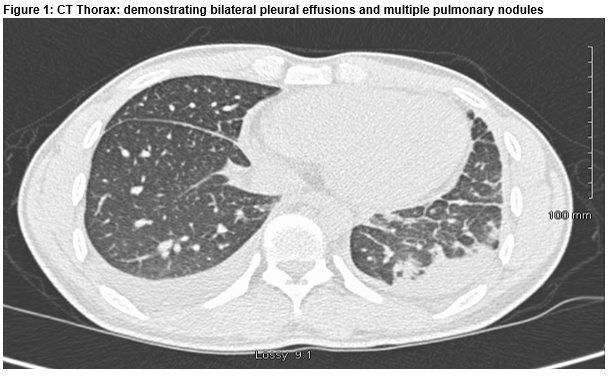
A provisional diagnosis of miliary TB was made based on the characteristic clinical and radiographic presentation, lymphocytic exudate and previous residence in an endemic area. He was commenced on standard anti tuberculous treatment. He was reviewed in clinic one month later. His symptoms had failed to improve and he was re-admitted for further investigations. He underwent CT guided lung and pleural biopsy. The specimens showed non caseating granulomas (Fig. 2). He was commenced on steroids. On review in clinic one month later he reported significant symptomatic improvement. Repeat chest radiograph showed complete resolution of the pleural effusions. He is currently completing a six-month tapering course of steroids.
Discussion
Sarcoidosis is a multisystem disorder characterised by the presence of non caseating granulomatous inflammation on biopsy. Pleural effusions are a rare manifestation of sarcoidosis1. There are a number of proposed mechanisms including increased capillary permeability secondary to pleural involvement, superior vena cava obstruction and lymphatic disruption2. These can occur at any radiographic disease stage but more commonly occur in Stage I and II. They are typically small to moderate in size and unilateral, with preponderance to the right side. Typically, the pleural fluid is exudative and lymphocytic predominant, similar to tuberculosis. There have also been case reports of haemothorax and chylothorax. There is often a high CD4/CD8 ratio and a low adenine deaminase3. Biopsy demonstrating non caseating granulomas is required to make a definitive diagnosis. Oral steroids are the standard treatment for sarcoid pleural effusions although some resolve spontaneously4. Pleural effusion secondary to sarcoidosis is a rare entity. It can be misdiagnosed as tuberculosis with consequent delay in appropriate therapy. This case confirms the value of CT guided pleural biopsy to determine the underlying aetiology of a pleural effusion.
Correspondence
Dr. Úna Lannin, Medical Registrar Cavan General Hospital
Email: [email protected]
Conflict of interest
No conflicts of interest to disclose.
References
1. Pleural effusions in a series of 181 outpatients with sarcoidosis. Huggins JT, Doelken P, Sahn SA, King L, Judson MA Chest. 2006 Jun; 129(6):1599-604
2. A Case of Chylothorax Causing Pleural Effusion in Sarcoidosis Nancy Holder, MD 1 , Mihir Barvalia, MD 1 , Carla Wang-Kocik, MD 1 , Harish Seethamraju, MD 1 , Thiruvengadam Anandarangam, MD
3. Pleural sarcoidosis diagnosed on the basis of an increased CD4/CD8 lymphocyte ratio in pleural effusion fluid: a case report Toru Kumagai, Yasuhiko Tomita, Takako Inoue, Junji Uchida, Kazumi Nishino and Fumio Imamura Journal of Medical Case Reports20159:170 DOI: 10.1186/s13256-015-0656
4. Sarcoidosis. Iannuzzi MC, Rybicki BA, Teirstein AS. N Engl J Med 2007;357(21):2153-2165
(P638)