Audit of GP Referrals for Tonsillectomy to the ENT Clinic Using Present HIQA Guidelines
W Hasan, I O’Riordan, J Kinsella, D McShane
Otolaryngology, Head & Neck Surgery Department, Tallaght Hospital, Dublin 24
Abstract
Recurrent sore throat for possible tonsillectomy is the commonest clinical entity referred to the ENT outpatient department. The numbers involved represent a large clinical burden on the service. Not all of these patients require surgical intervention. Patients who fit the criteria for tonsillectomy are faced with two stage obstacles; the long waiting time until assessed by the Otolaryngologist at OPD and the time spent on long operative waiting lists. The aim of this study was to analyze the percentage of referred patients with sore throats requiring tonsillectomy versus those not needing surgery, using the present HIQA guidelines for this operation.
Introduction
The main guidelines for tonsillectomy in the US, UK and Ireland are the Clinical Practice Guidelines: Tonsillectomy in Children, American Academy of Otolaryngology- Head and Neck Surgery (2011), SIGN 117- Management of Sore Throat and Indication for Tonsillectomy (2010) in the UK and in Ireland, a Health Technology Assessment of Scheduled Surgical Procedures- Tonsillectomy HSE, April 2013. These guides are predominantly based on the criteria set forward by Paradise et al1 in the New England Journal of Medicine in 1984, which showed a proven benefit in performing tonsillectomy in patients who meet a specific number of episodes of tonsillitis; 7 episodes or more in one year, 5 episodes or more a year for 2 consecutive years, or 3 or more a year for at least 3 consecutive years. In Paradise’s study, 187 children who met the criteria underwent either tonsillectomy or were managed medically. Half of the children were randomised to either option, while the other half were assigned according to parental preference. Follow up showed a statistically significant reduction in incidence of illness due to sore throat at 2 years follow-up in children who had tonsillectomy compared to those who were managed medically. However, no statistically significant difference was found at 3 years period. Despite the obvious time lapse of the publication of this sentinel paper by Paradise, his criteria still form the basis of current international clinical practice guidelines for tonsillectomy.
The American Academy of Otolaryngology recommends watchful waiting for children who do not meet the Paradise Criteria2. However, they do recommend surgery for certain group of children who do not meet the criteria but who may benefit from surgery. These include children with multiple antibiotic allergy, aphthous stomatitis or recurrent peritonsillar abscess. The SIGN guidelines in the UK also uphold the Paradise Criteria, while stating explicitly that each of the episodes of tonsillitis must be well documented, clinically significant and adequately treated.3 Tonsillectomy was also advocated for children in whom the episodes of sore throat are wholly disabling and prevent normal functioning. In Ireland, the guidelines in use again advocate tonsillectomy in children and adults meeting Paradise’s criteria. In addition of sore throat they also include associated criteria useful in determining if the bout of sore throat is significant. These are temperature >38.3oC, cervical lymphadenopathy, tonsillar exudate or a positive culture for group A beta-haemolytic streptococcus. They again make exceptions for children in particular circumstances, such as immunocompromised children or those with diabetes or cystic fibrosis in which tonsillitis would leave them at risk of complications.
Methods
A prospective study of 58 consecutive patients of all ages referred to our ENT clinic in Tallaght Hospital with recurrent sore throat for possible tonsillectomy was undertaken. A proforma based on the exact HIQA guidelines for tonsillectomy in patients with sore throat was completed during each consultation. Patients were booked for tonsillectomy, discharged back to their General Practitioner (GP) or reviewed after six months in the clinic.
Results
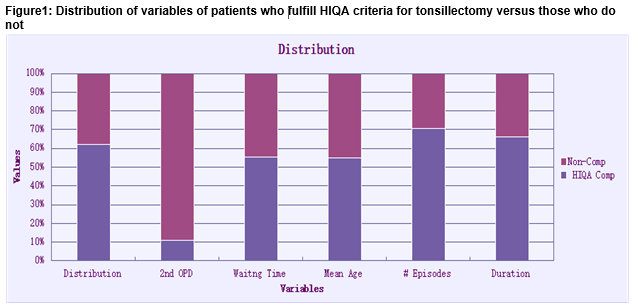
Data of all 58 patients were included in the study. Overall, 36 (62%) meet the HIQA guidelines for tonsillectomy and 22 (38%) did not. Of those who met the criteria 33 (91.6%) were listed for surgery at first consultation and 3 (8.3%) needed a second OPD visit for other investigations. The mean waiting time from referral to first OPD consultation was 19.2 (1-48) months with SD 14.9. Thirty two patients (88.8%) were referred by GPs and 4 (11.1%) were referred from other sources. The mean age at first consultation was 10.2 (4-36) with SD 7.7. The mean number of episodes of sore throats per year was 7.3 (3-12) with SD 3. The mean duration of symptoms was 4.3 years (1-10) with SD 2.3. Of the 22 patients who did not meet the criteria for tonsillectomy 15 (68.1%) were booked for second follow up visit in 6 months and 7 (31.8%) were discharged back to their GPs. The mean waiting time before first OPD consultation was 15.4 (5-26) months with SD 5.5. Twenty one patients (95.4%) were referred by GPs only and 1 (4.5%) had an alternative referral source. The mean age at first consultation was 8.4 (3-23) with SD 4.6. The mean number of episodes per year was 3 (0-12) with SD 3.1. The mean duration of symptoms was 2.2 years (1-4) with SD 1.05. (Fig1)
Discussion
The guidelines in the US, Britain and Ireland are quite similar in relation to indication for recurrent tonsillectomy, with difference reflective of different population specifics e.g. incidence of cystic fibrosis in Ireland. In recent years, various studies have looked at whether these widely accepted guidelines are adequately treating children. Al-Hussaini et al performed a retrospective study in 2013 to analyze the number of tonsillectomies performed, and the number of hospital admissions for tonsillitis and peritonsillar abscess between 1999 and 2010 in the UK4. There was a significant decrease in the number of children undergoing tonsillectomy since the SIGN guidelines for tonsillectomy were published in 2010, (p=0.005 in England and p=0.003 in Wales) and a significant increase in the number of admissions for hospital for tonsillitis. The authors suggest that the current guidelines are too stringent and rule out tonsillectomy for some children who may benefit from the procedure. This concern is also outlined in the Position Paper from ENT UK in 20095. This document also highlights the falling number of tonsillectomies and the increasing number of hospital admissions in the UK for tonsillitis and suggests possible correlation. However, contrary to these studies, a 10 years retrospective study of patients undergoing tonsillectomy from 2003 to 2012 at a tertiary care children’s hospital in the US showed a significant increase in the number of admission with tonsillitis for both adults and children (increase by 118% and 179% respectively) despite a negligible change in tonsillectomy rates6. These conflicting results represent an area that requires further study to investigate whether more stringent criteria for tonsillectomy are likely to cause an increase in hospital admissions for tonsillitis. Since the introduction of these guidelines throughout the UK, few studies have elucidated whether these guidelines are actually being adhered to in clinical practice, in terms of both GP referrals and ENT surgeon’s decision to operate. Other factors may influence a surgeon’s decision as to whether to operate or not. A 2008 UK audit examined whether there was documentation of SIGN criteria in children undergoing tonsillectomy7. It was found that in 100 children, 44% were documented to have met the SIGN criteria for tonsillectomy preoperatively. This is an increase from a previously documented 12%7. However it still represents less than half of children and highlights the need for clear and concise documentation of criteria. The study also highlights possible subjective decisions made by Otolaryngologists to operate on children that may fall outside the criteria for tonsillectomy but may benefit from the operation. The current literature suggests a gap in the evidence base related to the indications for tonsillectomy, as despite very similar and clear guidelines that are in place, very few studies have examined to what extent these guidelines are being followed, and overall, how beneficial these guidelines have been proven to be since their introduction in 1987.
Recurrent tonsillitis is a very common condition that is debilitating for sufferers. For the majority of patients, surgical intervention with tonsillectomy remains the only cure. As demonstrated in this study, improved awareness by GPs of the HIQA guidelines for tonsillectomy would significantly reduce the number of referrals to the ENT outpatient service and hence speed the process towards earlier surgical intervention for those who would benefit from surgery. An educational programme in this regard for GPs would likely have a significant effect in reducing waiting times for ENT outpatient appointments. Consideration should also be given to a specialist nurse led assessment service whereby unnecessary referrals can be screened out and returned to the referring doctor to facilitate quicker OPD assessment of patients who are more likely to require a tonsillectomy.
Corresponding Author:
Wael Hasan, Otolaryngology, Head / Neck Surgery Department, Tallaght Hospital, Dublin 24
Tel: 00353 872739577
Conflict of Interest:
The authors declare no conflict of interest in this study
References:
1. Paradise JL, Bluestone CD, Bachman RZ. Efficacy of tonsillectomy for recurrent throat infection in severely affected children. Results of parallel randomized and nonrandomized clinical trials. N Engl J Med 1984;310:674–683.
2. American Academy of Otolaryngology, AAO-HNSF Clinical Practice Guideline: Tonsillectomy in Children January 3, 2011.
3. SIGN. Management of sore throat and indications for tonsillectomy. Edinburgh: Scottish Intercollegiate Guidelines Network; 2010. Report No.:117.
4. A Al-hussaini, D Owens, A Tomkinson. Health costs and consequences: have UK national guidelines had any effect on tonsillectomy rates and hospital admissions for tonsillitis? European Archives for Otorhinolargnyology. May 2013, Volume 270, Issue 6, pp 1959-1965.
5. Indications for Tonsillectomy: Position Paper ENT UK 2009.
6. H Patel, C Straight, E Lehman, M Tanner, M Carr. Evolving Indications for Tonsillectomy. Otolaryngology Head Neck Surg September 2013 vol. 149 no. 2 suppl P245.
7. A Toh, A Mullin, J Grainger,H Uppal. Indications for Tonsillectomy: Are We Documenting Them? Ann R Coll Surg Engl. Nov 2009; 91: 697–699.
P470