Commotio Cordis Caused During Hurling Game
C. Connellan1, S. Kelleher2 (co-authors)
M. Islam1, D. Kenny2, A. James2, T. Prendiville2, K. Walsh2
1. Galway University Hospital
2. Our Lady’s Children’s Hospital, Crumlin
Abstract
A teenage boy had a cardiac arrest following a blow to the chest from a hurling ball (sliotar). Prompt resuscitation and automated external defibrillation enabled a full recovery. This is the first reported case of commotio cordis caused by a sliotar although it is described in other sports. Primary prevention of commotio cordis (CC) and secondary prevention of cardiac death are discussed.
Introduction
‘Commotio cordis’ describes cardiac arrhythmia due to blunt chest trauma occuring during ventricular repolarisation, in the absence of structural damage.1,2 It is a rare but important cause of sudden cardiac death (SCD) where the incidence of SCD in 14 - 35 year olds in Ireland between 2005 and 2007 is 4.96 for males and 1.3 for females per 100,000 person-years.3 While there is a commotio cordis registry in the U.S., this does not exist in Europe and CC is likely underreported. Considering that most CC cases occur in adolescents and have a high mortality rate, timely management of cardiac arrest is key.4
Case Report
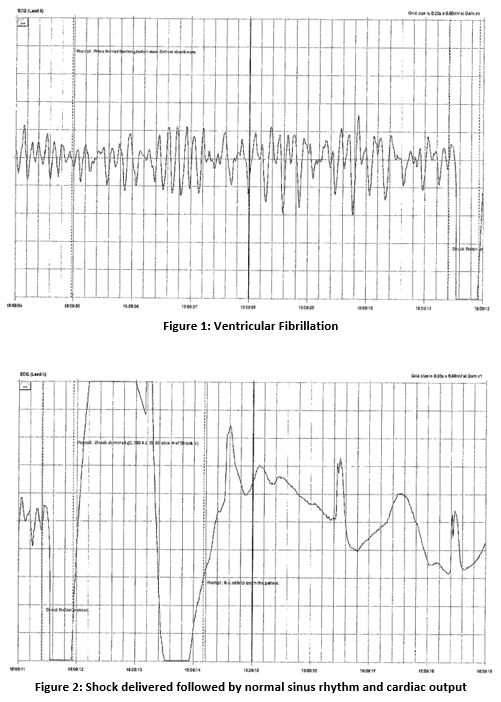
A previously well 13 year old collapsed following a blow from a sliotar to the left side of his chest. His mother, a nurse, commenced CPR almost immediately after determining there was no pulse. An AED was applied and 1 shock delivered achieving return of spontaneous circulation with print outs below. ‘Down time’ was less than 4 minutes and his GCS was 15 by the time of ambulance arrival. He had a normal examination and ECG on admission with potassium of 4.0 mmol/L and blood glucose 9.1 mmol/L. Troponin peaked at 607ng/l at 4 hours (normal range <14) with CPK reaching 325 U/L (normal range <308) at 24 hours. This was expected following CPR and quickly fell.
During monitoring in the Cardiac ICU, he experienced progressively longer, asymptomatic episodes of ventricular tachycardia, with runs up to 22 beats and frequent premature atrial contractions (PACs). He was commenced on an infusion of a class II antiarrhythmic, esmolol. Despite side effects of bradycardia and hypotension this was well tolerated with cessation of the bouts of ventricular tachycardia, and he was successfully transitioned to oral bisoprolol. The patient was advised not to return to competitive sport for 3 months. Beta-blockade therapy was continued during this period.
A diagnosis of CC requires the exclusion of other causes of ventricular fibrillation. An echocardiogram out-ruled cardiomyopathy and cardiac MRI out-ruled arrhythmogenic cardiac scarring although it did show non-specific fat saturation in the right ventricular outflow tract. This is considered incidental, but warrants repeat in 2 years to outrule any progression. Exercise stress testing revealed no arrhythmia and normal recovery phase parameters. Thus, the diagnosis of CC was reached.
Discussion
Primary prevention of CC centres around the use of protective chest wall shields or of soft balls.1 However, even when worn chest shields are not wholly protective against CC1, particularly in such an agile sport where the shield would move, rendering protection incomplete. Replacing the sliotar with a soft ball is unlikely to be acceptable as the fundamental characteristics of the game would be significantly altered and CC is such a rare event. We suggest efforts instead focus on the response to cardiac arrest.
In secondary prevention of SCD CPR training and rapid access to AEDs are lifesaving measures, as seen in this case. Indeed, prompt resuscitation and access to AEDs are associated with increased survival rates in CC, which are now as high as 58%.4 Due consideration has been given to introducing a public access AED programme, however the cost benefit analysis of implementing an effective scheme and the large number of AEDs already provided on a voluntary basis suggest public expenditure be otherwise appropriated.5 However, there is no mandated upkeep of voluntary AEDs nor an AED registry in Ireland. We believe that prompt access to existing, well maintained AEDs, effective CPR and integration with emergency services will improve survival in out of hospital cardiac arrests whether from rare causes like CC or more common causes.
Conflicts of Interest Statement
The authors do not have any conflicts of interest to declare.
Corresponding Author
Dr. Claire Connellan
Care of Louise,
Secretary to Dr Orla Flanagan,
Paediatric Department,
Galway University Hospital
Email: [email protected]
References
1. Link MS, Estes III NAM, Maron BJ. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: task force 13: Commotio Cordis: a scientific statement from the American Heart Association and American College of Cardiology. Circulation. 2015;132(22):e339-e42.
2. Maron BJ, Gohman TE, Kyle SB, Estes III NAM, Link MS. Clinical profile and spectrum of commotio cordis. JAMA. 2002;287(9):1142-6.
3. Margey R, Roy A, Tobin S, O'Keane CJ, McGorrian C, Morris V, Jennings S, Galvin J. Sudden cardiac death in 14- to 35-year olds in Ireland from 2005 to 2007: a retrospective registry. Europace. 2011;13(10):1411-8.
4. Maron B, Haas T, Ahluwalia A, Garberich R, Estes III NAM, Link M. Increasing survival rate from commotio cordis. Heart Rhythm. 2013;10(2):219-223.
5. Health Information and Quality Authority. Health technology assessment (HTA) of public access defibrillation. Dublin: HIQA, 2014.
Issue: Ir Med J; Vol 112; No. 6; P956
