Cross-sectional Analysis of the Standards of Consent Applied to Anaesthesia in Ireland: Are Anaesthetists Aware of their Legal and Ethical Obligations?
Cafferkey A1, Lyons B2
1Department of Anaesthesia, The Royal Victoria Eye and Ear Hospital, Dublin 2
2Department of Anaesthesia, Our Lady’s Children’s Hospital, Crumlin, Dublin 12
Abstract
Consent to a medical intervention has legally and ethically evolved to a process prioritising autonomy and patient-led decision-making. This cross-sectional analysis investigated Irish anaesthetists’ practices of taking consent. Following ethical approval, trainees and fellows of the College of Anaesthetists of Ireland were invited to participate in a 33 question online survey. One hundred and sixty responses (11.8%) were received, an equal number coming from consultants and trainees. The majority (93.7%) worked in a teaching hospital. Fifteen percent said their department had guidelines on obtaining consent for anaesthesia, but only 4.5% said their department used a separate consent form. Most (63.8%) do not usually document consent. A significant number rarely (21.8%) or never (27.8%) explained risks to patients. Lack of time was identified as the most frequent barrier (77.6%), with just under half first meeting the patient in the theatre holding-bay or the anaesthetic room. Forty-one percent felt the ultimate decision regarding which anaesthetic technique is employed should usually lie with the anaesthetist alone. These results suggest a wide variation in the practice of obtaining consent for anaesthesia. Less than half deemed their practice to be adequate in this regard, while 50% were concerned about litigation stemming from inadequate consent.
Introduction
In order for consent to be valid, the patient “must have received sufficient information in a comprehensible manner about the nature, purpose, benefits and risks of an intervention…; [must] not be acting under duress; and [must] have the capacity to make the particular decision”1. In Ireland, there seems to be a wide variation in the practice of obtaining consent and many ‘consents’ may not fulfill the necessary ethical and legal requirements2.
The role of the anaesthetist as a peri-operative physician is usually to facilitate an intervention carried out by another speciality. Encounters with patients are often brief, leaving little time for the consent process and to ensure that the patient “retains ultimate decision-making authority”1. In addition, the role of the anaesthetist is poorly understood by many Irish patients3,4, and patients may not regard their discussion with an anaesthetist as a consent process in itself5. Thus, patient expectations of the ‘anaesthetic consent process’ are arguably different to those of other specialities6.
The aims of the survey were to examine the practice of obtaining consent for anaesthesia, to determine knowledge and utilisation of available professional guidance, to identify limitations to the consent process for anaesthesia, and to investigate anaesthetists’ awareness of their professional and legal obligations in relation to consent.
Methods
Ethical approval was granted by the Royal College of Surgeons in Ireland Research Ethics Committee. All trainees and fellows of the College of Anaesthetists of Ireland (approximately 1350) were emailed on three separate occasions to request participation in this anonymous online survey. The survey contained 33 questions: five related to participant demographics and work practices; three to knowledge and utilisation of available guidance; fourteen to the practice of obtaining consent; four to documentation of consent; five to awareness of professional and legal obligations, while two related to limitations to the consent process for anaesthesia.
Results
One hundred and sixty responses were received, a response rate of 11.8%.
Anaesthetist Demographics
Most respondents were aged 30-39 years (41.9%), followed by 40-49 (24.4%), 20-29 (14.4%), 50–59 (13.7%), 60-69 (3.7%), and >70 (1.9%). Over half had been practicing anaesthesia >10 years (51.2%), followed by 4-6 years (16.9%), two to four years (11.9%), zero to two years (10.6%), 6-8 years (5%), and 8-10 years (4.4%). Half of respondents were consultants, with the remainder split between different stages of training. There was overlap in the work practices of those surveyed. Most (93.7%) worked in a teaching hospital, while 16.9% worked in a private hospital. Most (94.9%) practiced general adult anaesthesia, 48.7% practiced obstetric anaesthesia and 47.5% practiced paediatric anaesthesia.
Knowledge and Utilisation of Available Guidance
Just 15% replied that their department had guidelines on how to obtain consent for anaesthesia. The most commonly used source of guidance was the Association of Anaesthetists of Great Britain and Ireland (AAGBI) (46.1%), followed by advice from colleagues (37%), the Irish Medical Council (25.9%), the respondent’s anaesthetic department guidelines (19.5%), and medical indemnifiers (15.6%). Guidance from the Health Service Executive (HSE) was the least frequently used source (8.4%). Some used multiple sources, but one-third reported using none. Most (69%) were unaware of the HSE National Consent Policy. Of those who knew of it, just under 40% had read it
Documentation of Consent and Awareness of Obligations
Most (63.8%) do not usually document consent for anaesthesia. Of those who do so, nearly all use the anaesthetic record, while very few (1.8%) use a separate consent form. In keeping with this finding, a minority (4.5%) reported that their department had a separate anaesthesia consent form.
Just over half of respondents were sure of their ethical and legal obligations when obtaining consent. A similar number agreed that having a separate written consent form for anaesthesia would improve the standard of consent, while one-third felt that this would provide better protection against litigation. Less than half deemed their practice for obtaining consent to be adequate and expressed concern about litigation stemming from this deficiency (Table 1).
Risk Disclosure and Discussion of Alternatives
Most (81.6%) explain the benefits of their proposed technique always or most of the time. A significant proportion (11.9%) never explain all of the risks. A fifth rarely or never explain common risks with benign consequences. A quarter rarely or never disclose rare risks which have serious consequences.
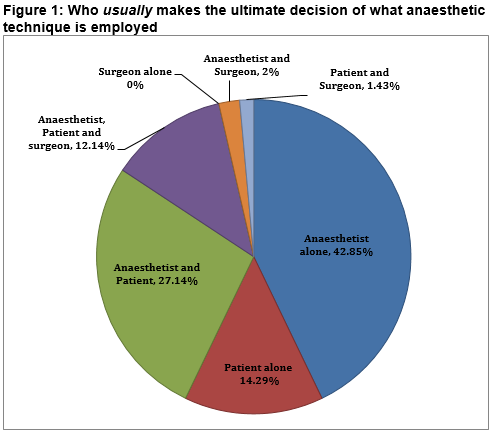
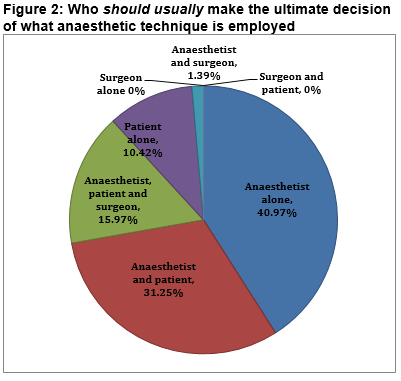
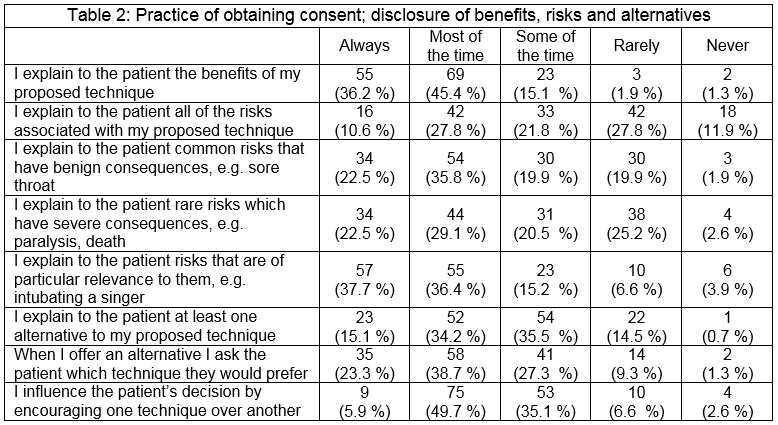 Half of those surveyed always or most of the time explain at least one alternative to the proposed anaesthetic technique. A significant proportion (15.1%) rarely or never do so. Of those offering an alternative, two-thirds ask the patient which technique they would prefer, but few would explain all alternatives (table 2). Two-thirds agreed that their proposed anaesthetic technique is influenced by the patient’s wishes. A minority disagreed with this statement. The majority agreed that their proposed anaesthetic technique is influenced by their skills/experience (table 1). Nearly half of respondents feel that the ultimate decision regarding which anaesthetic technique is employed usually and should usually lie with the anaesthetist alone (figures 1 & 2). The patient was identified as the sole decision-maker by 14.3% and as part of the decision-making group by 55% when asked who usually makes this decision.
Half of those surveyed always or most of the time explain at least one alternative to the proposed anaesthetic technique. A significant proportion (15.1%) rarely or never do so. Of those offering an alternative, two-thirds ask the patient which technique they would prefer, but few would explain all alternatives (table 2). Two-thirds agreed that their proposed anaesthetic technique is influenced by the patient’s wishes. A minority disagreed with this statement. The majority agreed that their proposed anaesthetic technique is influenced by their skills/experience (table 1). Nearly half of respondents feel that the ultimate decision regarding which anaesthetic technique is employed usually and should usually lie with the anaesthetist alone (figures 1 & 2). The patient was identified as the sole decision-maker by 14.3% and as part of the decision-making group by 55% when asked who usually makes this decision.
Timing of Consent
Nearly half reported that their first contact with most patients where technique is discussed occurs either in the theatre holding bay (35.7%) or in the anaesthetic room prior to the induction of anaesthesia (11.9%). This discussion begins in the pre-operative assessment clinic in 19.6%, and on the ward prior to surgery in 32.9%. A quarter disagreed with the statement that the patient is given enough time to digest the information provided (table 1).
Consent
Time constraints were identified as the commonest barrier (77.6%), followed by: a fear of scaring the patient or dissuading them from undergoing the procedure (48.2%); lack of guidance regarding what is expected when obtaining consent for anaesthesia (47.6%); concerns about a patient’s ability to understand what is proposed/their options (39.9%); language barriers (17.5%). Two-thirds (62.1%) agreed that there was a lack of clear guidance for anaesthetists to consult when obtaining consent.
Discussion
This study has several limitations. The low response rate limits the validity and generalisability of the findings. In addition, it raises the question of whether anaesthetists view consent as an important issue that is separate from the surgical consent. Anaesthetists who have a particular interest in consent may have been drawn to taking part. The HSE Consent Policy suggests that anaesthetists should obtain separate consent for anaesthesia, and that relying on the surgical consent to encompass anaesthesia may amount to “inappropriate delegation… [which] may render the consent invalid”1. The AAGBI state that it is up to the anaesthetist to ensure that the patient is given and comprehends information relating to their anaesthetic7.
Despite over half of respondents stating that they were aware of their ethical and legal obligations when obtaining consent for anaesthesia, a paternalistic approach to decision-making emerged. The anaesthetist alone was viewed as the person who usually or should usually make the ultimate decision regarding the type of anaesthesia used in many cases. This seems contrary to the doctor’s “duty to help patients to make decisions for themselves”8. A survey of UK anaesthetists and surgeons revealed similar views, where 10% of anaesthetists and two percentof surgeons disagreed that a main purpose of consent was to respect a patient’s autonomy9. Over half of respondents influenced their patient’s decision by encouraging one technique over another. Giving the patient “strong recommendations regarding a particular treatment” does not amount to duress1. Indeed the AAGBI view it as “good practice” for the anaesthetist to give their opinion, but caution care that patient autonomy is not overridden7.
The ‘reasonable patient’ standard of risk disclosure necessitates the discussion “of any material risk, whether [the patient] inquires or not, regardless of it’s infrequency”10. Therefore, “common, even if minor, side effects [and]… rare but serious adverse outcomes…. [which] includes death, permanent disability… [or] disfigurement and chronic pain [should be disclosed]”1. Our survey findings are in keeping with other studies that have shown that minor commonly occurring risks are disclosed frequently, while serious but rare risks are disclosed infrequently11-14. Of concern, a number of respondents never or rarely disclosed common or rare risks, potentially invalidating the consent.
Patients should be informed of all alternatives and their associated risks, benefits and likelihoods of success1,15. Our results concur with previous studies identifying that discussion of alternative anaesthetic techniques varies widely, and may not take place at all5,13,16,17. Risk disclosure immediately prior to a procedure may render the consent invalid, especially in the context of elective surgery1,18. The AAGBI state that “the anaesthetic room is not an acceptable time or place to provide patients with new information other than in exceptional circumstances”7. Despite this, a heterogenous patient population exists where some actually want consent to be given at this very time, while others would like a longer time frame between giving consent and the procedure itself4,6,17. In reality, it may be very difficult for the anaesthetist to ascertain exactly what their patient wants given that nearly half of those surveyed first meet the majority of their patients immediately prior to the administration of the anaesthetic.
The recent Montgomery judgement in the UK Supreme Court19 prompted the Royal College of Surgeons (UK) to publish new guidance on consent, reflecting a patient-centred shift in standard20. This document highlights the surgeon’s obligation to provide individualised information to equip each patient with the knowledge necessary to decide what treatment, if any, they will undergo. Considerable time is required “to get to know the patient well enough to understand their views and values” so that they can make an informed decision that reflects their wishes20. Our survey suggests that anaesthetists frequently do not get this exposure to their patients pre-operatively to explore their desires adequately, if at all.
The majority of respondents were unaware of the HSE Consent Policy, even though nearly all work in teaching hospitals, of which most would be under the auspices of the HSE. This likely reflects the generic nature of this policy and raises questions over the accessibility and dissemination of HSE guidance on consent within anaesthetic departments. Indeed, a significant number were concerned regarding the lack of guidance available for consent on anaesthesia. Specific guidance from the HSE addressing difficulties encountered when obtaining consent for anaesthesia may provide clarity to ensure that the process of consent is in line with recommended principles and legal obligations.
In summary, despite the study limitations, our findings suggest that there is a wide variation in how the principles of consent are applied in anaesthesia practice in Ireland. The HSE National Clinical Programme in Anaesthesia Model of Care for Pre-admission Units21 has highlighted the importance of pre-operative assessment clinics in the preparation of patients for anaesthesia including beginning the consent process. However, this survey has identified important discrepancies between the obligations of anaesthetists and their clinical practice. The patient population is heterogeneous, with varying desires regarding each aspect of the consent process. These differing needs can only be determined by adequate dialogue between the anaesthetist and patient, which is difficult given the significant time constraints identified in our survey. This has important implications for the planning and provision of anaesthesia services in the future
Conflict Of Interest
Neither author has any conflict of interest to declare
Correspondence: A Cafferkey, The Royal Victoria Eye and Ear Hospital, Dublin 2
Email: [email protected]
References
1. Health Service Executive. National Consent Policy. (2013).
2. Madden D. Medicine, Ethics and the Law. Second ed: Bloomsbury; 2011.
3. Smith A, Mannion S. Irish patients knowledge and perception of anaesthesia. Irish medical journal. 2013;106(2):50-2.
4. Frohlich S, Tan T, Walsh A, Carey M. Epidural Analgesia for labour: Maternal Knowledge, Preferences and Informed Consent. Irish medical journal. 2011;104(10):300-2.
5. Zarnegar R, Brown MR, Henley M, Tidman V, Pathmanathan A. Patient perceptions and recall of consent for regional anaesthesia compared with consent for surgery. Journal of the Royal Society of Medicine. 2015;108(11):451-6.
6. Burkle CM, Pasternak JJ, Armstrong MH, Keegan MT. Patient perspectives on informed consent for anaesthesia and surgery: American attitudes. Acta anaesthesiologica Scandinavica. 2013;57(3):342-9.
7. The Association of Anaesthetists of Great Britain and Ireland. Consent for Anaesthesia. (2006).
8. Medical Council. Guide to Professional Conduct and Ethics for Registered Medical Practitioners. (8th ed) 2016.
9. Jamjoom AA, White S, Walton SM, Hardman JG, Moppett IK. Anaesthetists' and surgeons' attitudes towards informed consent in the UK: an observational study. BMC medical ethics. 2010;11:2.
10. Geoghegan v. Harris [2000] IEHC 129.
11. Brull R, McCartney CJ, Chan VW, Liguori GA, Hargett MJ, Xu D, Abbas S, El-Beheiry H. Disclosure of risks associated with regional anesthesia: a survey of academic regional anesthesiologists. Regional anesthesia and pain medicine. 2007;32(1):7-11.
12. Hegarty A, Omer W, Harmon D. Informed consent for epidural analgesia in labour: a survey of Irish practice. Irish medical journal. 2014;107(6):183-4.
13. Sakaguchi M, Maeda S. Informed consent for anesthesia: survey of current practices in Japan. Journal of anesthesia. 2005;19(4):315-9.
14. Braun AR, Leslie K, Merry AF, Story D. What are we telling our patients? A survey of risk disclosure for anaesthesia in Australia and New Zealand. Anaesthesia and intensive care. 2010;38(5):935-8.
15. Birch v University College London Hospital NHS Foundation Trust [2008] EWHC 2237.
16. Ranganathan P, Patil V. Informed consent for anesthesia: a survey among Indian anesthesiologists. Journal of anesthesia. 2011;25(4):633-4.
17. Tait AR, Voepel-Lewis T, Gauger V. Parental recall of anesthesia information: informing the practice of informed consent. Anesthesia and analgesia. 2011;112(4):918-23.
18. Fitzpatrick v White [2007] IESC 51.
19. Montgomery v Lanarkshire Health Board [2015] UKSC 11.
20. Consent: Supported Decision Making. A Guide to Good Practice. The Royal College of Surgeons of England. 2016.
21. Health Service Executive National Clinical Programme in Anaesthesia Model of Care for Pre-admission Units 2014. Available from: http://www.hse.ie/eng/about/Who/clinical/natclinprog/anaesthesia/modelofcare.pdf.
P668