Donegal Going against the Flow: National Differences in Long-Term Urinary Catheterisation Rates in Men (> 65 Years) With Benign Prostatic Hypertrophy.
R Stewart1, S Maguire1, K Hanley2 , P Armstrong3
1Donegal Specialist Training Scheme in General Practice, The Education Centre, St Conal’s, Letterkenny, Donegal
2National Director of GP Training, ICGP, Donegal Specialist Training Scheme in General Practice
3Lifford Health Centre, Donegal
Abstract
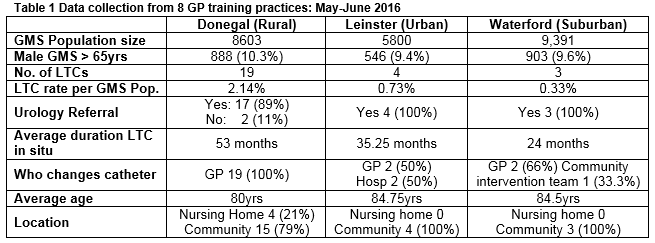
An analysis of Primary Care Reimbursement Service (PCRS, 2013) data demonstrated high rates of urinary catheter changes in Donegal compared to other regions of Ireland. There is a catheter change rate of 10.2% in Donegal men over 65 with medical cards (GMS) compared to rates of 2.7% and 0.17% in Waterford and South Dublin, respectively1. This 60-fold difference between an area with perceived good access to services (South Dublin) and Donegal an area that does not, prompted a survey of general practitioners in each of these areas to assess whether true male catheterisation rates were similarly disproportionate in Donegal. Based on this, data was collected from a population of 23,794 GMS patients in GP training practices in Donegal (Rural), Leinster (Urban) and Waterford (Suburban). The data sampled for Donegal demonstrated 19 long-term catheters (LTCs per 8603 GMS) compared to four LTCs (per 5,800 GMS) in Leinster and 3 LTCs (per 9,391 GMS) in Waterford (Table 1). This anomaly in LTC rates may be a proxy for lack of access to basic Urology services.
Introduction
Donegal is a geographically removed county known to have high levels of social deprivation2. Areas like this are known to face particular challenges when it comes to provision of healthcare services3. Data from the National Treatment purchase fund demonstrates that approximately 50% of patients are waiting for more than a year for Urology outpatient appoitments4. Letterkenny University Hospital (LUH) currently does not have an inpatient Urology service. Benign prostatic hypertrophy (BPH) and its associated chronic obstructive urological symptoms are common in men over the age of 50. Primary treatment options include the use of medical therapies and surgical procedures such as a transurethral resection of the prostate (TURP)5. The estimated UK prevalence for LTCs in men >75yrs is 0.5%6.Guidance refers to urinary catheterization as a temporary measure for relieving acute urinary retention (AUR) and not a long-term treatment option5,7,8.
LTCs have many potential complications including the risk of urinary tract infection, pain, psychological distress and impact on sexual function9. As such, the use of LTCs should be reserved as a last resort when treating chronic obstructive urological symptoms5,8. Analysis of Primary Care Reimbursement Service (PCRS, 2013) data demonstrated high rates of urinary catheter changes in Donegal compared to the rest of Ireland: 10.2% in Donegal men over 65 (GMS) compared to rates of 2.7% and 0.17% in Waterford and South Dublin, respectively1. PCRS is the system used to record and process specialist treatment claims by GPs, of which the insertion of a urinary catheter is one. This study aimed to survey general practices in Donegal and two other areas (comparing rural, suburban and urban areas) of Ireland to assess whether this disproportionately high LTC change rate meant that greater numbers of men with BPH in Donegal had long term catheters. The data was collected (May-June 2016) to examine the trend in figures demonstrated in the PCRS report and to further explore the possible reasons behind the anomalies found in the data.
Methods
Preliminary data analysis was collected from the PCRS data report 20131.This data was used to inform a data collection tool. This tool was used to form a retrospective survey which was dispensed to 9 randomly selected GP training practices in Donegal (Rural), Leinster (Urban) and the South East (Suburban). Inclusion criteria included GMS patients; 65 years or older; with a diagnosis of BPH who have a LTC in situ (defined as >28 days). Data was collected by GP trainers and trainees. Patients were identified by; surveying all practice staff to identify relevant patients, electronic patient file search – search terms “BPH” and retrospective review of STC claims). 8 of 9 practices surveyed responded. Given the size of GP practices and their familiarity with those who require LTC changes on a three monthly basis the risk of underreporting is limited.
Results
Discussion
There is no current inpatient urology service in Letterkenny University Hospital and the waiting list for a routine appointment is currently >1.5 years (as of 07/12/201610). The initial PCRS figures used, come from 2013 when Letterkenny University Hospital had a Urology service in place. More recent 2015 data is comparable1. It is clear from the data that there are significant differences in both rates and duration of urinary catheters in Donegal compared to Leinster and Waterford even when taken in the context of demographic differences. This appears to be an anomaly and is not seen with other types of PCRS claim1. It may therefore be reasonable to postulate that this represents a lack of access to urology services.
Acknowledgement
The author would like to acknowledge the help of the Donegal Specialist Training Scheme in General Practice and the general practitioners who agreed to take part in the study.
Conflict of Interest
The authors declare that they have no competing interests.
Correspondence:
Dr Rory Stewart, GP Registrar, Donegal Specialist Training Scheme in General Practice.
Email: [email protected]
References
1. Primary Care Reimbusment Service (PCRS) Annual data report, 2013 & 2015. Available at URL: http://www.hse.ie/eng/staff/PCRS/PCRS_Publications/
2. Irish Central Statistics Office (CSO) Census Report, 2011. Available at URL: http://census.cso.ie/areaprofiles/areaprofile.aspx?Geog_Type=CTY&Geog_Code=33
3. Call for urgent action to tackle urology waiting list at Letterkenny General Hospital. Donegal Now. 2015 Oct 07. Available from URL: https://www.donegalnow.com/news/call-for-urgent-action-to-tackle-urology-waiting-list-at-letterkenny-general-hospital/48363
4. The National Treatment Purchase Fund. Outpatient waiting lists, 2017. Available at URL: http://www.ntpf.ie/home/pdf//2017/01/specialities/out-patient/7800.pdf
5. Nickel, JC. Méndez-Probst, CE. Whelan, TF. Paterson, RF. Razvi, H. Update: Guidelines for the management of benign prostatic hyperplasia. Can Urol Assoc J. 2010 Oct; 4(5): 310–316.
6. NICE guideline: Healthcare-associated infections: prevention and control in primary and community care, 2012. Available at URL: https://www.nice.org.uk/Guidance/CG139
7. IPCC Guidelines for the Prevention of Catheter associated Urinary Tract Infection, 2012. Available at URL:http://www.hse.ie/eng/about/Who/healthwellbeing/Infectcont/Sth/gl/IPCC_Guidelines_Section_12_1.pdf
8. Gould, CV. Umscheid, CA. Agarwal, RK. Kuntz, G. Pegues, DA. And the Healthcare Infection Control Practices Advisory Committee (HICPAC) Guideline for the prevention of catheter associated infections. 2009, 8-34. Available at URL: http://www.cdc.gov/hicpac/pdf/CAUTI/CAUTIguideline2009final.pdf
9. Igawa, Y. Wyndaele, JJ. Nishizawa, O. Catheterization: Possible complications and their prevention and treatment. International Journal of Urology (2008) 15, 481–485.
10. Stewart, R. In conversation with Letterkenny University Hospital appointments department by phone (07/12/2016).
(P640)
