Iatrogenic Bowel Injury at Exchange of Supra-Pubic Catheter
Foran AT, Nason GJ, Rohan P, Keane GM, Connolly S, Hegarty N, Galvin D, O’Malley KJ
Department of Urology, Mater Misericordiae University Hospital, Eccles St, Dublin 7, Ireland
Abstract
Suprapubic catheter insertion and exchange is a common urological procedure, but it is not without risks and complications. While bowel perforation is a recognised complication at suprapubic catheter insertion, it is not commonly reported at suprapubic catheter exchange. We report our experience of recognition, diagnosis and subsequent successful management of the most important complication related to suprapubic catheters.
Case Series
We report a case series of two small bowel perforation at the time of SPC exchange. An 81-year-old man presenting with poor output from SPC in past 48 hours following exchange. The first exchange of SPC had been performed in the outpatients in his wheelchair. He had a history of prostate cancer treated with radiotherapy six years previously. A SPC had been inserted under local anaesthesia with a flexible cystoscope twelve weeks previously due to urinary incontinence. Of note the patient had multiple other medical comorbidities including diverticular disease. There was faeculent material draining into the SPC. The bladder was distended and easily palpable below the umbilicus. A urethral catheter was inserted and drained clear urine. A CT abdomen/pelvis revealed that the SPC was located in a loop of distal ileum, Figure 1. A laparotomy revealed the SPC balloon was lying in the distal ileum causing obstruction with the bowel loop stuck to the anterior abdominal wall. A single fresh entry point in the ileum was noted and the affected bowel was resected, and side to side ileal anastomosis performed. A suprapubic cystotomy and reinsertion of the SPC under direct vision was performed. The patient had an uneventful post-operative recovery and the SPC has been exchanged every three months.
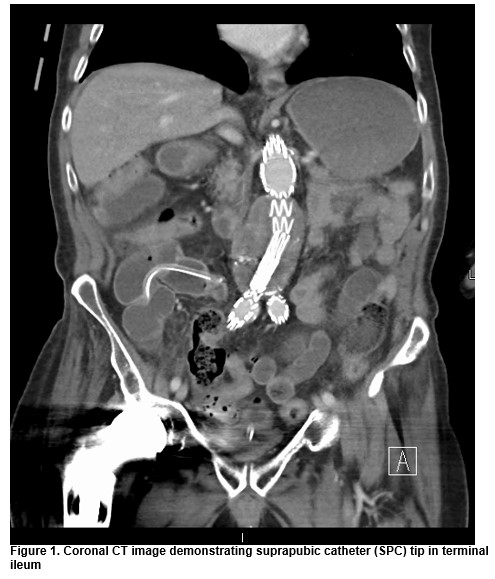
Our second case was an 84-year-old gentleman that attended for his first change of suprapubic catheter. His background medical history was significant for Parkinson’s disease, atrial fibrillation and insulin dependent diabetes mellitus. He presented the day following suprapubic exchange with faeculent material draining from SPC. A CT abdomen revealed single entry point of the catheter into the terminal ileum, Figure 1. At laparotomy, the terminal ileum was fixed to the bladder with an apparent fresh entry point into the bowel. The affected portion of bowel was resected and a new suprapubic catheter was inserted into the bladder under direct vision. The SPC has been changed without complication on a three monthly basis since.
Both cases were following the first exchange of SPC and performed by experienced registrars. In each case, the SPC was removed and immediately replaced using an aspectic technique without reported difficulty. There was no documentation of pre-filling the bladder or flushing the SPC following exchange.
Discussion
Our cases highlights the dangers of this procedure, carrying mortality rates of up to 1.8%6 and highlights the potential risk of bowel perforation. While this risk is well recognised at the time of suprapubic catheter insertion, there is a paucity of cases describing it at time of SPC exchange2-6. Risk factors include the presence of inflammatory conditions1. The weakening of musculature with age, including bowel wall musculature and decrease in abdominal tone could be another contributing factor7, this was reflected in the published literature as the patients were all at least 75 years old1,2,4,5,8. The position of the patient is an important factor- lying the patient flat or in a Trendelenberg position shifts some bowel cranially- exchange in a wheelchair is suboptimal as in our first case. Various areas of the bowel have been injured but the terminal ileum appears to be the most commonly implicated2.
BAUS guidelines 9 currently recommend that SPC be placed either under direct vision or via ultrasound guidance neither of which completely eradicate the risk of bowel injury. Whether the bowel injury occurred at initial insertion, similar to the case described by Ahmed et al10 or at exchange is difficult to say- however given it functioned well for three months in a clinical well patient and there was only one entry site at laparotomy and laparoscopy in both cases- so it would appear the injuries occurred at exchange. If the injury occurred at the time of insertion, an entry and exit point would be expected and the patient likely would have presented unwell earlier. Following review of this case, all elective SPC insertions are now performed in theatre under general anaesthesia (GA) in our unit. Ultrasound guided placed using a Seldinger approach is advisable to ensure bowel segments are not in the line of insertion. Management differed among the cases with conservative methods being successfully employed1, as well as operative management 2, 3, 7. SPC exchange is not free of complications: it should be performed in the supine position, pre-filling of the bladder, immediate exchange and flushing of the SPC following exchange to confirm position are important aspects of a safe exchange. Iatrogenic bowel related-injury is not confined to time of insertion and patients and relatives should be properly consented regarding these complications.
Corresponding Author:
Mr Gregory Nason, FRCS Urol., Specialist Registrar in Urology, Department of Urology,
Mater Misericordiae University Hospital, Eccles St, Dublin 7, Ireland
Email: [email protected]
Conflicts of Interest
The authors have no conflicts of interest to declare.
References
1. Kass-Iliyya A, Morgan K, Beck R, Iacovou J. Bowel injury after a routine change of suprapubic catheter. BMJ Case Rep. 2012;2012.
2. Gallagher KM, Good DW, Brush JP, Alhasso A, Stewart GD. Small bowel injury after suprapubic catheter insertion presenting 3 years after initial insertion. BMJ Case Rep. 2013;2013.
3. Chang C-P, Li J-R, Cheng C-L, Ou Y-C, Ho H-C, Chiu K-Y. Suprapubic catheter change resulting in terminal ileal perforation. Urological Science. 2014;25(2):68-9.
4. Mongiu AK, Helfand BT, Kielb SJ. Small bowel perforation during suprapubic tube exchange. Can J Urol. 2009;16(1):4519-21.
5. Witham MD, Martindale AD. Occult transfixation of the sigmoid colon by suprapubic catheter. Age Ageing. 2002;31(5):407-8.
6. Sheriff MK, Foley S, McFarlane J, Nauth-Misir R, Craggs M, Shah PJ. Long-term suprapubic catheterisation: clinical outcome and satisfaction survey. Spinal Cord. 1998;36(3):171-6.
7. Chitale S, Irving S. Plausible mechanism of small bowel injury during trocar cystostomy. BMJ Case Rep. 2010;2010.
8. Wu CC, Su CT, Lin AC. Terminal ileum perforation from a misplaced percutaneous suprapubic cystostomy. Eur J Emerg Med. 2007;14(2):92-3.
9. Harrison SC, Lawrence WT, Morley R, Pearce I, Taylor J. British Association of Urological Surgeons' suprapubic catheter practice guidelines. BJU Int. 2011;107(1):77-85.
10. Ahmed SJ, Mehta A, Rimington P. Delayed bowel perforation following suprapubic catheter insertion. BMC Urol. 2004;4(1):16.
(P737)
