Incidence of Thyroid Cancer among Patients with Thyroid Nodules
A. Gilmartin1, M. Ryan2
1.Graduate Entry Medical School University of Limerick
2.Barrington’s Hospital, Limerick.
Abstract
Aim
To evaluate thyroid nodules and to determine the incidence of thyroid cancer.
Methods
This retrospective cohort study collected data from ten patients who presented with thyroid nodules to Barrington’s Hospital Limerick. Ultrasound/FNA results of thyroid nodules were used to measure the incidence of thyroid cancer.
Results
The number of thyroid nodules diagnosed as malignant was significantly greater than benign nodules (***p-value <0.0004, 95% confidence interval (-1.109 to -0.399)). This data indicates that females are more likely to develop thyroid cancer than males.
Discussion
The incidence of thyroid cancer is growing at a rapid pace. Papillary carcinoma is the most common thyroid cancer diagnosed. Notably, it is the most likely diagnoses in impalpable thyroid nodules. Females are more likely to develop thyroid cancer than males.
Introduction
Thyroid cancer is one of the most prevalent solid tumour types throughout the world. Studies show a rising incidence, particularly in women (1). Tumours which were 2cm (or smaller) accounted for 87% of the increased numbers of cancer discoveries. Despite an earlier diagnosis, there was no change in mortality (2). The increase is largely attributable to small papillary thyroid cancers (3). Evidence has shown that monitoring documented small papillary cancers without surgery can be performed safely for long periods of time (4). Advancements and increased availability in easily accessible, sensitive diagnostic imaging have contributed to the quoted increased incidence figures. These include thyroid ultrasound as well as ultrasound guided Fine Needle Aspiration (FNA). This raises concern for clinical over-diagnosis. In addition, this emphasises the importance of having evidence-based guidelines to influence clinical management of thyroid nodules. Without clear benefit to patients, the management of low risk cancers has caused significant expenditure in the health care sector. A resulting backlash against the early detection of thyroid cancer followed. The latest American Thyroid Association (ATA) guidelines for the management of adult patients with thyroid nodules and differentiated thyroid cancer differ from those previously published. Of note, the guidelines highlighted the over-diagnosis and overtreatment of a disease which is usually slowly progressive. Furthermore, it has been queried that treatment related morbidity may pose a greater risk than benefit to patients (5).
The four guidelines (ATA, NCCN, BTA and AACE/ACE-AME) describe particular sonographic features of thyroid nodules. These features are then used to determine the risk of malignancy. Common features used are micro-calcifications, raised lesions, irregular borders, extra thyroidal extension, etc. The presence of such features aid in determining the need for FNA. In addition, clinical features are used to determine whether thyroid nodules should be investigated further. Family history is one such clinical feature which aids clinicians. It is suggested a family history of thyroid cancer may predict a more a disease which is more aggressive. However, further research to support this is required (6, 7). Guidelines also note that nodule size does not predict malignancy. However, three of the guidelines recognize that thyroid cancers smaller than 1 cm are unlikely to increase mortality risk (8). A summary of such guidelines state that FNA is recommended for nodules larger than 1cm which have sonographic features such as solid, hypoechoic, micro-calcifications, extra-thyroidal extension, irregular border and dimensions showing the nodule to have a greater height than width (9). The objective of this study was to evaluate thyroid nodules according to gender, age and size. The frequency of a malignant or benign diagnosis of nodules following FNA was also to be considered.
Methods
This retrospective cohort study collected data from ten patients who presented with thyroid nodules. Results of thyroid nodules obtained from ultrasound/FNA were used to measure the incidence of thyroid cancer. Data was obtained from patients who presented to the Endocrinology Department in Barrington’s Hospital Limerick. Data collected included patient sex, age, nodule size, histologic features, and staging.
Statistical analysis was preformed using Graph Pad Prism 7. P-values were estimated using unpaired T-test, two tailed, normal distribution. Trends in incidence of thyroid cancer among nodules were statistically analysed.
Results
A total of 10 patients with thyroid nodules were investigated using ultrasound guided fine needle aspiration. 8 patients were found to have malignant nodules while 2 patients had nodules classified as benign. The number of thyroid nodules diagnosed as malignant was significantly greater than benign nodules (p-value <0.0004, 95% confidence interval (-1.101 to -0.399)) (Figure1). The size of the malignant tumours identified varied from 0.08-3cm.
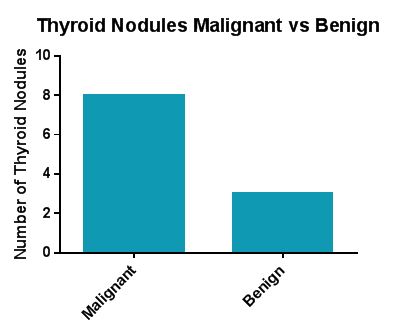 Figure 1. Thyroid Nodules Malignant vs Benign
Figure 1. Thyroid Nodules Malignant vs Benign
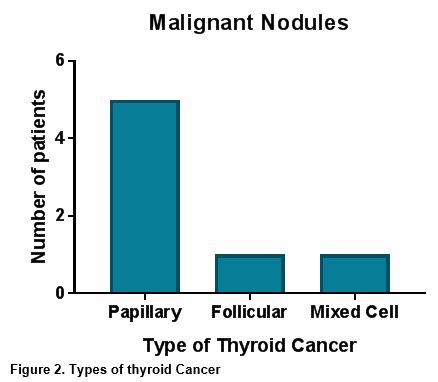
Papillary cancer represented the majority of malignant nodules, at 71% of the nodules identified. Other types of thyroid cancer reported included follicular and mixed cellular (Figure 2).
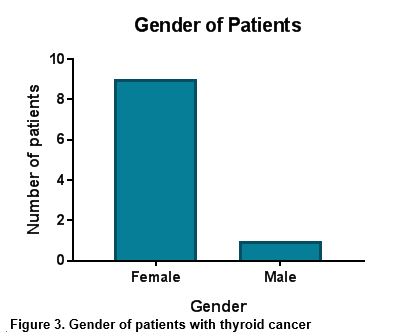
A total of 90% of patients were female (figure 3). The age range of patients varied from 32 to 76 years of age with median age of 60.
Discussion
Malignant nodules accounted for the majority of thyroid nodules examined by FNA; this is consistent with the increasing incidence of thyroid cancer worldwide. Detection rates of thyroid cancer has grown rapidly. Over the past three decades, a 240% increased incidence has been demonstrated (10). Recent research shows that sub-centimetre, and hence impalpable, thyroid cancers are growing at the greatest rate (2). The data in this study reflects this, showing malignant thyroid nodules varying from a sub-centimetre size of .08cm to 3cm. A thyroid nodule size of greater than 2 cm is associated with an increased risk of well-differentiated thyroid cancer. Larger nodules, if cancerous, carry a significantly greater likelihood of being follicular or Hurthle cell carcinomas (or other rare malignancies). This is in comparison with smaller nodules which are more commonly papillary carcinomas (11).
Papillary cancer was found to be the most frequent cancer diagnosed among the malignant thyroid nodules. This concurs with current statistics as the most common endocrine malignancy, accounting for 96.0% of total new endocrine cancers and 66.8% of deaths due to endocrine cancers(10). According to the World Health Organization, papillary carcinomas which measure 1.0cm or less are diagnosed as papillary thyroid micro-carcinomas(12). This is reflected in the data of this study as papillary cancers were reported to be between .08 cm and 1.1cm in size.
Radiation exposure to the thyroid gland in childhood as well as age, female sex, and family history are risk factors that increase the incidence of well-differentiated thyroid cancer. The majority of patients in this study were female. However, due to small population size it is not appropriate to draw significant conclusions regarding gender from this study. Existing literature states that over the past 35 years the absolute increase in thyroid cancer in women was almost 4 times greater than that of men(1). The peak incidence of thyroid cancer occurs in premenopausal women. This strongly suggests that female sex hormones may play a role in thyroid cancer pathophysiology(13). The selection of patients with thyroid nodules for FNA depended on nodule size (greater than 8mm), number of nodules (single nodules were considered higher risk of malignancy) and specific ultrasound features. Ultrasound parameters, such as microcalcifications, increased vascularity, irregular margins, have been traditionally associated with increased risk of malignancies. According to the ATA guidelines, a taller than wide shape in a thyroid nodule is a suspicious feature and should be investigated further by FNA (14). Whilst this study did not focus on the ultrasound features noted during examination, there is scope to consider this in future studies. The age profile of the patients studied varied from 32 to 68. Thyroid cancer can occur in any age-group but more so in adults aged 45 to 54 years, with a mean age of 50 years at diagnosis (15).
Detection rates of thyroid cancer are growing at a rapid pace. This is largely due to development and utilization of radiological tools allowing the diagnosis of previously undetectable thyroid nodules. The highest mortality rates are associated with papillary carcinomas. Notably, it is also the most likely diagnoses made when investigating impalpable sub-centimetre thyroid nodules. Gender analysis shows females are more likely to develop thyroid cancer than males. Increasing incidence and early diagnosis has not changed mortality rates of thyroid cancer. Therefore, a review of current guidelines may be reasonable to avoid the over-diagnosis and over-treatment of thyroid nodules.
Conflict of Interest
The authors have no conflict of interest in relation to the subject matter in this manuscript.
Correspondence:
Aoife Gilmartin,
Graduate Entry Medical School
University of Limerick
Email: [email protected]
References
1. Davies L, Welch HG. Current thyroid cancer trends in the United States. JAMA otolaryngology-- head & neck surgery. 2014;140(4):317-22. 2. Hoang JK, Choudhury KR, Eastwood JD, Esclamado RM, Lyman GH, Shattuck TM, et al. An exponential growth in incidence of thyroid cancer: trends and impact of CT imaging. AJNR American journal of neuroradiology. 2014;35(4):778-83. 3. Tufano RP, Noureldine SI, Angelos P. Incidental thyroid nodules and thyroid cancer: considerations before determining management. JAMA otolaryngology-- head & neck surgery. 2015;141(6):566-72. 4. Ito Y, Miyauchi A, Inoue H, Fukushima M, Kihara M, Higashiyama T, Tomoda C, Takamura Y, Kobayashi K, Miya A. An observational trial for papillary thyroid microcarcinoma in Japanese patients. World journal of surgery. 2010;34(1):28-35. 5. Kitahara CM, Sosa JA. The changing incidence of thyroid cancer. Nature reviews Endocrinology. 2016;12(11):646-53. 6. Naing S, Collins BJ, Schneider AB. Clinical behavior of radiation-induced thyroid cancer: factors related to recurrence. Thyroid : official journal of the American Thyroid Association. 2009;19(5):479-85. 7. Pinto AE, Silva GL, Henrique R, Menezes FD, Teixeira MR, Leite V, Cavaco BM. Familial vs sporadic papillary thyroid carcinoma: a matched-case comparative study showing similar clinical/prognostic behaviour. European journal of endocrinology. 2014;170(2):321- 8. Jeon MJ, Kim WG, Choi YM, Kwon H, Lee YM, Sung TY, Yoon JH, Chung KW, Hong SJ, Kim TY, Shong YK, Song DE, Kim WB. Features Predictive of Distant Metastasis in Papillary Thyroid Microcarcinomas. Thyroid : official journal of the American Thyroid Association. 2016;26(1):161-8. 9. Nabhan F, Ringel MD. Thyroid nodules and cancer management guidelines: comparisons and controversies. Endocrine-related cancer. 2017;24(2):R13-r26. 10. Carling T, Udelsman R. Thyroid cancer. Annual review of medicine. 2014;65:125-37. 11. Kamran SC, Marqusee E, Kim MI, Frates MC, Ritner J, Peters H, Benson CB, Doubilet PM, CIbas ES, Barletta J, Cho N, Gawande A, Ruan D, Moore EF Jr, Pou K, Larsen PR, Alexander EK. Thyroid nodule size and prediction of cancer. The Journal of clinical endocrinology and metabolism. 2013;98(2):564-70. 12. Bradley NL, Wiseman SM. Papillary thyroid microcarcinoma: the significance of high risk features. BMC cancer. 2017;17(1):142. 13. Moleti M, Sturniolo G, Di Mauro M, Russo M, Vermiglio F. Female Reproductive Factors and Differentiated Thyroid Cancer. Frontiers in endocrinology. 2017;8:111. 14. Kwak JY. Indications for fine needle aspiration in thyroid nodules. Endocrinology and metabolism (Seoul, Korea). 2013;28(2):81-5. 15. Nguyen QT, Lee EJ, Huang MG, Park YI, Khullar A, Plodkowski RA. Diagnosis and treatment of patients with thyroid cancer. American health & drug benefits. 2015;8(1):30-40.
P802
