Infliximab Induced Cardiac Tamponade
N. O’Morain*1, L. Kumar*1, C. O’Carroll-Lolait2, A. Alakkari1, B. Ryan1
1. Department of Gastroenterology & Clinical Medicine, Tallaght University Hospital/Trinity College Dublin, Dublin 24
2. Department of Cardiology, Tallaght University Hospital/Trinity College Dublin, Dublin 24
*Dr. O’Morain and Dr. Kumar contributed equally to this case report
Abstract
Aim
To report the first case of cardiac tamponade related to Infliximab induction therapy in an Ulcerative Colitis patient.
Methods
Review of published case reports.
Results
This complication was likely due to a type 3 hypersensitivity immune-complex reaction resulting in a reactive pericardial effusion
Discussion
Though rare, this case demonstrates how autoimmune reaction to anti-TNF𝛼 therapy can initially mimic infection, as our patient presented with tachycardia, hypotension, raised inflammatory and infective markers and fever.
Introduction
Biologic therapies are increasingly used in the treatment of Inflammatory Bowel Disease. Reactions to infusion therapy are not uncommon but are mostly benign and self-limiting. Rarely, life-threatening complications can occur.
Case Report
A 48-year-old biologic-naïve lady was admitted with acute severe Ulcerative Colitis, confirmed on sigmoidoscopy. Having failed IV steroids, rescue Infliximab therapy induced remission. ECG and serum troponin were requested to investigate an episode of chest pain post infusion, the results of which were normal. The patient was discharged home well following resolution of symptoms, with a plan to complete outpatient induction therapy. The patient re-presented, however, 6 days post-infusion with fevers, rigors, chest pain and exertional dyspnoea.
Image 1: Chest X-Ray pre and post first dose infliximab infusion.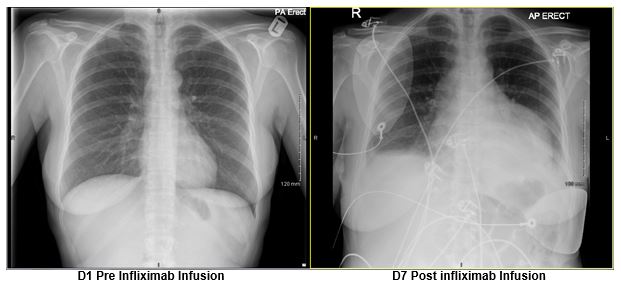
Initial investigations raised the suspicion for sepsis with raised inflammatory markers (CRP 208mg/L, Thrombocytosis 652 x109/L) and a leukocytosis (WCC 13.4 x109/L). Hypotension and tachycardia were treated with IV fluids and antibiotics. Abdominal imaging and Sigmoidoscopy showed quiescent colitis. Chest X-Ray demonstrated blunted costophrenic angles and cardiomegaly (Image 1). ECG showed widespread ST elevation with raised troponin (64ng/L). An urgent cardiology review prompted a bedside echocardiogram which revealed a large circumferential (3cm) pericardial effusion with normal LVF (Image 2). Care was transferred to the CCU due to persistent haemodynamic instability.
The admission was further complicated by episodes of fast atrial fibrillation requiring intravenous amiodarone. Coronary angiogram, tuberculosis and autoimmune screens were negative. Serial echocardiograms, chest x-rays and ECGs did not show any deterioration or evidence of tamponade. The patient stabilized over the course of 2 weeks with antibiotics, antiviral treatment and slow diuresis and the patient was discharged home. The patient re-presented 2 weeks later with progressive dyspnoea. At this point, echocardiogram established cardiac tamponade, requiring urgent pericardiocentesis. Fluid analysis displayed elevated LDH and inflammatory cells, in keeping with a reactive picture. The patient stabilized and improved with gentle diuresis. Close outpatient monitoring did not demonstrate any further recurrence or persistent cardiac dysfunction. Infliximab therapy has been abandoned.
Image 2: Apical 4 chamber view showing global circumferential large pericardial effusion. Pulse wave Doppler of tricuspid valve inflow showing no significant amount of tricuspid valve inflow variation with respiration.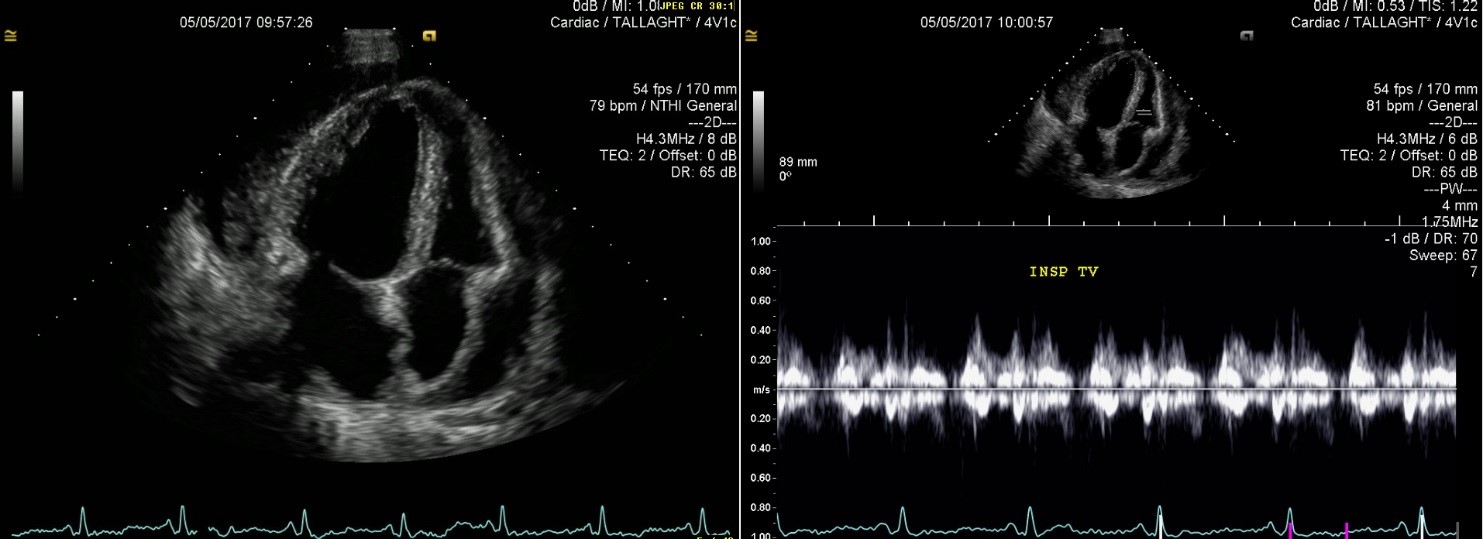
Discussion
Biologic agents are increasingly used therapies in the treatment of auto-immune conditions, including inflammatory bowel disease (IBD). Serious infectious and immunogenic adverse reactions occur in an estimated 5% of patients receiving anti-TNF alpha therapy (ATT)1. Pericardial complications have been reported in both adult and paediatric Crohn’s populations receiving ATT1,2, and more recently in a paediatric Ulcerative Colitis patient3. Pericardial effusion with cardiac tamponade has previously been described in patients with rheumatoid arthritis receiving Adalimumab (ADA) or Infliximab (IFX) therapy4-7. It has been suggested that this complication arises due to the severity of disease and extra-articular manifestations, of which pericarditis is common. More common causes of pericardial effusion in this setting, and important to exclude, are TB pericarditis, drug induced lupus erythematosus (DILE), or exacerbation of heart failure by Infliximab.
Here we present the first reported case of pericardial effusion with tamponade in an adult patient with Ulcerative Colitis receiving IFX. Our patient had recently diagnosed pancolitis which had responded well to first line therapies including aminosalicylates and oral steroids. An acute severe flare did not respond to systemic intravenous steroids and prompted escalation of therapy to a biologic agent, which was well tolerated. A seemingly innocuous episode of chest pain post-infusion, with normal troponin and ECG, did not prompt any further investigation and the patient was discharged. However, this may well have heralded the development of cardiac effusion and subsequent tamponade.
Most patients presenting with pericardial effusion due to biologic therapy have either Rheumatoid Arthritis (RA) or develop a drug-induced lupus erythematosus (DILE). Our patient had negative autoimmune screen including ANA, rheumatoid factor, anti-CCP prior to, and after the development of pericardial effusion. The pathophysiology of infliximab‐induced pericarditis is not well understood however direct cardiac toxicity, IgE‐mediated allergic reaction, humoral antibody response and cell‐mediated hypersensitivity delayed reaction have been suggested as possible mechanisms8. We posit that this complication was likely as a result of the high inflammatory burden due to the acute flare of Ulcerative Colitis and the high titers of Infliximab following the infusion, and may therefore represent a type 3 hypersensitivity immune-complex reaction resulting in a reactive pericardial effusion due to supratherapeutic drug levels. Pericardial effusion/tamponade is a rare side effect of Infliximab therapy. Though rare, this case demonstrates how autoimmune reaction to anti-TNF𝛼 therapy can initially mimic infection, as our patient presented with tachycardia, hypotension, raised inflammatory and infective markers and fever. It is important to consider non-infective causes of similar presentations. Initial investigations for post-infusion chest pain should include a chest x-ray, with a low threshold for serial investigations. Our patient did not develop any long term cardiac dysfunction and had a normal follow up Echocardiogram. Good disease control has been maintained with oral mesalazine. While reported evidence is limited, subsequent treatment with an integrin inhibitor (i.e. Vedolizumab) for disease flares has been successful in patients with previous Infliximab–induced pericardial effusions1 and remains a potential treatment option for this patient.
Conflicts of Interest Statement
The authors have no conflicts to declare.
Corresponding Author
Dr. Neil O’Morain,
Department of Gastroenterology & Clinical Medicine,
Tallaght University Hospital,
Dublin 24.
Tel: 0861048627
Email: [email protected]
References
1. Naseer M, Kulairi Z, Kam M. Cardiac Tamponade as a Presenting Manifestation of Infliximab-Induced Lupus in Patient Treated for Crohn’s Disease. ACG Case Reports Journal. 2017;4:e1. doi:10.14309/crj.2017.1.
2. Burke JP, Kelleher B, Ramadan S, Quinlan M, Sugrue D, O'Donovan MA. Pericarditis as a complication of infliximab therapy in Crohn's disease. Inflammatory Bowel Disease. 2008 March;14(3):428-9.
3. Dipasquale V, Gramaglia SMC, Catena MA, Romano C. Pericarditis during infliximab therapy in paediatric ulcerative colitis. J Clin Pharm Ther. 2018;43:107–109
4. Hakan Ozkan, Ahmet Seckin Cetinkaya, Tekin Yildiz, and Tahsin Bozat, “A Rare Side Effect due to TNF-Alpha Blocking Agent: Acute Pleuropericarditis with Adalimumab,” Case Reports in Rheumatology, vol. 2013, Article ID 985914, 2 pages, 2013. doi:10.1155/2013/985914
5. Manuel José Fernández, Anguita Laura, Cejudo Díaz, del Campo Virgilio, Martínez Mateo. Cardiac tamponade. A complication of treatment with infliximab. Medicina Clínica, Volume 149, Issue 5 2017
6. Henry D. Lather and J. Michelle Kahlenberg. Haemorrhagic Pericardial Effusion with Tamponade: A Rare Adverse Effect of Infliximab—Case Report and Literature Review. Case Reports in Rheumatology 2016
7. M. H. Edwards, A. M. Leak . Pericardial effusions on anti-TNF therapy for rheumatoid arthritis—a drug side effect or uncontrolled systemic disease? Rheumatology, Volume 48, Issue 3, 1 March 2009, Pages 316–317
8. Kiyomatsu H, Kawai K, Tanaka T,Kiyomatsu T, Nozawa H, Kanazawa T, Kazama S, Ishihara S, Yamaguchi H, Sunami E, Watanabe T. Mesalazine induced pleuropericarditis in a patient with Crohn's disease. Intern Med. 2015;54:1605-1608.
P902
