More Teaching – Not More Exams: Interns’ Views in Improving Prescribing Safety
M.P. O’Shea1, K. Harkin2, H.M. Sulaiman3, M. Hennessy1, M. Barry1, C. Kennedy1
1. TCD Department of Clinical Pharmacology, Dublin
2. Inchicore Family Doctors, Dublin
3. Trinity College Dublin School of Medicine
Dear Sir,
Newly graduated doctors (interns) must become accustomed to a number of challenging tasks in their first year as prescribers. Prescribing in the inpatient setting by interns is very common in Ireland, and is a known source of iatrogenic risk to patients1.
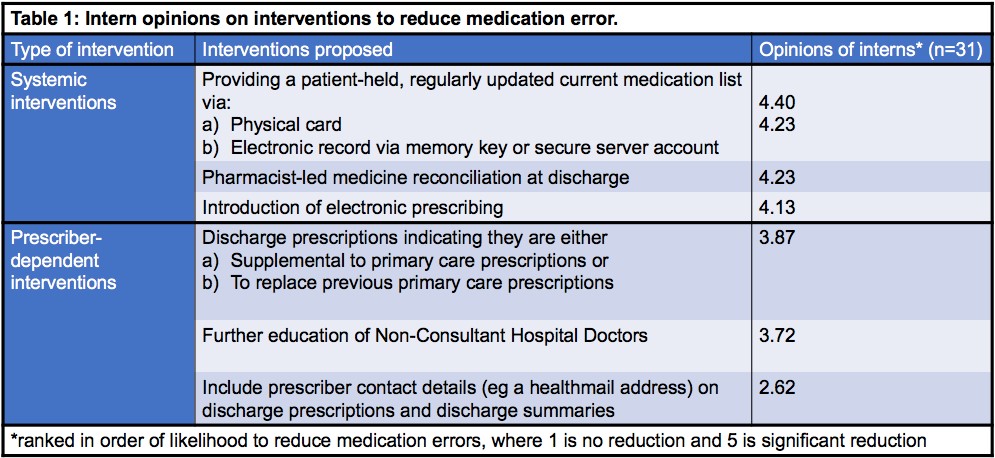
Interventions to address this can be categorized as prescriber-dependent (eg traditional didactic teaching, and formative or summative assessments), or systemic (eg use of patient held medication lists, medicine reconciliation at discharge, electronic medical records). Several educational interventions have been validated to address this issue, but evidence is limited to once-off interventions which do not adequately assess clinical outcomes2. We believe these interventions should target transition of care, a moment of particular vulnerability in the patient care pathway1.
We conducted a mixed method survey of interns in Saint James’s Hospital (SJH) (January 2018). Qualitative components included open questions, evaluated using thematic analysis. Quantitative components included questions with Likert scale responses. Paired sample 2-tailed t-test was used to compare items scored on Likert scales. The survey was conducted at an intern teaching session. Approval to conduct this survey was obtained as per hospital protocol.
Thirty-one interns took part in the survey (93.94%, n=33). Interns were asked to rank their preferences for six interventions to reduce medication errors (see table 1). Systemic interventions were viewed as significantly more likely to reduce prescription error rates compared to prescriber-dependent interventions (p=0.005, n=26). Patient-held medication lists were considered most likely to reduce prescribing errors.
Most interns (83.87%) were satisfied with their ability to complete prescriptions and discharge summaries, while 72.41% agreed that training on discharge prescribing was adequate. Most interns (90.32%) agreed they would like further pharmacology teaching as part of intern year. Many (56.67%) disagreed that a prescribing safety exam at the end of intern year would improve patient care. When considering the prescribing environment, 70.97% of interns agreed or strongly agreed that, if they are unfamiliar with a patient, they can discuss their care with someone who is more familiar with their care.
With regard to qualitative outcomes, interns were asked to indicate why they thought errors occurred at discharge. On thematic analysis, time pressure and fatigue were highlighted for all errors, while human factors (including handwriting and inexperience) were highlighted for a number of error types. Access to information on charges was highlighted as a cause for communication errors at discharge.
Systemic changes are preferred by interns to prescriber-dependent changes. Such changes would address issues described in the qualitative component of the survey. Introduction of electronic prescribing to SJH in October 2018 may reduce identified sources of errors, including eliminating handwriting errors, and improving access to the complete patient file.
With regard to prescriber-dependent interventions, participants suggested that further pharmacology education would improve prescribing, whereas a prescribing safety exam would not. As a summative assessment appears to be undesirable, and passive teaching doesn’t improve clinical outcomes, there may be a role for formative assessments in conjunction with a didactic curriculum3,4.
Corresponding Author
Michael P. O’Shea
TCD Department of Clinical Pharmacology, Dublin
Email: [email protected]
References
1. O’Shea MP, Kennedy C. Quantifying discharge prescription omission error in an irish university teaching hospital Pharmacology 2017; 231P London, UK: pA2Online; 2017.
2. McCarthy RM, Hilmer SN. Teaching Junior Medical Officers safe and effective prescribing. Internal medicine journal. 2013;43(11):1250-3.
3. Mansouri M, Lockyer J. A meta-analysis of continuing medical education effectiveness. The Journal of continuing education in the health professions. 2007;27(1):6-15.
4. Ross S, Loke YK. Do educational interventions improve prescribing by medical students and junior doctors? A systematic review. Br J Clin Pharmacol. 2009;67(6):662-70.
P943
