Operative Management of Perinatal Lumbar Disc Herniation and Cauda Equina Syndrome: A Case Series
DP Ahern1, D Gibbons2, M Dodds1, M Timlin1, N Cassidy1, S Morris1, K Synnott1, JS Butler1,2
1. National Spinal Injuries Units, Department of Trauma & Orthopaedic Surgery, Mater Misericordiae University Hospital, Dublin, Ireland.
2. Spine Service, Department of Trauma & Orthopaedic Surgery, Tallaght University Hospital, Dublin, Ireland.
Abstract
Introduction
Perinatal lumbar discectomy for lumbar disc herniation or cauda equina syndrome is a rare clinical scenario. This case series outlines the surgical management of this clinical scenario at a national tertiary referral centre over a 10-year period
Methods
A retrospective review of all females who underwent discectomy / decompression for lumbar disc herniation or cauda equina syndrome in the perinatal period at a national tertiary referral centre for spine surgery over a 10-year period between January 2008 to December 2017.
Results
6 cases required surgical intervention. All patients were successfully managed with surgical decompressive procedures and recovered well in the postoperative period without complication.
Conclusions
The principles of management remain the same in the pregnant and non-pregnant populations, although treatment options are complicated by the desire to avoid risk to the developing foetus. Surgical intervention is safe to both mother and baby and if performed promptly is associated with an excellent functional outcome.
Keywords
Cauda Equina Syndrome, Lumbar disc herniation, discectomy, pregnancy, non-obstetric surgery
Introduction
Lower back pain is a frequently encountered symptom in pregnancy1. Symptomatic lumbar disc herniation is reported as the cause of lower back pain in pregnancy in approximately 1:10,0002. Cauda equina syndrome (CES) is a rare but potentially devastating condition, capable of causing profound irreversible neurological deficits and is considered one of the few spine surgical emergencies3. A herniated lumbar disc is frequently the cause of CES, causing compression, with subsequent dysfunction, of the lumbar and sacral nerve roots4.
Spinal surgery in the pregnant population poses technical challenges and is generally reserved for emergency cases. Non-obstetric surgery in the pregnant patient is uncommon, with a reported incidence of 1-2% of pregnancies5. Furthermore, the rarity of CES, with a 1-2% incidence in those undergoing surgery for lumbar disc herniation, makes this an uncommon scenario encountered in clinical practice6. As a result, there is a paucity of literature pertaining to this topic. This study describes the surgical management of this uncommon but potentially devastating clinical scenario at a national tertiary referral centre over a 10-year period.
Methods
The National Spinal Injuries Unit (NSIU) at Mater Misericordiae University Hospital, Dublin, is the national tertiary referral centre for all spine pathology in the Republic of Ireland. The NSIU database generated all cases of women of childbearing age who underwent lumbar discectomy or decompression during the period of January 2008 to December 31st 2017.
The study inclusion criteria were women who had undergone lumbar discectomy or decompression for herniated lumbar disc disease or cauda equina syndrome while pregnant or in the postpartum period. A total of 6 cases were identified and the medical records and imaging of these cases were reviewed.
The neurologic assessment of the study group included the power grading system set out by the American Spinal Injuries Association (ASIA) Impairment Scale (Table 1.)
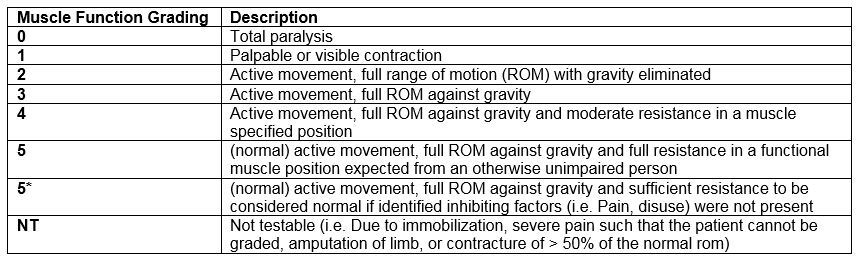
Table 1. Muscle Function Grading adopted from the ASIA Impairment Scale.
Results
Case A
A 33 year old female at 5 weeks gestation, was transferred from a peripheral hospital with suspected cauda equina syndrome. She reported an initial 4-week history of mid-thoracic back pain, precipitated by carrying a heavy load. Over the subsequent two months, her pain migrated to her low back with increased severity and was accompanied by left lower limb radiculopathy. She then presented with a two-week history of left lower limb weakness and a two-day history of urinary retention and saddle anaesthesia. Following transfer, her physical examination was notable for 1/5 power in the left S1 myotome, with absent sensation to both pin-prick and light touch sensation from the S1 to S4-5 dermatomes. She had no voluntary anal contraction. Her reflexes were normal. MRI demonstrated a large L5-S1 paracentral disc herniation, with prolapse indenting the thecal sac and compressing the left S1 nerve root.
This patient underwent an L5/S1 discectomy under general anaesthetic. The procedure was performed in the prone position, where a left lateral laminectomy and discectomy was performed without complication. She recovered well postoperatively with complete resolution of her motor and sensory neurologic deficits. No urinary retention was noted on serial post-void residual bladder scans and she was discharged home on postoperative day 4. She was reviewed in the outpatient setting at 6 weeks following surgery, with no complications relating to surgery or pregnancy identified.
Case B
A 29 year old female, at 36 weeks’ gestation, was transferred from a maternity hospital with a 6-hour history of new-onset lower limb motor weakness, urinary and faecal incontinence and suspected acute cauda equina syndrome. Her symptoms began 6 hours earlier when receiving antenatal care. Her background history was significant for an L4/L5 discectomy four years prior for symptomatic lumbar disc herniation. Her physical examination was notable for 1/5 power in the L5-S1 myotomes, and 1/2 sensation in the L5-S1 dermatomes. She had absent perineal sensation at S4-S5 and absent voluntary anal contraction. An MRI spine demonstrated a recurrent L4/L5 disc extrusion, with caudal migration and an L5/S1 disc protrusion and canal stenosis.
With the combined clinical and MRI findings the decision was made following discussion with obstetrician, anaesthetist and patient to proceed to revision L4-S1 posterior lumbar decompression, including an L5 laminectomy, foraminotomy and L5/S1 discectomy under general anaesthetic in the left lateral decubitus position. Postoperatively, the patient experienced uterine contractions and the decision was made to proceed to Caesarean Section. A healthy baby girl was delivered. Both patient and baby had an uncomplicated recovery, with complete resolution of the patient’s neurology.
Case C
A 36 year old female was transferred from a maternity hospital with symptoms suggestive of acute cauda equina syndrome, four days following a Caesarean Section for her third pregnancy. She had a longstanding history of lower back pain with bilateral lower limb radiculopathy. She described an acute worsening of her radicular pain following her Caesarean section, which initially settled but subsequently returned with associated bilateral lower limb weakness, urinary retention and saddle anaesthesia.
The physical examination was remarkable for bilateral 2/5 power in bilateral L5 myotomes, with 1/2 sensation in bilateral L5 dermatomes. MRI demonstrated a large disc prolapse at L4/L5 causing significant canal stenosis. She subsequently underwent an L4/L5 discectomy without immediate postoperative complication. Postoperatively, she experienced a persistence of lower limb weakness and urinary dysfunction, with raised post-void residuals requiring intermittent self-catheterisation. At 6 weeks postoperatively she reported resolution of her neurological dysfunction.
Case D
A 31 year old female presented with worsening lower back pain and progressive lower limb weakness and paraesthesia, seven days post-partum, following a normal vaginal delivery. Her background history was notable for a lumbar L5/S1 disc prolapse one year prior following a road traffic accident, which was managed conservatively. She described a three-day history of worsening back pain, right lower limb radiculopathy, constipation and urinary hesitancy.
On examination she had 3/5 power in her S1 myotomes, with 1/2 sensation in the S1 – S5 dermatomes. A post-void bladder ultrasound confirmed urinary retention. She had absent anal sensation and no voluntary anal contraction. An MRI scan demonstrated a large right-sided paracentral disc prolapse at L5/S1(See Figure 1.). She underwent an L5/S1 discectomy. Persistence of her saddle anaesthesia and urinary dysfunction was noted postoperatively. At 6 weeks postoperatively, she was neurologically normal, with full 5/5 power throughout the myotomes of her lower limbs bilaterally and intact 2/2 sensation throughout the dermatomes of her lower limbs bilaterally. Although her bladder function had not fully recovered by 6 weeks, it had recovered at 12 weeks following surgery.
Case E
A 37 year old woman who was 12 weeks’ gestation on her third pregnancy, was admitted from the outpatients clinic with a recurrent herniated L4/L5 disc prolapse. Her background history was significant for an L4/L5 discectomy two years prior. She was investigated for recurrence of her severe radicular pain and associated episodes of urinary and faecal incontinence. Her physical examination was remarkable for 4/5 power in her L5 myotome. Anal examination was normal. An MRI scan performed revealed a large left paracentral disc herniation at L4/L5.
In consultation with obstetrics/gynaecology the decision was made to undergo discectomy. This was performed successfully and without postoperative complications to either the mother or foetus. The patient had made a full functional recovery at 6 weeks post-operative clinical review.
Case F
A 32 year old woman, at 16 weeks’ gestation, was transferred from a peripheral hospital with an acute history of severe back pain, left lower limb radiculopathy and saddle anaesthesia that was precipitated by lifting her 11 month old son. Her pregnancy had been normal and her medical history was unremarkable. Her physical examination was notable for 1/2 sensation in her left S1 dermatome and saddle area, with absent voluntary anal contraction. An MRI scan demonstrated a large sequestrated disc at L5/S1, extruded caudally and causing significant thecal sac and S1 nerve root compression.
Due to patient concerns regarding surgery during pregnancy, the patient initially declined operative intervention. She subsequently developed urinary retention on day 1 of admission and the decision was made to proceed to L5/S1 discectomy. This was performed under general anaesthetic in the prone position and without complication. At 6 weeks postoperatively her resolving paraesthesia was limited to S3 area and her urinary dysfunction had completely resolved.
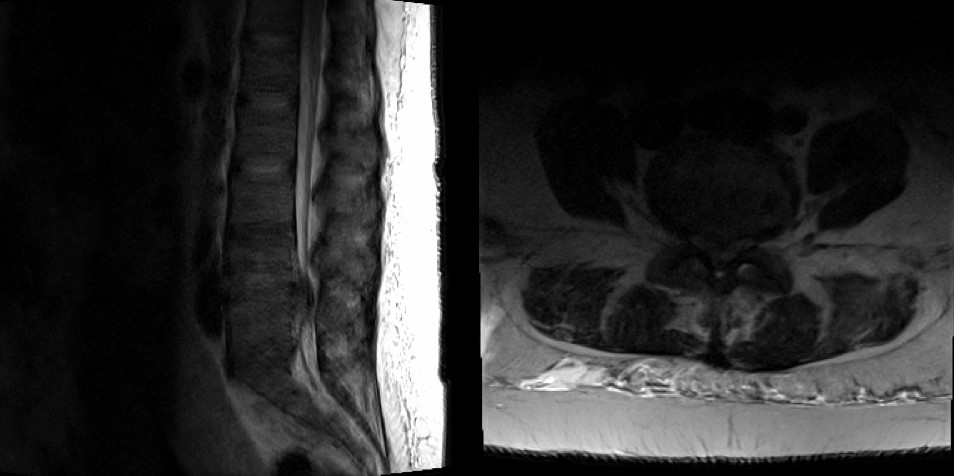
Figure 1. MRI images of Case D showing a large right-sided L5-S1 paracentral disc herniation.
Discussion
This case series describes the varying presentation of patients who underwent lumbar discectomy and/or decompression surgery at the various stages of pregnancy, from the first trimester through to the post-partum period.
Although uncommon, current evidence suggests that non-obstetric surgery is generally safe to both mother and foetus5. The indications for operative intervention for symptomatic acute lumbar disc herniation remain the same for both the pregnant and non-pregnant populations7. Acute, severe or progressive neurological deficit or CES constitute absolute indications for urgent surgical intervention. Relative indications for surgical intervention include intractable pain despite conservative measures. 90% of acute attacks of acute lumbar radiculopathy resolve spontaneously with non-operative measures, although evidence is lacking regarding the efficacy of individual conservative interventions8.
Providing adequate analgesia can prove difficult in the pregnant patient. Paracetamol remains the oral analgesic of choice for pregnant females, with non-steroidal anti-inflammatory and opiate medications contra-indicated due to a teratogenic risk to the developing foetus9. Selective nerve root blocks have been shown to provide effective short-term relief in lumbar radiculopathy, however these techniques require the use of fluoroscopy which carries a potential risk to the developing foetus10. Caudal corticosteroid epidural injections may provide short term analgesia with reduced radiation exposure11,12. Nevertheless, analgesic control in this population remains challenging.
In those without absolute indications, the timing of surgery is debatable. Surgical intervention within 6 months of onset is associated with superior outcomes13. Maternal mental distress, as a result of chronic severe pain, is associated with worse neonatal outcomes14. These proposed benefits must be balanced with the potential risk of inducing preterm labour as a result of the physiologic stress of surgery15. Overall, the risk of inducing labour appears proportional to the length of pregnancy, with third trimester pregnancies experiencing greatest risk16. These procedures should be performed with appropriate obstetric, paediatric and midwifery support available.
Spinal procedures, including microdiscectomy, the procedure of choice for lumbar disc herniation, require the use of intra-operative fluoroscopy which carries potential risk to the developing foetus17. However, the risk to the foetus appears small. Doses less than 100mGy are thought to pose a small risk and doses less than 50mGy are considered negligible18. A single lumbar spine fluoroscopic image carries an estimated dose of 3mGy to the developing foetus. Based on these calculations, judicious use of imaging appears low risk18.
The gravid uterus complicates patient positioning during lumbar discectomy19. The prone position is most commonly used in the non-pregnant population and is the position in which surgeons would be most comfortable. In the first and second trimesters, the prone position is considered safe with the use of the lateral decubitus position adopted for third trimester cases19,20. For these cases, the left lateral decubitus position should be used preferentially, regardless of the site of pathology, due to the risk of aortocaval compression when placed on the right lateral position. Use of the Relton-Hall laminectomy frame has also been proposed which avoids direct compression on the gravid uterus by placing posts on the upper sternum and iliac crests20,21.
Funding Statement
No funding
Conflicts of Interest
The authors declare no conflict of interest.
Corresponding Author
Daniel Patrick Ahern
National Spinal Injuries Unit,
Department of Trauma and Orthopaedic Surgery,
Mater Misericordiae University Hospital,
Dublin,
Ireland
Email: [email protected]
References
1. Fast A, Shapiro D, Ducommun EJ, Friedmann LW, Bouklas T, Floman Y. Low-back pain in pregnancy. Spine. 1987 May;12(4):368–71. 2. LaBan MM, Perrin JC, Latimer FR. Pregnancy and the herniated lumbar disc. Arch Phys Med Rehabil. 1983 Jul;64(7):319–21. 3. Spector LR, Madigan L, Rhyne A, Darden B, Kim D. Cauda equina syndrome. J Am Acad Orthop Surg. 2008 Aug;16(8):471–9. 4. Lavy C, James A, Wilson-MacDonald J, Fairbank J. Cauda Equina Syndrome. Obstetric Anesthesia Digest. 2010 Mar 1;30(1):16–7. 5. Balinskaite V, Bottle A, Sodhi V, Rivers A, Bennett PR, Brett SJ, et al. The Risk of Adverse Pregnancy Outcomes Following Nonobstetric Surgery During Pregnancy: Estimates From a Retrospective Cohort Study of 6.5 Million Pregnancies. Ann Surg. 2017 Aug;266(2):260–6. 6. Shapiro S. Cauda Equina Syndrome Secondary to Lumbar Disc Herniation. Neurosurgery. Oxford University Press; 1993 May 1;32(5):743–7. 7. Kapetanakis S, Giovannopoulou E, Blontzos N, Kazakos G, Givissis P. Surgical management for lumbar disc herniation in pregnancy. J Gynecol Obstet Hum Reprod. 2017 Dec;46(10):753–9. 8. Gibson JNA, Waddell G. Surgical interventions for lumbar disc prolapse: updated Cochrane Review. Spine. Spine; 2007 Jul 15;32(16):1735–47. 9. Niederhoff H, Zahradnik H-P. Analgesics during pregnancy. The American Journal of Medicine. Elsevier; 1983 Nov 14;75(5):117–20. 10. Pfirrmann CWA, Oberholzer PA, Zanetti M, Boos N, Trudell DJ, Resnick D, et al. Selective Nerve Root Blocks for the Treatment of Sciatica: Evaluation of Injection Site and Effectiveness—A Study with Patients and Cadavers. Radiology. Radiological Society of North America; 2001 Dec 1;221(3):704–11. 11. Dilke TFW, Burry HC, Grahame R. Extradural Corticosteroid Injection in Management of Lumbar Nerve Root Compression. Br Med J. British Medical Journal Publishing Group; 1973 Jun 16;2(5867):635–7. 12. Sehmbi H, D'Souza R, Bhatia A. Low Back Pain in Pregnancy: Investigations, Management, and Role of Neuraxial Analgesia and Anaesthesia: A Systematic Review. Gynecol Obstet Invest. 2017;82(5):417–36. 13. Sabnis AB, Diwan AD. The timing of surgery in lumbar disc prolapse: A systematic review. Indian J Orthop. 2014 Mar;48(2):127–35. 14. Liou S-R, Wang P, Cheng C-Y. Effects of prenatal maternal mental distress on birth outcomes. Women Birth. 2016 Aug;29(4):376–80. 15. Pike IL. Maternal stress and fetal responses: Evolutionary perspectives on preterm delivery. American Journal of Human Biology. Wiley Subscription Services, Inc., A Wiley Company; 2005 Jan 1;17(1):55–65. 16. Visser BC, Glasgow RE, Mulvihill KK, Mulvihill SJ. Safety and timing of nonobstetric abdominal surgery in pregnancy. Dig Surg. 2001;18(5):409–17. 17. Di Martino A, Russo F, Denaro L, Denaro V. How to treat lumbar disc herniation in pregnancy? A systematic review on current standards. Eur Spine J. Springer Berlin Heidelberg; 2017 Oct;26(Suppl 4):496–504. 18. McCollough CH, Schueler BA, Atwell TD, Braun NN, Regner DM, Brown DL, et al. Radiation Exposure and Pregnancy: When Should We Be Concerned? RadioGraphics. Radiological Society of North America; 2007 Jul 1;27(4):909–17. 19. Kathirgamanathan A, Jardine AD, Levy DM, Grevitt MP. Lumbar disc surgery in the third trimester – with the fetus in utero. International Journal of Obstetric Anesthesia. Elsevier; 2006 Apr 1;15(2):182. 20. Brown MD, Levi AD. Surgery for lumbar disc herniation during pregnancy. Spine. 2001 Feb 15;26(4):440–3. 21. Han I-H, Kuh S-U, Kim J-H, Chin D-K, Kim K-S, Yoon Y-S, et al. Clinical Approach and Surgical Strategy for Spinal Diseases in Pregnant Women: A Report of Ten Cases. Spine. 2008 Aug;33(17):E614–9.
P843
