Overnight Emergency CT Imaging: A 10-Year Experience at an Irish Tertiary Referral Hospital.
Hynes J1, Redmond CE1, Healy GM1, Cronin, J2, Heffernan, EJ1.
1Department of Radiology, St. Vincent’s University Hospital, Elm Park, Dublin, Ireland
2Emergency Department, Vincent’s University Hospital, Elm Park, Dublin, Ireland
Abstract
In recent years there has been increased utilisation of computed tomography (CT) imaging in developed countries, however there is a paucity of data regarding the utilisation of CT in the emergency overnight setting. We retrospectively analysed trends in ‘overnight’ (midnight to 8am) CT utilisation over a ten-year period at a single Irish tertiary referral hospital. Over the study period, we observed a significant increase in the proportion of CT imaging that was carried out overnight. There was no significant variation in the yield of pathological findings over the study period, which remained low (64% of CT studies were normal or had non-critical findings). The multiple factors which have contributed to the increased utilization of overnight emergency CT in recent years, the potential for reporting errors overnight and the implications therein for patient safety warrant consideration.
Introduction
The last two decades have witnessed an increase in the utilisation of Computed tomography (CT) imaging in the developed world1. This has been attributed to multiple factors; a greater availability of CT2, an ageing population3 and the increased complexity of modern medicine with an expansion of the clinical indications for CT4. CT plays an important role in emergency medical care, however concerns exist regarding the risk of fatigue-related error in CT reporting overnight and there is an observed association between increased overnight caseload and error rate5.
Most Irish radiology departments provide overnight emergency CT coverage with implicit challenges for staffing. Culleton et al6 recently reported on weekend CT activity in an Irish tertiary referral centre and observed a three-fold increase over 10 years. We hypothesised that recent significant practice change has also occurred with the usage of overnight emergency CT. The aim of our study is to retrospectively review the use of overnight emergency CT at an Irish tertiary hospital over a 10-year period.
Methods
All CT studies performed ‘overnight’ (i.e. between midnight and 8am) during the month of March each year from 2007-2016 were identified using the hospital’s Radiology Information System (RIS) and retrospectively reviewed. Our institution is a tertiary referral hospital which has an emergency department (ED) with annual attendance circa 52,000. The overnight emergency CT cover in our institution is provided by an off-site radiology registrar and a consultant radiologist. The CT protocol and findings were recorded and classified independently by three of the authors (JH, CR and GH) using a system based upon Royal College of Radiologists’ standards for the communication of findings7 - critical (e.g. ruptured abdominal aortic aneurysm), clinically significant/urgent (e.g. appendicitis) or normal/non-critical (e.g. pulmonary nodule). A group consensus was taken when discrepancies in the classifications existed. In order to compare overnight CT activity to overall departmental and hospital workload, the total number of CT examinations performed on each day and the monthly ED attendance figures were recorded as markers of overall radiology and hospital activity. Analysis of Variance (ANOVA) was performed to assess for trends, using SPSS version 22 (IBM, New York, USA) and an alpha of 0.05 considered statistical significance. The study was approved by the Institutional research board.
Results
Over the 10-year period studied, the mean number of CT studies performed per 24 hour period increased from 21.6 (SD 9.1) in 2007 to 47.6 (SD 17.3) in 2016 (p<0.001). The number of overnight CT studies increased, with the mean number of studies per night increasing from 0.4 (SD 0.8) to 1.2 (SD 1.1, p<0.001). When expressed as a proportion of total CT activity, overnight CT examinations accounted for 1.8% of studies in 2007, rising to 5.1% in 2015 and dropping to 2.5% in 2016, with a significant overall trend upwards during the study time period (p<0.001). The number of overnight CT studies per month peaked in 2014 and 2015 (73 for both years).
The mean monthly ED attendance over the ten year study period was 3755.5 (SD 415). Attendance remained static over the first seven years of the study, before significantly increasing in 2014 from a mean of 3508 (SD 113) during the period 2017-2013, to 4331 (SD 156) during 2014-2016 (p<0.001). This corresponded to the amalgamation of ED services from a nearby level 2 hospital into our institution in September 2013.
CT brain (including non-contrast, post-contrast and CT carotid/intracranial angiography) accounted for over two thirds of all overnight CT imaging (67.9%). Notably, CT intracranial angiography accounted for 24.3% of overnight studies in 2016, while this was rarely performed in previous years. CT abdomen was the second most commonly performed study, accounting for 20.8% of overnight CT imaging. The third most commonly performed study was CT thorax (including CT pulmonary angiogram [CTPA] and conventional CT thorax), accounting for 6.9% of overnight CT imaging. CT of the cervical spine accounted for 3.5% of overnight CT imaging.
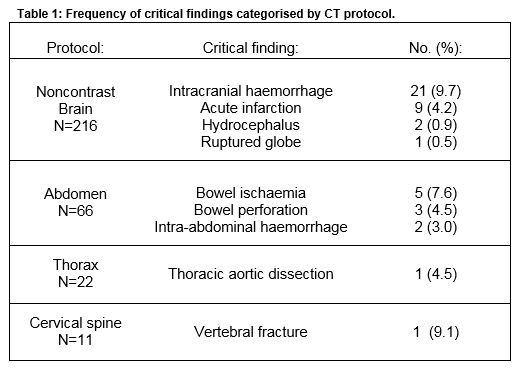
The yield of critical findings varied considerably during the study but there was no significant trend during the years of study and the average was 15.7% over the ten years. Overall 63.8% of CT studies were normal or had non-critical findings. Non-contrast CT brain had the lowest yield of pathological findings (15.3% critical and 7.9% clinically significant) of any protocol performed. Of the 216 CT brain studies performed, there were 33 (15.3%) studies with critical findings. All critical findings are outlined in Table 1. While 13 (68.4%) CTPA studies demonstrated a clinically significant result, for 11 of these cases the finding was present on the chest radiograph performed immediately prior to the CTPA; consolidation (n=6), pulmonary oedema (n=4) and pleural effusion (n=1). The two clinically significant findings not apparent on chest radiographs were a fourth order pulmonary embolus and a case of severe coronary artery disease.
Discussion
In this study, we have observed significant increases in both the overall CT activity, overnight CT activity and the proportion of examinations carried out overnight. The percentage of CTs performed overnight increased up to threefold in 2015 when compared to 2007 (5.1% vs 1.8% respectively). While a relative decline in overnight CT imaging was observed in 2016, it is noteworthy that the proportion of CT activity performed overnight in 2016 (2.5%) was still higher than five of the first six initial years of the study period. Despite this increased demand, there was no significant trend in the yield of critical or significant findings throughout the study period. We believe that this increase in the proportion of CT examinations carried out overnight reflects a change in working practice and therefore, the contributing factors and the potential implications warrant consideration. Overnight CT increased from 2.9% in 2013 to 5% in 2014, coinciding with both the incorporation of a nearby ED service into our hospital and the implementation of the European Working Time Directive (EWTD) at our institution.
There is little comparable evidence in the international literature on what constitutes an appropriate yield of findings from CT in the overnight setting. A Dutch series of over 1000 patients undergoing emergency abdominal CT yielded urgent findings in 57.9% of cases8, while 13.8% of patients had clinically signifcant pathologies in an analysis of emergency CT brain examinations in non-trauma patients9. It is important to recognise that these studies were not performed explicity in the overnight setting and that marked differences exist in what is considered an ‘urgent’ or ‘significant’ finding making any direct comparison difficult. ED attendance increased by 30% in March 2014, as services were transferred from a nearby level two institution. The increase was sustained in 2015 and 2016. While this undoubtedly contributed to the overall activity of the radiology department (and the hospital as a whole) the fact remains that the proportion of CT imaging carried out during the overnight period was on the increase prior to this event and continued afterwards, which confirms that this event was not the sole contributor to increasing the overnight CT workload.
The advent of new clinical pathways is also likely to have influenced overnight emergency CT practice. For example, following the publication of the ESCAPE trial10 a national referral pathway for mechanical thrombectomy for the management of acute ischaemic stroke was commenced. This requires suitable patients to undergo an urgent CT neck and intracranial angiogram, accounting for the large number of these studies performed in 2016. The updated NICE guidelines for non-contrast CT brain in head trauma published in January 201411 may have also played a role by mandating that head injured patients meeting certain criteria undergo imaging within one hour of injury and others, including anticoagulated patients, should undergo imaging within 8 hours of injury. It is difficult to establish whether the introduction of EWTD has had an impact on the utilization of overnight CT. EWTD has resulted in an end to the traditional 24-hour ‘on-call’ system of service provision with on-site doctors instead working blocks of shorter ‘night shifts’. This perhaps has resulted in an attitudinal change such that access to advanced diagnostics similar to that available during the normal working day is expected. The majority of research on the effect of EWTD on medical working practices to date has focused on its effect on the training and health of doctors with little investigation into its impact upon resource and staffing implications.
In the USA, a large survey of academic radiology departments demonstrated a direct correlation between the expansion of after-hours radiology and costs, as the majority provided either financial or "time off" incentives for the provision of overnight services12. Indeed with the introduction of EWTD in our institution, radiologists receive time off in lieu the next day for performing and interpreting overnight CT studies, thus presenting a challenge to normal daytime service delivery. However, while it was impossible to determine the exact proportion of requests for CT arising from the ED as opposed to inpatient teams in our study it is reasonable to expect that the majority of overnight activity would originate in the ED. The Emergency Department at our institution operated an EWTD-compliant roster long in advance of its introduction hospital-wide and so this wouldn’t be expected to have a significant impact.
ED overcrowding has been an increasingly topical issue in Irish healthcare in recent years. It is unlikely that overcrowding independently affects the utilization of advanced imaging, other than as a measure of increased hospital activity. Overcrowding occurs when insufficient ward beds are available to accommodate the number of admitted patients in a given hospital. Access to overnight CT does not create additional bed capacity. However additional CT access overnight could potentially expedite the discharge of patients who may be waiting until morning for non-emergent but clinically indicated investigations.
We observed differences in diagnostic yield between different CT modalities. Perhaps most interestingly the vast majority of pathology on CTPAs (85%) was present on a chest radiograph performed prior to the CTPA. The majority of patients presenting with pulmonary embolism (PE) are haemodynamically stable and may be empirically anticoagulated if there are no contraindications. Urgent CTPA is indicated in patients presenting with signs and symptoms of pulmonary embolism who are haemodynamically unstable or who have contraindications to anticoagulation13. We believe a study specifically examining the usage of CTPAs in the overnight setting may be worthwhile.
Occupational fatigue has been identified as an important contributor to error and poor decision making across a variety of industries, particularly in aviation14. In addition to the physical and cognitive fatigue common to all healthcare professionals, radiologists are prone to visual fatigue which is recognised as a source of diagnostic error15. While the provision of overnight emergency coverage is an important component of a radiology trainee’s education and development of autonomy, performing large quantities of examinations during the overnight period generates the potential for reporting error and adverse patient outcomes.
This study has several limitations. Our analysis was limited to the month of March of each year. We chose this month as we believed it would be less subject to seasonal variations in CT activity and reflect an accurate representation of the overall trend. We acknowledge that the classification system we adopted for the CT findings (critical, significant and normal/non-significant) may be susceptible to interobserver variability. It must be acknowledged that in certain circumstances (e.g. suspected stroke) a ‘normal’ CT brain is critical in determining suitability for further treatment. In conclusion, this study demonstrates a significant increase in the proportion of CT imaging performed overnight over a ten-year period at an Irish tertiary referral hospital. We postulate that the introduction of EWTD compliant working practices, local reconfiguration of ED services and new clinical pathways have contributed to this increase. Increasing the usage of overnight CT has implications on the staffing and resource allocation within Radiology Departments.
Conflict of Interest
No Conflicts of Interest declared
Correspondence:
Dr. John Hynes, Department of Radiology, St. Vincent’s University Hospital, Dublin 4, Ireland.
Email: [email protected]
Tel: +353 85 130 1477
References
1. Raja AS1, Ip IK, Sodickson AD, Walls RM, Seltzer SE, Kosowsky JM, Khorasani R. Radiology Utilization in the Emergency Department: Trends of the Past 2 Decades. American Journal of Roentgenology. 2014;203(2):355-360.
2. Sun, Zhonghua and Ng, Kwan-hoong and Vijayananthan, A. 2010. Is utilisation of computed tomography justified in clinical practice? Part 1: application in the emergency department. Singapore Medical Journal. 51 (3): pp. 200-206
3. The Irish Longitudinal Study on Ageing (TILDA). (2013) Patterns and Determinants of Health Care Utilisation in Ireland [Online]. Available from: http://www.thehealthwell.info/node/435786
4. Boland G, Guimaraes A, Mueller P. The radiologist’s conundrum: benefits and costs of increasing CT capacity and utilization. Eur Radiol. 2008;19(1):9-11.
5. Davenport M, Ellis J, Khalatbari S, Myles J, Klein K. Effect of Work Hours, Caseload, Shift Type, and Experience on Resident Call Performance. Academic Radiology. 2010;17(7):921-927.
6. Culleton, S, Torreggiani, W. Analysis of the last decade of weekend out-of-hours CT imaging: How have things changed? Irish Medical Journal 2014;107(3):77-79
7. The Royal College of Radiologists. Standards for the communication of critical, urgent and unexpected significant radiological findings, Second edition. London: The Royal College of Radiologists, 2012
8. Demchuk AM, Goyal M, Menon BK, Eesa M, Ryckborst KJ, Kamal N, Patil S, Mishra S, Almekhlafi M, Randhawa PA, Roy D, Willinsky R, Montanera W,Silver FL, Shuaib A, Rempel J, Jovin T, Frei D, Sapkota B, Thornton JM, Poppe A, Tampieri D, Lum C, Weill A, Sajobi TT, Hill MD. Endovascular treatment for Small Core and Anterior circulation Proximal occlusion with Emphasis on minimizing CT to recanalization times (ESCAPE) trial: methodology. Int J Stroke. 2014;10(3):429-438
9. National Institute for Health and Care Excellence (2014) Head injury: assessment and early management. NICE guideline CG176
10. Laméris W1, van Randen A, van Es HW, van Heesewijk JP, van Ramshorst B, Bouma WH, ten Hove W, van Leeuwen MS, van Keulen EM, Dijkgraaf MG,Bossuyt PM, Boermeester MA, Stoker J. Imaging strategies for detection of urgent conditions in patients with acute abdominal pain: diagnostic accuracy study. BMJ. 2009;338(jun26 2):b2431-b2431.
11. Wang X, You J. Head CT for Nontrauma Patients in the Emergency Department: Clinical Predictors of Abnormal Findings. Radiology. 2013;266(3):783-790.
12. Sellers A, Hillman B, Wintermark M. Survey of After-Hours Coverage of Emergency Department Imaging Studies by US Academic Radiology Departments. Journal of the American College of Radiology. 2014;11(7):725-730
13. French A. Clinical Characteristics of Patients with Acute Pulmonary Embolism: Data from PIOPED II. The Journal of Emergency Medicine. 2008;34(4):491)
14. Helmreich R. On error management: lessons from aviation. BMJ. 2000;320(7237):781-785
15. Krupinski E, Berbaum K, Caldwell R, Schartz K, Kim J. Long Radiology Workdays Reduce Detection and Accommodation Accuracy. Journal of the American College of Radiology. 2010;7(9):698-704
P669