A Cluster of Paediatric Invasive Group A Streptococcal and Chicken Pox Infections
C Ó Maoldomhnaigh, K Butler, P Gavin.
Paediatric Infectious Disease Department, Children’s University Hospital, Temple Street, Dublin 1.
Abstract
An increase in invasive group A streptococcus (GAS) cases referred to the paediatric infectious disease (PID) department of the Children’s University Hospital (CUH), Temple Street, prompted review of all invasive GAS cases in 2016. All of the 10 cases identified occurred over a 16-week period from February to June, of which 6 (60%) required admission to the paediatric intensive care unit. The median length of stay was 21.5 days. Seven had active chickenpox infection at diagnosis. This study highlights the significant morbidity of invasive GAS in children in Ireland. Most cases were associated with a vaccine preventable illness, which should prompt reappraisal of the absence of varicella vaccine from the national immunisation schedule in Ireland.
Introduction
Group A streptococcus (GAS) causes a variety of acute clinical syndromes from pharyngitis and scarlet fever commonly seen in primary care to more severe life-threatening invasive disease. Invasive GAS, categorised into three groups - necrotising fasciitis, streptococcal toxic shock syndrome and sepsis with or without an identifiable source of infection- is a notifiable disease to the Health Protection Surveillance Centre (HPSC)1. Laboratory criteria for a confirmed case require isolation of GAS from a normally sterile site. The HPSC previously reported a marked increase in the incidence of invasive GAS infections from 1.65/100,000 population in 2011 to 3.65/100,000 in 20132. The increased incidence was notable also for a 300% increase in the proportion of invasive GAS cases in children. After a slight decrease in incidence in 20153 (2.3/100000), we noted a cluster of invasive GAS cases referred to the paediatric infectious disease (PID) department of Children’s University Hospital (CUH), Temple Street, in 2016. We sought to further characterise this cluster of paediatric invasive GAS infections.
Methods
All referrals to the PID service in CUH are recorded on an electronic database that includes diagnosis and causative organism. This database was searched for any cases involving GAS infection in 2016. Invasive GAS infection was defined as per the HPSC. Cases that did not fit criteria for invasive disease were excluded. A medical chart review was carried out for all patients with invasive GAS and data collected on patient demographics, clinical presentation and hospital course.
Results
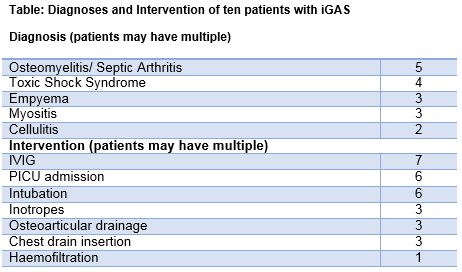
Sixteen patients were referred to the PID service in CUH in 2016 with GAS infection, of whom 10 fulfilled criteria for invasive disease and are included in this analysis. All 10 cases occurred over a 16-week period from February to June. Median age was 2.5 years (range, 0.8 - 3.9yrs) and 5 were male. All were previously healthy without history of underlying immunocompromise. Diagnoses and interventions are shown in the table. Seven had active primary chicken pox with admission occurring a median of 5 days after onset of rash. All had either secondary (5, 71%) or persisting, increasing fever (2, 29%). Six patients (including three with chicken pox) required admission to the paediatric intensive care unit (PICU). The median length of stay (LOS) in PICU was 6.5 days (range, 3- 22 days). The median LOS in hospital for all 10 patients was 21.5 days (range, 7-103 days).
Discussion
This study highlights the ongoing, significant morbidity associated with invasive GAS in children in Ireland. Chicken pox infection, long recognised as the most significant risk factor for invasive GAS in children4,5, was associated with 70% of cases from a single tertiary paediatric centre. Fever persisting beyond 5 days or recurrent secondary fever were typical in patients with invasive GAS complicating chicken pox. This characteristic clinical picture should prompt emergency referral for inpatient care. Introduction of universal varicella vaccination has dramatically reduced chicken pox related hospitalisations and deaths elsewhere, including those associated with invasive GAS infectio.6,7. That the majority of invasive GAS infections in this paediatric cluster were associated with a vaccine preventable illness should prompt reappraisal of the continuing absence of varicella vaccine from the national immunisation schedule in Ireland.
Conflicts Of Interest
There are no conflicts of interest on the paper.
Correspondence:
Cilian Ó Maoldomhnaigh, Paediatric Infectious Disease Department, Children’s University Hospital, Temple Street, Dublin 1.
Email [email protected]
References
1. HPSC. Case Definitions for Notifiable Diseases. 2012:1-112. http://www.hpsc.ie/NotifiableDiseases/CaseDefinitions/File,823,en.pdf.
2. Meehan M, Murchan S, Bergin S, Flanagan DO, Cunney R. Increased incidence of invasive group A streptococcal disease in Ireland , 2012 to 2013. Euro Surveill. 2013;2011(18(33)):pii=20556.
3. HPSC. Epidemiology of Invasive Group A Streptococcal Disease in Ireland, 2015. http://www.hpsc.ie/A-Z/Other/GroupAStreptococcalDiseaseGAS/Publications/AnnualReports/File,15967,en.pdf. Accessed March 13, 2017.
4. Coleman S. The association between varicella (chickenpox) and group A streptococcus infections in historical perspective. SAGE open Med. 2016;4:2050312116658909. doi:10.1177/2050312116658909.
5. Laupland KB, Davies HD, Low DE, Schwartz B, Green K, McGeer A. Invasive group A streptococcal disease in children and association with varicella-zoster virus infection. Ontario Group A Streptococcal Study Group. Pediatrics. 2000;105(5):E60. doi:10.1017/S0950268810001378.
6. Frère J, Bidet P, Tapiéro B, Rallou F, Minodier P, Bonacorsi S, Bingen E, Ovetchkine P. Clinical and Microbiological Characteristics of Invasive Group A Streptococcal Infections Before and After Implementation of a Universal Varicella Vaccine Program: Table 1. Clin Infect Dis. 2016;62(1):75-77. doi:10.1093/cid/civ793.
7. Patel RA, Binns HJ, Shulman ST. Reduction in pediatric hospitalizations for varicella-related invasive group A streptococcal infections in the varicella vaccine era. J Pediatr. 2004;144(1):68-74. doi:10.1016/j.jpeds.2003.10.025.\
(P718)
