Counselling in Primary Care – A General Practitioner’s Perspective
M. Rafferty1, C. Bradley2
1. Mercy University Hospital, Co. Cork
2. Department of General Practice, University College Cork, Co. Cork
Abstract
Introduction
Counselling in Primary care (CIPC) is a new service introduced by the HSE in 2013, providing short-term counselling for medical-card holders, suffering from mild to moderate mental health problems.
Aims
To explore GP’s views on CIPC for the treatment of mild to moderate mental health disorders.
Methods
Qualitative semi-structured interviews were conducted with GPs who had previously utilized the CIPC service in the Cork/ Kerry region. Forty GPs were identified and sent invitation letters. GPs were purposefully sampled based on criteria of location (urban/rural), gender, practice size (single handed/group) and length of time qualified. A total sample size was generated using the ‘ten plus three’ method. Interviews were carried out in person, transcribed verbatim and analyzed using the framework analysis method.
Results
Nineteen GPs were interviewed. Core themes emerged and were analyzed.
1. GPs unanimously agreed that CIPC has been of benefit in treating mild to moderate mental health disorders.
2. Suggested improvements to the service were made, including allowing GP visit card holders to avail of the service (n=10) and adolescents aged between 16 and 18 (n=5).
3. A majority (n=12) of GPs interviewed expressed the opinion that a combination of talk therapy and medication was associated with the best outcomes in treating mild to moderate mental health disorders.
Conclusion
CIPC seems to improve mental health services at a primary care level. While improvements can certainly be made to the service, GPs report positive patient outcomes and a reduction in psychiatric referrals for patients who can be suitably managed within the community.
Introduction
For the primary care provider, the incidence of patients presenting with mental health issues has steadily increased over the past two decades1. By 2001 in Ireland, there was a widely recognised need to develop primary care services “so that they become the cornerstone of care and preventive services for communities across the country” as this was recognised to be “...consistent with best international practice.”2. Allied to this was a growing body of international evidence for the benefits of an integrated approach to the provision of psychological and counselling services within the context of primary care3,4. As a result, the HSE initiative A Vision For Change was launched in 20061. This was a strategy document, which recommended the provision of mental health services through multidisciplinary Community Mental Health Teams (CMHTs). As part of the CMHT approach, a community based counselling service, Counselling in Primary Care (CIPC), was introduced in 2013. CIPC is now a well-established mental health service which provides up to eight free counselling sessions within the primary care setting. It is aimed at medical card holders, over the age of eighteen, with mild to moderate mental health issues. The first phase of a National Evaluation Study examining the CIPC service carried out in 2017 demonstrated some interesting findings, including the rapid growth in referrals since it’s launch with more than 19,000 referrals in 2017, an increase of 4% on the previous year 5. Certain planned evaluation tasks remained outstanding however, including qualitative data collection and analysis from key service stakeholders including GPs. This qualitative study aimed to meet this requirement by examining the benefits and limitations of this relatively new facility according to GPs in the Cork/Kerry region, with the hope of making possible recommendations for service improvement in the future.
Methods
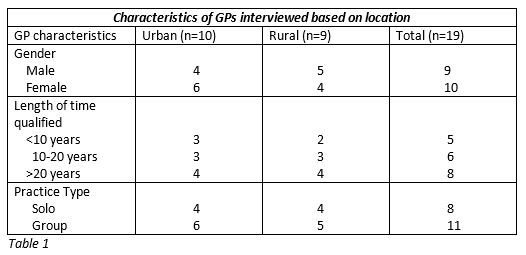
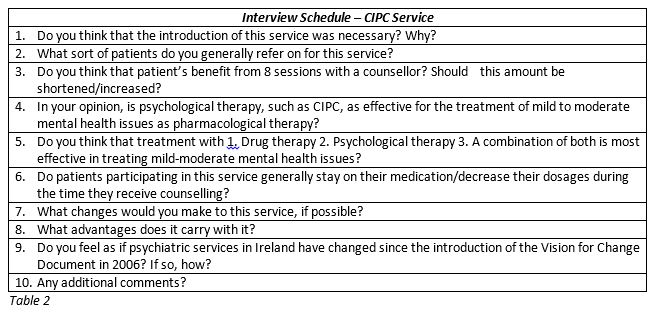
Ethical approval was granted by the Clinical Research Ethics Committee of Cork teaching hospitals in March 2016. Qualitative semi-structured interviews were conducted with GPs who had previously utilized the CIPC service in the Cork/ Kerry region. Forty GPs were identified from a list provided by the Department of General practice, UCC, and sent invitation letters. Twenty-nine GPs agreed to participate. These GPs were purposefully sampled based on criteria of location (urban/rural), gender, practice size (single handed/group) and length of time qualified (See Table 1). A total sample size was generated using the ‘ten plus three’ method6. Ten GPs were interviewed, and the information gathered was analysed at this point. Three further GPs were then interviewed to see if any new insights were being produced. Any further interviews that were considered necessary were carried out in blocks of three, with a check for a data saturation point at the end of each block (when no new information was elicited). This point was reached following two subsequent blocks of interviews, bringing the overall sample size to 19. Interviews were carried out between July 2016 and March 2017. An interview schedule which explored GPs’ views on the current service and how it might be improved was followed (see Table 2). Mean interview duration was 18 minutes. Interviews were carried out by MR, transcribed verbatim and analyzed using the framework analysis method7. Initial analysis was undertaken by MR and reviewed separately by CB. Resource constraints meant more independent validation of findings was not possible.
Results and Discussion
A table of themes was generated using framework analysis method as described by Gale et al (2013). (See Table 3).
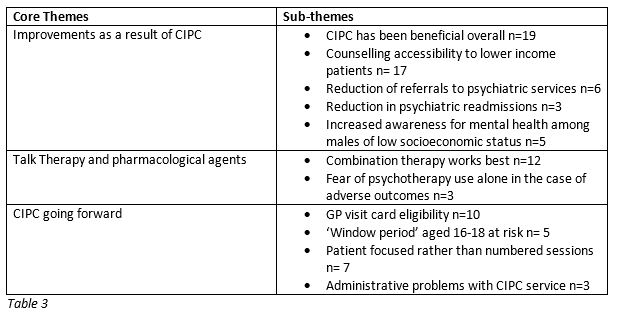
Improvements brought about by CIPC
There was a unanimous agreement among all GPs interviewed that CIPC has improved mental health services at a primary care level for a number of reasons, the most obvious being that a support now exists for patients who previously couldn’t afford counselling. This has been shown to help not only newly presenting patients, but also those who have been suffering from such mental health issues for years and may benefit from a free counselling service within the community.
Some GPs implied that CIPC, in conjunction with other new supports in the primary care setting aimed to facilitate the work of CMHTs, has prevented certain patients from relapsing on progress made as psychiatric inpatients where relevant, leading to better patient prognosis overall and a more efficient utilization of resources. This fact may be reflected in recent Health Research Board Statistics; re-admissions to psychiatric units declined by 26% between 2008 and 2017 8.
The fact that certain GPs found CIPC to have brought about a reduction in the need to refer some patients on to psychiatric services when they can be adequately managed within the community was reassuring, and relates directly back to one of the key objectives outlined by the vision for change document1, which states:
‘Well-trained, fully staffed, community-based, multidisciplinary CMHTs (Community Mental Health Teams) should be put in place for all mental health services. These teams should provide mental health services across the individual’s lifespan, and, where possible, reduce the need for in patient hospital admissions.’
Some GPs noted that CIPC has lead to an increased awareness for talk therapy among men in lower socioeconomic classes. According to census 2011 data only 48.9% of men with a mental health disability are in long term employment, compared to 78.3% of men in the overall population9. This ongoing cycle of exclusion, shame and stigmatization promotes the furthering of mental health problems amongst males, whilst increasing rates of both self- harm and suicide. Talk therapy and counselling for men who are struggling financially and who may not feel comfortable in talking to friends or family members about their problems is paramount to the resolution of this problem, and positive feedback from GPs regarding this issue is very reassuring.
GP No.13: ‘The sad fact of the matter is that the majority of those who seek out talk therapy in this country are female, and the majority of those who take their own lives are male. A service offering free, accessible counselling like CIPC may help to bridge this gap.’
Talk Therapy and pharmacological agents
The opinions of GPs in this study matched the conclusions drawn from previous research10,11,12; the majority of GPs felt that a combination of psychological and pharmacological therapy tends to work best for mild to moderate mental health disorders. Certain GPs, particularly in rural areas, felt that drug therapy should be provided first line in cases of mild to moderate depression out of fear of the repercussions that may follow should their patients deteriorate psychologically shortly after the consultation having had no prior pharmacological intervention. This is an understandable concern; previous research has shown that 68% of patients who commit suicide have been seen by a doctor in the month prior to their death13. Prescribing antidepressants for this reason alone seems somewhat counterintuitive; the most widely prescribed form of anti-depressant, SSRIs, are known to increase one’s risk of suicide in the two to three weeks following initiation of treatment, as they endow patients who had previously been contemplating suicide with a newfound alertness which may lead them to act upon their previous thoughts14. It must be appreciated that each individual case is different, however this point serves to highlight how there is an element of residual hesitancy to become reliant on talk therapy as a sole first line treatment for mild to moderate mental health problems.
CIPC going forward
Many GPs advised that the service should be made available to GP visit cardholders, in order to allow CIPC to be utilized by more patients struggling financially. As of 2014 there were approximately 402,000 GP visit card holders in the country15. The burden of having such a significant number of patients as prospective service users could very well overwhelm CIPC as it currently stands; therefore significant changes to the CIPC service would need to be made in order to facilitate this change. In turn the same benefits noted by GPs regarding medical card holders since the implementation of the service could be observed; reduced referrals to psychiatric services, increased awareness for talk therapy among males and a more efficient utilization of resources. GP’s perceptions of CAMHS services proved to be an interesting, albeit slightly unsettling, finding. The majority felt that the availability and effectiveness of mental health services for children left much to be desired; with adolescents in the ‘16-18’ age bracket most at risk of falling outside of the criteria to avail of either child or adult psychiatry services. While the Vision for Change policy document outlined many recommendations in regards to how specialist mental health services should be delivered to children who needed them, it would appear not much has been done to improve CAMHS services since the policy’s implementation almost 9 years ago. This could possibly be as a result of the economic recession that occurred shortly after the Vision for Change policy’s implementation; CAMHS staff numbers alone have decreased by 15% since 200816. Creating a similar service to CIPC with counsellors who specialize in areas pertained to adolescents and children is a starting point.
GP No.7 : ‘I’ve had one too many patients in the 16-18 age bracket…this is a vulnerable age group, prone to many mental health problems and the fact of the matter is that the services just aren’t there for them.’
The third recommendation is based around the concept that the service should be more focused around the patient in question, rather than an ‘eight session’ framework. However, recent NICE guidelines advise that no more than eight counselling sessions are required for most cases of mild to moderate mental illness 17. Opinions on this topic were varied; some GPs thought that in making CIPC a ‘limitless’ counselling service, patients wouldn’t have the motivation to reach a point of independence. The alternate view, that patients who improved over the course of their CIPC sessions could regress if their issues weren’t resolved fully, is also valid. It could be suggested that while eight sessions appears sufficient for most patients, cases where patient’s issues hadn’t been resolved could benefit from further counselling at the recommendation of the counsellor or a referral to a psychiatric team. Issues pertaining to confusion regarding eligibility criteria and the referral process were discussed. This pertained to a minority of GPs, however many suggested that the referral process should be made available to be carried out online; saving time and resources both for GPs and administrative staff.
Conclusion
Overall, the concluding data from this study shows that Counselling in Primary Care is an effective service for the treatment for mild to moderate mental health issues at a primary care level, with all GPs unanimously agreeing that it has positively influenced how such issues are managed within the community. This study supports existing literature which demonstrates that a combination of talk therapy and pharmacological agents tend to work best for the treatment of mild mental health disorders. Future research, using a nationwide approach in sampling GPs to further add to the results found in this article is recommended, as is externally auditing framework analysis results. These limitations, as experienced in this study, may be addressed in the second phase of the National Evaluation Study for CIPC, due in 2019.
Conflict of Interest
The author has no conflicts of interest to declare.
Corresponding Author
Dr. Mairead Rafferty,
Mercy University Hospital,
Co. Cork
Email: [email protected]
References
1. Health Service Executive; A Vision For Change. 2006 p. 8-10.
2. Department of Health & Children Business Plan, 2006, p. 17)
3. Bor R, McCann D, editors. The Practice of Counselling in primary care. Sage; 1999 May 19.
4. Evans R, Mellor-Clark J, Barkham M, Mothersole G. Developing the resources and management support for routine evaluation in counselling and psychological therapy service provision: Reflections on a decade of CORE development. European Journal of Psychotherapy and Counselling. 2006 Jun 1;8(2):141-61.
5. HSE NCS (2018). Counselling in Primary Care Service, National Evaluation Study, Phase 1. Dublin: Health Service Executive, pp.3-12.
6. Ritchie J, Lewis J: Qualitative research practice: a guide for social science students and researchers. 2003, London: Sage
7. Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC medical research methodology. 2013 Dec;13(1):117.
8. Daly, A. &; Walsh, D. Activities of Irish Psychiatric Units and Hospitals 2016, Dublin: Health Research Board, p. 15. (2017)
9. CSO (2011) Profile 3 at work – Employment, Occupations and Industry: Irish Census, CSO Publishing, Cork, CD358.
10. McHugh RK, Whitton SW, Peckham AD, Welge JA, Otto MW. Patient preference for psychological vs. pharmacological treatment of psychiatric disorders: a meta-analytic review. The Journal of clinical psychiatry. 2013 Jun;74(6):595.
11. Heuzenroeder L, Donnelly M, Haby MM, Mihalopoulos C, Rossell R, Carter R, Andrews G, Vos T. Cost-effectiveness of psychological and pharmacological interventions for generalized anxiety disorder and panic disorder. Australian and New Zealand journal of psychiatry. 2004 Jan 1;38(8):602-12.
12. Wolf NJ, Hopko DR. Psychosocial and pharmacological interventions for depressed adults in primary care: a critical review. Clinical psychology review. 2008 Jan 1;28(1):131-61.
13. World Health Organization, Figures and Facts about Suicide. Geneva: World Health Organization. (1999)
14. Predictable SE. Side effects of antidepressants: an overview. Cleve Clin. J. Med.. 2006 Apr;73:351-61.
15. Department of Public Expenditure and Reform. Staff Paper; General Medical Services Scheme. July 2016.
16. HSE. Fifth Annual Child & Adolescent Mental Health Service Report 2012 – 2013, p.58. (2014)
17. NICE Clinical Guidelines. Depression in adults: recognition and management;(October 2009)
P869
