Knowledge, Attitudes and Practices of Non-Consultant Hospital Doctors In The Immediate Post-Fall Period
O’Reilly, D.1, Rutledge, N.1, Hurson, C.2, Clifford, G.2
1 UCD Intern Training Network
2 St. Vincent’s University Hospital
Abstract
Aim
The aim of this study is to determine the knowledge, attitudes and practices of Non-Consultant Hospital Doctors (NCHDs) in the immediate post-fall period.
Methods
A survey study design was employed using an online questionnaire of all NCHDs in SVUH comprising 15 questions that blend dichotomous, multiple choice, scaled and open-ended questions to determine knowledge, attitudes and practices of NCHDs across three constructs; injury management, falls prevention and fracture prevention. Descriptive statistics was used to analyse data.
Results
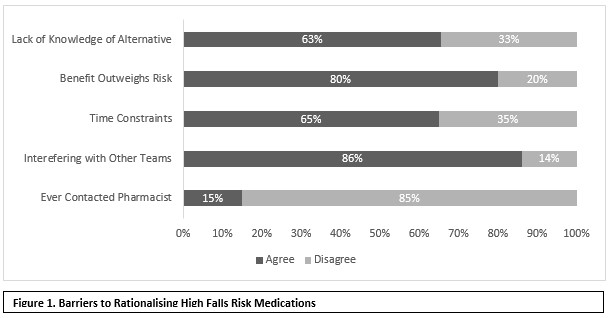
There was a 40% response rate (n=105). The respondents reported dissatisfaction with their standard of falls assessment training (mean 4/10). Between 60-70% of NCHDs do not routinely determine hip trauma, joint tenderness, syncope, use of anti-coagulants, visual symptoms, amnesia or vomiting. Half of respondents (n=57) rarely or never rationalised medications. The main reasons for this are lack of knowledge of alternatives (63%), time constraints (65%), benefits outweighing the risks (80%) and reluctance to interfere with care of another medical team (86%). Only 9% always consider a bone health review.
Discussion
A targeted education programme in the areas of hip assessment, neurological assessment, syncope management, medication rationalisation and bone protection is warranted.
Introduction
Falls are the most common adverse incident in hospital that medical teams are requested to assess. Approximately 240,000 falls occur annually in acute hospitals in England and Wales1. Nearly 40% of people who suffer an in-hospital hip fracture are dead within three months2. Despite the frequency of falls, the quality of medical assessment post-fall can vary significantly. Post-fall medical assessment tends to focus on injury identification and misses many opportunities for prevention. St. Vincent’s University Hospital (SVUH) have developed a standardised in-hospital post-fall medical review proforma for use by non-consultant hospital doctors (NCHDs). The proforma comprises a concise history and physical examination, identification and management of common falls-related injuries; and prompts to identify and rationalise high falls risk medications (HFRM). The proforma incorporates relevant best practice recommendations and clinical guidelines3. Understanding the NHCD approach to falls prevention is an important step in the development of this proforma, and to guide future education programmes and quality improvement initiatives aimed at modifying behaviours of NCHDs. The aim of this study is to determine knowledge, attitudes and practices (KAP) of NCHDs in the immediate post-fall period.
Methods
A survey study design was employed using an online questionnaire which comprised 15 questions that blended dichotomous, multiple choice, scaled and open-ended questions to determine knowledge, attitudes and practices of NCHDs across three constructs; injury management, falls prevention and fracture prevention. A pilot questionnaire was performed with 20 NCHDs after which modifications were made to the instrument and process. There were 269 NHCDs working clinically in SVUH at the time of the survey. Assuming a response rate of 50%, a sample of 134 was required. Medical HR sent a pre-prepared email to all NCHDs with an overview of the study, including participant information, and a link to the questionnaire. A follow up email was sent to NCHDs two weeks later by Medical HR to improve the response rate. Completion of the online questionnaire was deemed as consent. Ethical approval was received from SVUH Ethics Committee. Descriptive statistics were used to analyse data.
Results
There was a 40% response rate (n=105; Intern: 81%; SHO: 9%; Reg/SpR 10%). SHOs and Reg/SpR do not typically perform a post-fall assessment which may account for the low response rate. The respondents reported being confident in their assessment of a fall (mean 8/10) but were not satisfied with the standard of falls assessment training (mean 4/10). Most NCHDs (>90%) routinely determined the mechanism of fall, blackout, pain, vitals and head trauma. Between 60-70% of NCHDs do not routinely determine hip trauma, joint tenderness, use of anti-coagulants, syncope, visual symptoms, amnesia or vomiting. Importantly, the medication record is reviewed (65%) and high falls risk medications are identified (65%) frequently. However, 57% rarely or never rationalise medications. The main reasons for this are lack of knowledge of alternative (63%), time constraints (65%), benefits outweighing the risks (80%) and reluctance to interfere with care of another medical team (86%). Only 9% always consider a bone health review.
Discussion
The Post-Fall Medical Review Proforma has been implemented hospital-wide and, through local audit, has shown consistently high usage among NCHDs. Despite their reported confidence, which may arise from an element of complacency due to the non-injurious nature of most inpatient falls, it is clear that NCHDs require more comprehensive training in the assessment of a patient in the immediate post-fall period particularly in hip assessment; neurological assessment; syncope management; medication rationalisation; and bone health. NCHDs do not always complete an appropriate musculoskeletal or neurological assessment. NCHDs report that the benefits of HFRM can outweigh the risks though this does not correlate with 63% reporting that they lack knowledge of alternative medications. The low level of bone health assessments may reflect a perceived non-acute nature of osteoporosis. A targeted education programme around these key areas is warranted. Suggestions include a multidisciplinary lunchtime teaching session with the following topics: Hip Assessment (physiotherapist/orthopaedic surgeon); neurological assessment (neurologist); medication rationalisation (pharmacist); syncope management (geriatrician); and bone protection (endocrinologist).
Conflicts of Interest
The authors have no conflicts of interest.
Correspondence
Gareth Clifford, Dr. Steeven’s Hospital, Dublin 8
Tel: 076-6959944
Email: [email protected]
References
1. Royal College of Physicians. National Audit of Inpatient Falls: audit report 2015. London: RCP, 2015
2. Johal, K.S., Boulton, C. and Moran, C.G. (2009) Hip fractures after falls in hospital: a retrospective observational study Injury 40: 201-204
3. National Patient Safety Agency. Essential care after an inpatient falls 2011 – NPSA/2011/RRR01. London: NPSA, 2011
(P740)
