The Triangular Sign, a Useful Diagnostic Marker for Biliary Atresia: A Case Series of Three Irish Infants
Smith A1, Shankar A2, Collins A3, Tarrant A4, 5, & Boyle MA1, 2
1Department of Neonatology, The Rotunda Hospital, Dublin
2The Royal College of Surgeons, Dublin
3National Centre for Paediatric Gastroenterology, Our Lady’s Children’s Hospital, Crumlin, Dublin
4Department of Radiology, The Rotunda Hospital, Dublin
5Department of Radiology, Temple Street Children’s University Hospital, Dublin
Abstract
Background
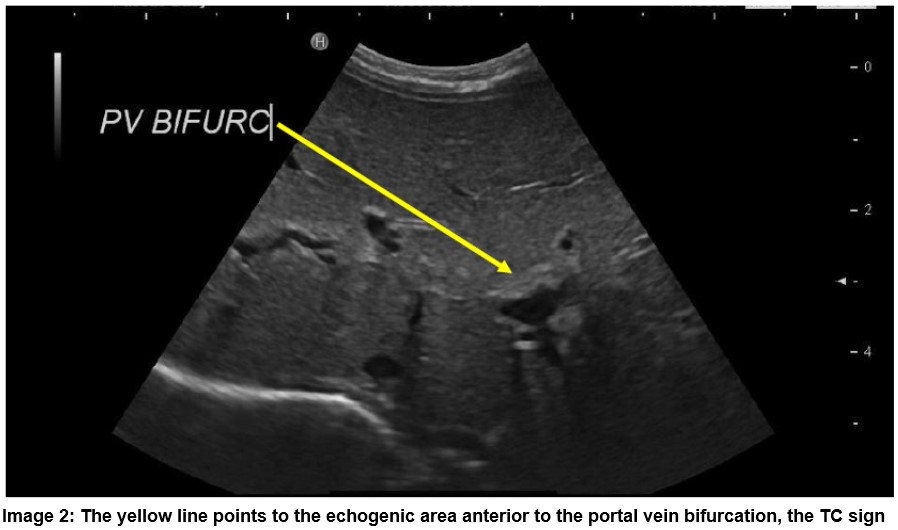
The triangular cord (TC) sign is the appearance of a triangular shaped echogenic density visualised immediately cranial to the portal vein bifurcation on ultrasonographic examination. Several studies have reported that this ultrasonographic sign is a reliable and helpful marker in identifying Biliary Atresia (BA).
Aims
To report the identification of the TC sign in three infants with BA in the Rotunda Hospital, Dublin.
Methods
A retrospective chart review was performed to evaluate the clinical presentation and imaging of the three patients with positive TC sign and BA.
Discussion
Timely, accurate diagnosis of BA is essential to minimise morbidity and optimise patient outcome. The TC is a valuable ultrasonographic sign to aid early diagnosis of BA.
Introduction
Biliary atresia (BA) is an idiopathic, chronic cholangiopathy leading to progressive obliteration of the intra and extrahepatic biliary tracts. The incidence of BA in the UK and Ireland is estimated at 1/16,700 live births, equating to approximately 4 babies born with BA in Ireland annually5. Classic symptoms include jaundice, pale stools and dark urine. Additional features such as hepatomegaly and failure to thrive may also be evident. Initial investigations include direct and indirect bilirubin, liver function tests, albumin, exclusion of congenital infection, coagulation screen and Coombs test. BA must be ruled out in any infant presenting with a conjugated jaundice.
Ultrasound scanning is indicated in each case of suspected BA to assess liver, gallbladder and spleen morphology, the presence of a common bile duct, vascular anatomy and presence of triangular cord sign. The triangular cord (TC) sign is the appearance of a triangular shaped echogenic density visualised immediately cranial to the portal vein bifurcation on ultrasonographic examination1. The TC represents the fibrotic remnant of the extra hepatic bile duct in BA6. Several studies have reported that the identification of this ultrasonographic sign is a reliable and helpful marker in reaching the diagnosis of BA2,3. Hepatobiliary iminodiacetic acid (HIDA) scanning is useful in supporting the diagnosis of BA, however many babies will go straight to biopsy to confirm BA due to time pressure to perform the Kasai procedure. As noncholestatic jaundice is extremely common in early infancy it can prove quite difficult to accurately identify the rare infant with cholestatic jaundice and BA. Therefore any sign which facilitates early detection of BA warrants attention. Here we report the identification of the TC sign in three patients born in the Rotunda Hospital, Dublin with subsequently confirmed BA.
Case Series
All three infants in our case series were term, female babies. Clinical jaundice was evident for all three patients and pale stools and dark urine were noted for patients two and three. Patients one, two and three had direct hyperbilirubinaemia detected of 137 μmol/L at 6 weeks of age, 103 μmol/L at four weeks of age and 150 μmol/L at 29 hours of age respectively. All three babies also had deranged liver function tests. There was no case of congenital infection or Coombs positive jaundice. Ultrasound imaging was requested and the TC sign was demonstrated for all three patients, as per Images one and two. The diagnosis of BA for patients one and two was primarily based on the lack of visualization of the gallbladder on a fasting ultrasound scan, in combination with the presence of the TC sign. For patient three, an ultrasound following a four-hour fast demonstrated a small gallbladder measuring 2.2mm in length in combination with the TC sign. Such ultrasound findings supported a suspected diagnosis of BA for all three patients and prompt referral to The National Centre for Paediatric Gastroenterology, Our Lady’s Children’s Hospital, Crumlin was arranged.
A hepatobiliary iminodiacetic acid scan (HIDA) was performed in Patient 3 prior to biopsy confirmation of the diagnosis of BA. Patient 1 and 2 proceeded directly to biopsy to confirm BA diagnosis. Once BA was confirmed all three babies were transferred to the UK for Kasai procedure within days as early corrective surgery before 8 weeks of age has a superior outcome.

Discussion
Early diagnosis of BA is essential. This condition is fatal unless surgical correction is performed and BA is the leading indication for liver transplantation in children7. Earlier age of BA detection is a predictor of improved native liver survival8. A UK & Ireland study also reported that if portoenterostomy is successful few children with BA require liver transplantation prior to adolescence9. A 2017 meta-analysis of 17 eligible studies with 1,444 patients reported that the triangular cord sign had a high accuracy for diagnosing BA with a sensitivity and specificity of 85 % (95% confidence interval, 77%-90%) and 97% (95% confidence interval, 94%-99%) respectively10. In addition, Kanegawa et al reported that the TC sign was more a more useful ultrasonographic sign than gallbladder contraction or length2.
In conclusion, timely, accurate diagnosis of BA is essential to minimise morbidity and optimise patient outcome. The TC is a valuable ultrasonographic sign to aid early identification of this uncommon condition as demonstrated in this report of three Irish patients with BA.
Corresponding Author:
Aisling Smith, The Rotunda Hospital, Parnell Square, Dublin
Email:[email protected]
Conflict of Interest
The authors have no conflict of interest to declare
References
1. Imanieh MH, Dehghani SM, Bagheri MH, Emad V, Haghighat M, Zahmatkeshan M, Forutan HR, Rasekhi AR, Gheisari F. Triangular cord sign in detection of biliary atresia: is it a valuable sign? Digestive diseases and sciences. 2010;55(1):172-5.
2. Kanegawa K, Akasaka Y, Kitamura E, Nishiyama S, Muraji T, Nishijima E, Satoh S, Tsugawa C. Sonographic diagnosis of biliary atresia in pediatric patients using the "triangular cord" sign versus gallbladder length and contraction. AJR American journal of roentgenology. 2003;181(5):1387-90.
3. Kotb MA, Kotb A, Sheba MF, El Koofy NM, El-Karaksy HM, Abdel-Kahlik MK, Abdalla A, El-Regal ME, Warda R, Mostafa H, Karjoo M, HH AK. Evaluation of the triangular cord sign in the diagnosis of biliary atresia. Pediatrics. 2001;108(2):416-20.
4. Humphrey TM, Stringer MD. Biliary atresia: US diagnosis. Radiology. 2007;244(3):845-51.
5. McKiernan PJ, Baker AJ, Kelly DA. The frequency and outcome of biliary atresia in the UK and Ireland. Lancet (London, England). 2000;355(9197):25-9.
6. Tan Kendrick AP, Phua KB, Ooi BC, Subramaniam R, Tan CE, Goh AS. Making the diagnosis of biliary atresia using the triangular cord sign and gallbladder length. Pediatric radiology. 2000;30(2):69-73.
7. Wang KS. Newborn Screening for Biliary Atresia. Pediatrics. 2015;136(6):e1663-9.
8. Jimenez-Rivera C, Jolin-Dahel KS, Fortinsky KJ, Gozdyra P, Benchimol EI. International incidence and outcomes of biliary atresia. Journal of pediatric gastroenterology and nutrition. 2013;56(4):344-54.
9. McKiernan PJ, Baker AJ, Lloyd C, Mieli-Vergani G, Kelly DA. British paediatric surveillance unit study of biliary atresia: outcome at 13 years. Journal of pediatric gastroenterology and nutrition. 2009;48(1):78-81.
10. Yoon HM, Suh CH, Kim JR, Lee JS, Jung AY, Cho YA. Diagnostic Performance of Sonographic Features in Patients With Biliary Atresia: A Systematic Review and Meta-analysis. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2017.
(P776)
