Ultrasound as a Diagnostic Tool in Pediatric Distal Forearm Fractures
A.S. Ahmed, A.E. Abdelhady, B. McNicholl
University College Hospital Galway, Ireland
Abstract
Aims
To evaluate the accuracy of ultrasound in pediatric distal forearm fractures as well as the effect on the ED waiting time for these patients.
Methods
Convenience sample of 42 pediatric patients presented with wrist injury. All patients underwent US examination followed by 2-views radiographs of the wrist with recording the time to US. In addition, the time to X-ray were calculated, retrospectively, on 95 pediatric patients for comparison.
Results
Forty-two patients were examined, 25 males (60%) and 17 females (40%), mean age 7.2 years. On X-Ray, 30 patients (71%) were confirmed to have a distal forearm fractures, of which, 28 (93%) were diagnosed by US. The sensitivity of ultrasound diagnosis was 93.3% (95% CI, 83%-100%), and the specificity was 92% (95% CI, 76%-100%). The positive and negative likelihood ratios were 11.6 and 0.07, respectively.
Conclusions
Ultrasound is a reliable diagnostic tool in the diagnosis of distal forearm fractures in children. Ultrasound has radiation free and decreases the length of stay in ED.
Introduction
Distal forearm fractures are considered one of the commonest injuries in adults and children, due to falling on an outstretched hand1. In children, the bone is softer and more flexible, and the fractures are mostly extra-articular2,3. There are different types of fractures distinctively seen in children: torus fractures (buckle), greenstick fractures, complete fractures and fractures of the epiphyseal plate4.
The main objectives of management are; to restore alignment and clinical appearance, to limit injury to local soft tissues and to regain functional forearm rotation5.
X-Ray studies are the most common investigation for suspected fractures6. Ultrasound (US) has recently been used for the detection of fractures, with reports suggesting that it may be more sensitive than X-Ray studies, because bone acts as a natural obstacle against sound transmission at high frequencies. Furthermore, US has the capability to analyze a region in multiple planes rather than the limited views offered by traditional radiography7,8. Currently, experience in bedside ultrasound is growing amongst emergency physicians9,10, with a relatively easy learning curve11,12. The absence of exposure to ionizing radiation is one of the main advantages of US. Children are up to four times more radiation sensitive than adults13-15. Another advantage in pediatric patients is the reduced pain exposure16,17. The role of ultrasound as a gold standard screening tool is currently under discussion18,19. An important feature in this debate is the actual diagnostic accuracy of ultrasound for detecting forearm fractures and is it possible that the US could replace the X-Ray in the emergency department.
The aim of our study is to evaluate and confirm the accuracy of ultrasound as a diagnostic tool in pediatric distal forearm fractures as well as the impact on ED waiting time.
Methods
This is a single center prospective diagnostic study utilizing a convenience sample of children from January to June 2017. Patients between the ages of one and 17 years who presented to the ED, University Hospital Galway, Ireland, with non-angulated distal forearm injuries were invited to participate after verbal consent from their guardian. Children were excluded if there was a clinical forearm deformity, multisystem trauma, history of bone disease or neurovascular compromise. Patients who arrived when no US trained doctor was present were treated in the normal fashion with X-Ray. All participants were assessed according to the eligibility criteria before performing an US with six views of the forearm. The presence of a cortical gap, cortical bulging, a kink, a torus formation, or a displacement was considered as diagnostic criteria for a fracture on ultrasound. Both the ED doctor who performed the US and the radiographer were blinded. The secondary outcome was to compare the waiting time to either US or X-Ray. This was assessed by measuring the time to the US prospectively and comparing it to the waiting time to X-Ray of a retrospective cohort of 95 patients.
All participants were examined with US by four emergency doctors who had attended the one-hour US presentation and hands-on training session. Time to US and the result of the scan were recorded. After US examination, a standard 2 views X-Ray of the wrist were taken. Finally, the patient was treated based on the X-Ray results and according to our institutional policy. All Data were collected and tabulated in a 2X2 contingency table. The study was reviewed and approved by Chairman Clinical Research Ethics Committee (CCREC) in Galway University Hospital.


Results
Forty-two patients were examined, 25 males (60%) and 17 females (40%), mean age 7.2 years. On X-Ray, 30 patients (71%), were confirmed to have a distal forearm fracture, including 29 radial fractures (69%), and one isolated ulnar fracture. Twenty-eight (93%) of the 30 fractures were diagnosed by US. In a further case, a fracture could not be ruled out by X-Ray, where the patient had positive findings on ultrasound. This was followed up by an orthopedic consultant in a fracture clinic, wherein he confirmed a fracture was present and treated the patient as such. On the basis of this review, the sensitivity of ultrasound diagnosis was 93.3% (95% CI, 83%-100%), and the specificity was 92% (95% CI, 76%-100%). The positive and negative predictive values were 0.97 and 0.85 respectively. The positive likelihood ratio was 11.6, which renders the US as a strong rule-in test (above 10). The negative likelihood ratio was 0.07 which is very close to zero, making the US a strong rule-out test. Based on this data, the accuracy of US in the diagnosis of distal forearm fractures was 93%.
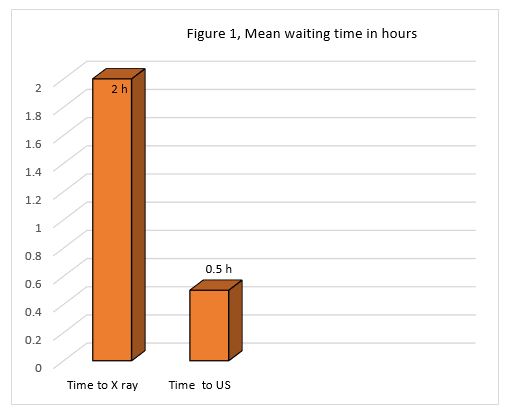
The mean waiting time to the US in the prospective study, including 42 children, was 30 minutes. This is in comparison to two hours of waiting time to X-Ray in the retrospective study, Figure 1.
Discussion
Based on the anatomy of the forearm, US is appropriate for the diagnosis of the fractures. The good image quality is guaranteed by both minimal soft tissue and the limited distance between the probe and the bone. This explains the high sensitivity and specificity (93% and 92% respectively), of ultrasound in the diagnosis of distal forearm fractures in children. The two missed patients were diagnostically insignificant, and the management plan was the same based on US versus X-Ray.
Time is always a constraint. If a patient can be seen and given a diagnosis without having to wait for two hours to get an X-Ray, this can help minimize the waiting time burden in Emergency Departments. This is especially true if we have a reliable alternative diagnostic tool with a waiting time of 30 minutes. Moreover, using the US as the sole initial diagnostic imaging modality, can reduce the exposure of pediatric patients to unnecessary doses of ionizing radiation.
In the literature, Rachel et al20, Herren et al21, Patel et al22 and Naveen et al23 were showed a high sensitivity and specificity, above 90%, in diagnosis of distal forearm fractures after short period of training, which is in line with our results. In our study we used one-hour US training, which is not a standard, to prove that US is growing amongst emergency physicians with a relatively easy learning curve. Although we are not calculating the power, however there are some studies such as Patel et al22 who did the power, 87%, and his sample size was 33 child which is less than ours. Regarding to the sample types, most of the studies used a convenience sample in a similar fashion to ours apart of Patel et al22 and Herren et al21 which used a consecutive sample. Rachel et al20, Naveen et al23, and Frances et al24 used pain and parent satisfaction as a secondary outcome. Unfortunately, we did not use this, however, we used the waiting time as Naveen et al23. Regarding the waiting time, we did use the mean rather than the median because our data did not include outliers.
Ultrasound is a reliable diagnostic tool, in the diagnosis of distal forearm fractures in children when performed by well-trained emergency doctors and using an appropriate viewing method. Ultrasound has an advantage over X-Ray, in terms of being radiation free and decreasing the length of stay in ED.
Conflict of Interest
No conflict of Interest
Corresponding Author
Ayman S. Ahmed
University College Hospital Galway
Email: [email protected]
References
1. Naranje SM, Erali RA, Warner WC Jr, Sawyer JR, Kelly DM. Epidemiology of Pediatric Fractures Presenting to Emergency Departments in the United States. J Pediatr Orthop. 2015 Jul 14.
2. Mizuta T, Benson WM, Foster BK, Paterson DC, Morris LL. Statistical analysis of the incidence of physeal injuries. J Pediatr Orthop 1987 Sep-Oct; 7(5):518–523. PMID: 349794.
3. Ackermann O, Liedgens P, Eckert K, Chelangattucherry E, Ruelander C, Emmanouilidis I, et al. Ultrasound diagnosis of juvenile forearm fractures. J Med Ultrason 2010; 37(3):123–127.
4. Laer LK, Linhart R. Frakturen und Luxationen im Wachstumsalter. 5th ed.Stuttgart, New York: Thieme; 2007.
5. Rodríguez-Merchán EC. Pediatric fractures of the forearm. Clin Orthop Relat Res. 2005 Mar; (432):65-72. Review.
6. Metz VM, Gilula LA. Imaging techniques for distal radius fractures and related injuries. Orthop Clin North Am 1993; 24:217–28.
7. Lewis D, Logan P. Sonographic diagnosis of toddler’s fracture in the emergency department. J Clin Ultrasound 2006; 34:190–4.
8. Beltrame V, Stramare R, Rebellato N, Angelini F, Frigo AC,Rubaltelli L. Sonographic evaluation of bone fractures: a reliable alternative in clinical practice? Clin Imaging 2012; 36:203–8.
9. May G, Grayson A. Towards evidence-based emergency medicine: best BETs from the Manchester Royal Infirmary. Bet 4: the use of ultrasound in the diagnosis of paediatric wrist fractures. Emerg Med J 2009; 26:822–5.
10. Dietrich AM, Coley BD. Bedside pediatric emergency evaluation through ultrasonography. Pediatr Radiol 2008; 38(suppl 4): S679–84.
11. Heiner JD, Proffitt AM, McArthur TJ. The ability of emergency nurses to detect simulated long bone fractures with portable ultrasound. Int Emerg Nurs 2011 Jul; 19(3):120–124. doi: 10.1016/j.ienj.2010. 08.004 PMID: 21665155.
12. Noble VE, Legome E, Marshburn T. Long bone ultrasound: making the diagnosis in remote locations. J Trauma 2003 Apr; 54(4):800. PMID: 12707550.
13. Ait-Ali L, Andreassi MG, Foffa I, Spadoni I, Vano E, Picano E. Cumulative patient effective dose and acute radiation-induced chromosomal DNA damage in children with congenital heart disease. Heart 2010 Feb; 96(4):269–274. doi: 10.1136/hrt.2008.160309 PMID: 19687017.
14. Linet MS, Slovis TL, Miller DL, Kleinerman R, Lee C, Rajaraman P, et al. Cancer risks associated with external radiation from diagnostic imaging procedures. CA Cancer J Clin 2012 Mar-Apr; 62(2):75–100. doi: 10.3322/caac.21132 PMID: 22307864.
15. Brenner DJ, Doll R, Goodhead DT, Hall EJ, Land CE, Little JB, et al. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci U S A 2003 Nov 25; 100 (24):13761–13766. PMID: 14610281.
16. Chaar-Alvarez FM, Warkentine F, Cross K, Herr S, Paul RI. Bedside ultrasound diagnosis of nonangulated distal forearm fractures in the pediatric emergency department. Pediatr Emerg Care 2011; 27 (11):1027–1032. doi: 10.1097/PEC.0b013e318235e228 PMID: 22068062.
17. Ackermann O, Eckert K, Schulze PC. Ultrasound diagnosis of forearm fractures in the growing age. No more x-ray. Ultraschall Med Suppl 2013; 34.
18. Sinha TP, Bhoi S, Kumar S, Ramchandani R, Goswami A, Kurrey L, et al. Diagnostic accuracy of bedside emergency ultrasound screening for fractures in pediatric trauma patients. J Emerg Trauma Shock 2011 Oct; 4(4):443–445. doi: 10.4103/0974-2700.86625 PMID: 22090734.
19. Rathfelder FJ, Paar O. Possibilities for using sonography as a diagnostic procedure in fractures during the growth period. Unfallchirurg 1995 Dec; 98(12):645–649. PMID: 8584947.
20. Rachel Rowlands, MBCHB, MRCPCH, James Rippey, MBBS, FACEM, Sing Tie, MBBS, FRACP, and James Flynn, MBBS, FACEM. Bedside ultrasound vs x-ray for the diagnosis of forearm fractures in children. Emergency medicine journal, October 2016.
21. Herren C, Sobottke R, Ringe M, Visel D, Graf M, Müller D, et al. Ultrasound-guided diagnosis of fractures of the distal forearm in children. Orthopaedics & Traumatology: Surgery & Research. 2015; 101(4):501–5.
22. Patel DD, Blumberg SM, Crain EF. The Utility of Bedside Ultrasonography in Identifying Fractures and Guiding Fracture Reduction in Children. Pediatric Emergency Care. 2009; 25(4):221–5.
23. Naveen Poonai, MD, Frank Myslik, MD, Gary Joubert, MD, Josiah Fan, MD, Amita Misir, MD, Victor Istasy, MB, BCh, Melanie Columbus, PhD, Robert Soegtrop, BSc Alex Goldfarb, BSc, Drew Thompson, MD, and Alexander Sasha Dubrovsky, MDCM, MS: Point-of-care Ultrasound for Nonangulated Distal Forearm Fractures in Children:Test Performance Characteristics and Patient-centered Outcome, ACADEMIC EMERGENCY MEDICINE, May 2017, Vol. 24, No. 5.
24. Frances M. Chaar-Alvarez, MD, MSc, Fred Warkentine, MD, MSc, Keith Cross, MD, MSc, Sandra Herr, MD, and Ronald I. Paul, MD. Bedside Ultrasound Diagnosis of Nonangulated Distal Forearm Fractures in the Pediatric Emergency Department. Pediatr Emer Care 2011; 27: 1027-1032.
P836
