A Study To Assess The Prevalence Of Exercise-Induced Bronchoconstriction In Inter-County Hurling.
Hunt EB1,2, Murphy B3, Murphy C4, Crowley T5, Cronin O1, Hay S1, Stack M1, Bowen B1, Ronan NJ1, Greene E1, Eustace JA2, Plant BJ1,2, Murphy DM1,2
1Department of Respiratory Medicine, Cork University Hospital
2Health Research Board Clinical Research Facility, University College Cork, Cork
3Tipperary Hurling CLC, Thurles,
4Cork Hurling CLC, Cork
5Kilkenny Hurling CLC, Kilkenny
Abstract
Exercise-Induced Bronchoconstriction (EIB) is an acute, transient airway narrowing occurring after exercise which may impact athletic performance. Studies report 10% of the general population and up to 90% of asthmatics experience EIB. Ninety-two players from three elite hurling squads underwent a spirometric field-based provocation test with real-time heart rate monitoring and lactate measurements to ensure adequate exertion. Players with a new diagnosis of EIB and those with a negative field-test but with a previous label of EIB or asthma underwent further reversibility testing and if negative, methacholine challenge. Eight (8.7%) of players had EIB, with one further athlete having asthma with a negative field test. Interestingly, only three out of 12 players who had previously been physician-labelled with EIB or asthma had their diagnosis objectively confirmed. Our study highlights the role of objective testing in EIB.
Introduction
Exercise Induced Bronchoconstriction (EIB) is an acute, transient airway narrowing defined as a 10% or more decline in FEV1 that occurs after exercise1. Usual symptoms include wheezing, shortness of breath, cough, or chest tightness during or after exercise. Symptoms usually occur during strenuous exercise and typically peak 5-10 minutes after exercise. Despite this, self-reported symptoms are poor predictors of EIB because several other conditions can mimic symptoms2. Conversely, athletes with no respiratory symptoms can have a bronchoconstrictive response to exercise3. Therefore, symptoms taken in isolation are unreliable when attempting to diagnose EIB. Exercise-Induced Bronchoconstriction is more common in endurance sports and sports that require high minute ventilation. More than 10% of the general population and up to 90% of persons previously diagnosed with asthma experience EIB4. The reported prevalence of EIB in athletes varies widely between sports and ranges from 7 to 50%, although it approaches 90% in athletes with asthma4,5.
The underlying mechanisms involved in this bronchoconstrictive response to exercise have not been fully elucidated with both airway cooling resulting from conditioning of inspired air and post-exercise rewarming of airways6. The airway response in EIB is believed to be initiated by airway dehydration with subsequent subtle changes in osmolarity resulting in changes in airway cells and ensuing inflammation7.
Hurling is the national sport of Ireland. It is played by two opposing teams of 15 players (squads of 30 players) on a grass surface and is considered to be one of the fastest team field sports (with the ball travelling up to 180km/hour), requiring a combination of anaerobic and aerobic stamina. Its combination of short bursts of speed are equivalent to those seen in ice-hockey but the size of the field (135–145 meters long and 80–90 meters wide) make the overall aerobic requirements similar to that of soccer. The sport is played all year round but with the main competitions played over the summer months. Despite being a national sport there is a paucity of research pertaining to exercise or medical related issues, with the majority of published research examining the epidemiology of sporting related injuries8,9,10. In order to more accurately reflect the typical exercise required for hurling we performed a field test in the team’s own training environment. We modified the field test to incorporate facets of a laboratory-based test to ensure that the exercise performed would be vigorous enough to potentially provoke a bronchoconstrictive response in a susceptible athlete. Using our field test we then aimed to define the prevalence of EIB in hurling, focusing our study on a cohort of elite inter-county hurlers-this cohort (three squads; Kilkenny, Cork and Tipperary) included the All-Ireland Finalist from 2013, both finalists from 2014 as well as the subsequent All-Ireland Winners from 2015.
Methods.
Ninety-two players from three senior inter-county hurling teams (Cork, Kilkenny and Tipperary) were recruited for the study in the period February-April 2015, during preseason training but prior to the commencement of the Senior Hurling Championship. This study was carried out in GAA Grounds as chosen by individual team coaches. This study was conducted with the approval of the Clinical Research Ethics Committee of the Cork Teaching Hospitals. All players underwent initial assessment comprising: a validated asthma control questionnaire if previously diagnosed with asthma11; spirometry testing pre and post a standardised field-based provocation test; blood testing for total IgE level and RAST (radioallergosorbent test) testing (grass, house dust mite, cat and dog) and post-exercise capillary sampling for lactate. The exercise protocol utilized in this study involved each player performing two minutes of high intensity hurling manoeuvres incorporating the basic skills of the game.
These manoeuvres were immediately followed by at least four minutes high intensity running-extended as needed to maintain a heart rate ≥80% predicted for four minutes. After this serial spirometry was performed to assess for a drop in FEV1 in accordance with standard exercise provocation protocols1,12. Pre-exercise and post-exercise spirometric data were measured using a calibrated, computerized, neumotachograph spirometer (Microlab Mark 8 Spirometer, Micro Direct, Inc. Lewiston, ME).
During the test, live heart rate monitoring was performed using the Polar H7 Heart rate sensor (Polar Electro, Kempele, Finland) in conjunction with Polar Team Sport application on the Apple® iPad (San Cupertino, California, USA). Using this device we were able to test 10 athletes simultaneously. Immediately after exercise a capillary blood lactate measurement was performed using the Simplified Blood Lactate Test Meter Lactate Pro2 LT-1730 (Arkray Inc. Kyoto, Japan). A qualified physician was present for all exercise testing. The ability to monitor heart rate in real-time is a unique facet of our field test, being more typical for a laboratory based test. This, in addition to on-site measurement of lactate insured an adequate test.
All eligible players consented to inclusion (any active member of the hurling squads). Those players with a prior diagnosis of either asthma or EIB were asked to withhold their medication in line with standard testing protocol4. No exclusion criteria were applied. Players previously labeled with asthma and/or EIB, who had a negative field provocation test, subsequently underwent laboratory-based pulmonary function tests with a bronchodilator challenge and/or methacholine challenge in order to either formalize or out-rule a diagnosis of asthma13, 14. Spirometry with reversibility testing was also subsequently performed in those players who had a positive field provocation test. Players with a new diagnosis, or whose diagnosis was confirmed, or whose diagnosis was not confirmed were formally reviewed at a dedicated asthma clinic prior to either discontinuing or instigating therapy. Data were analysed using standard statistical methods with IBM SPSS Statistics v21. A p value less than 0.05 was deemed significant.
Results
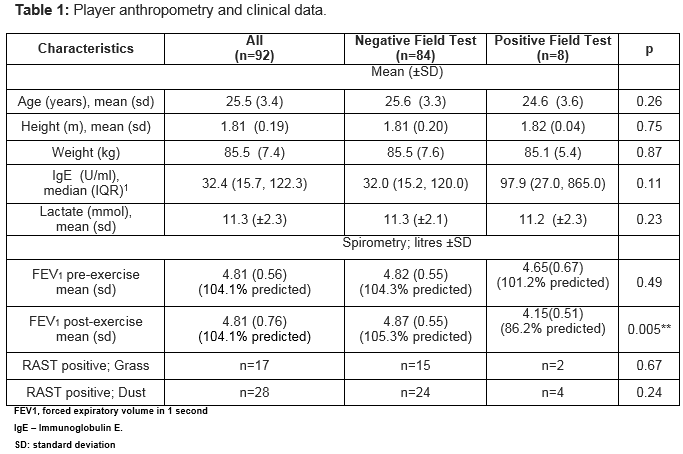
Ninety-two players were tested, of whom 12 players (13%) had previously been diagnosed with asthma or EIB (see Table 1). All players had elevated lactate levels at cessation of exercise indicative of supra-anaerobic threshold activity (normal value ≤4mmol). Ten players previously diagnosed with asthma/EIB were on regular treatment. Their medication was withheld in accordance with standard testing guidelines18. We identified EIB or asthma in 9/92 (9.8%) of our player cohort. However only three of the 9 diagnosed had a previous diagnosis of asthma/ EIB, and only two/12 of those previously labelled with EIB/asthma had a positive field based test result, while an additional subject had a negative field test but a positive bronchodilator response to inhaled Beta agonist (see figure 1).
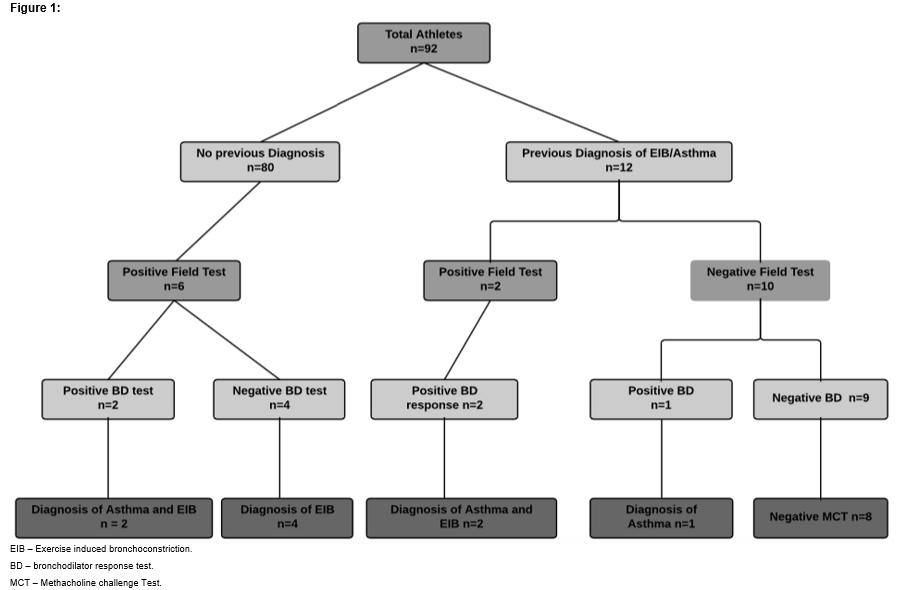 Subsequent laboratory-based testing on the 8 patients with EIB elicited a positive bronchodilator response in four players, including two subjects with, and two without a prior diagnosis of Asthma/EIB (see figure 1). It was found that in those players who had a negative field test, that anaerobic exercise precipitated a small (50ml) but statistically significant increase in average FEV1. One player with a prior physician diagnosis of EIB had a subsequent negative field test and no bronchodilator response but was unable to attend for a methacholine challenge. All other players in this category (8/9 players) had a methacholine challenge in addition to their field test and assessment for bronchodilator response, to insure that they were truly negative before ceasing therapy.
Subsequent laboratory-based testing on the 8 patients with EIB elicited a positive bronchodilator response in four players, including two subjects with, and two without a prior diagnosis of Asthma/EIB (see figure 1). It was found that in those players who had a negative field test, that anaerobic exercise precipitated a small (50ml) but statistically significant increase in average FEV1. One player with a prior physician diagnosis of EIB had a subsequent negative field test and no bronchodilator response but was unable to attend for a methacholine challenge. All other players in this category (8/9 players) had a methacholine challenge in addition to their field test and assessment for bronchodilator response, to insure that they were truly negative before ceasing therapy.
A raised IgE was utilised as a surrogate for atopy (an IgE level of >80units/ml) and was high in 32.5% of the players. Subjects previously labelled as asthmatic had a significantly higher IgE level (median IgE 28.8 U/ml vs. 242.0 U/ml, p=0.02). Although there was a trend towards a raised IgE in those diagnosed with EIB, this did not reach significance (97.9 U/ml vs. 32 U/ml, p=0.11) Allergen testing revealed that overall 17/92 players had raised allergen titres for grass pollen, with 28/92 players having raised titres against dust mite.
Discussion.
Our study achieved its primary target, which was to accurately determine the prevalence of EIB in a group of inter-county hurlers. The three team, 92-player cohort in this study reflects approximately 20% of those playing the sport at this elite level in Ireland. The player numbers are similar to those utilized in studies to determine EIB in other sports. The finding of asthma or EIB in 9.8% of our cohort is in line with reported prevalence of asthma in Ireland. We believe that the 8.7% prevalence of EIB reported in our study supports a roll for routine testing of those playing hurling. Furthermore, 6/8 of the EIB diagnoses were new while only 17% of players previously labeled with either EIB or asthma retained their diagnosis following the formal testing performed in this study. Similar findings amongst English professional soccer players were reported by Ansley et al 15. In that study sixty-five players with a physician diagnosis of asthma/EIB were referred for pulmonary function assessment. Of the 65 players assessed, 57 (88%) indicated regular use of asthma medication. Respiratory symptoms during exercise were reported by 57 (88%) players. Only 33 (51%) of the players tested had a positive bronchodilator or bronchial provocation test. Taken together, these results suggest that a group of players are being over-treated unnecessarily while a further group are being inadequately treated due to failure to diagnose the condition properly. Our results and those of others therefore highlight the requirement for objective testing to support a symptom-based diagnosis of asthma/EIB in athletes15.
The estimated prevalence of exercise-induced bronchoconstriction (EIB) varies from approximately 5 to 20 percent in the general population. The prevalence of EIB appears to be higher among elite athletes. In a study of 659 Italian Olympic athletes, the prevalence of exercise-induced bronchoconstriction was 14.7%16. Rates of 25% were reported amongst a group of elite long distance runners in Brazil17. In a Canadian group of athletes, 60% of swimmers, 29% of winter sport athletes, and 17% of controls had evidence of EIB18. In a study of varsity college athletes, 107 athletes from 22 sports participated, with 42 of 107 athletes (39%) found to be EIB positive19. In that particular study eucapnic voluntary hyperpnea test (EVH) was used as an indirect bronchoprovocation challenge, a method that can also be used to diagnosis EIB. Recent research by the same group demonstrated only 4 of 144 (2.7%) athletes were EIB-positive after EVH testing20. There is however a large discrepancy with regards to how EIB was classified and the testing criteria involved across these studies with EVH testing used in some instances but no formal field-testing being used in any of the studies. The high prevalence in winter sports athletes has been well documented where it is well known that cold air exposure over a prolonged period of time can act as an additional airway irritant21.
With over 32% of players in our study demonstrating evidence to support atopy and a significantly higher IgE level in those with a previous diagnosis of Asthma/EIB, it may be that symptoms associated with atopy e.g. rhinitis and hay fever and their associated negative effect on sporting performance may have played a role in the over diagnosis of asthma/EIB by physicians22. However, in contrast there was a trend towards raised IgE levels in those with EIB on formal testing. Furthermore, 17/92 players had raised allergen titers against grass pollen. This is of particular importance to this cohort as the game of hurling is typically played in the summer on grass fields when pollen counts are at their highest. One might therefore postulate that the results of our study may have been different if it had been performed during the summer rather than prior to the commencement of the main playing season (this was necessary to enable us to have access to the players). Field-testing of our cohort during the summer months may have yielded different results due to different pollen counts or possibly due to different ambient air temperature. Further studies examining the impact of performing player assessments at differing time points during the year are now required to answer this question. Given the contrasting signal from raised IgE levels this cannot currently be recommended to aid screening for EIB.
An early diagnosis of asthma or exercise induced bronchoconstriction in an athlete may prevent impaired performance that can ensue if preventative measures are not taken23. With drops in FEV1 of as much as 30% going undiagnosed in elite amateur athletes in this study, recognition and treatment of both pathologies would clearly be beneficial in maximizing player potential. Spirometry with reversibility and/or inhalation challenge may prove useful where exercise challenge testing is non-diagnostic but players' symptoms suggest asthma/EIB. It has previously been suggested that sports-specific exercise (as demonstrated in this field test) that produces the symptoms is most relevant for testing elite athletes24. As of yet there is no validated questionnaire available that may ease the screening burden25.
Acknowledgements;
This research was funded by the Wilton Respiratory Research Fund and a Denis O’ Sullivan Fellowship award (EH). The authors would like to thank the players, management and medical staff of the 2015 Kilkenny, Tipperary and Cork hurling squads for their participation in this study.
Conflict of Interest:
The authors have no financial conflicts of interest related to the contents of this manuscript.
Correspondence:
Dr. Desmond M Murphy, Consultant Respiratory Physician, The Department of Respiratory Medicine, Cork University Hospital, Cork, Ireland.
Tel: +353 214922327
Email: [email protected]
Bibliography
1. Parsons JP, Hallstrand TS, Mastronarde JG, Kaminsky DS, Rundell KW, Hull JH, Storms WW, Weiler JM, Cheek FM, Wilson KC, Anderson SD; American Thoracic Society Subcommittee on Exercise-induced Bronchoconstriction. An Official American Thoracic Society Clinical Practice Guideline: Exercise-induced Bronchoconstriction. Am J Respir Crit Care Med. 2013 May; 187(9):1016-1027.
2. Rundell KW, Im J, Mayers LB, Wilber RL, Szmedra L, Schmitz HR. Self-reported symptoms and exercise-induced asthma in the elite athlete. Med Sci Sports Exerc. 2001 Feb;33(2):208-13.
3. Holzer K, Anderson S D, Douglass J. Exercise in elite summer athletes: challenges for diagnosis. J Allergy Clin Immunol. 2002 Sep;110(3):374-80.
4. Parsons JP, Mastronarde JG. Exercise-induced bronchoconstriction in athletes. Chest. 2005;128(6):3966–3974.
5. Dickinson JW, Whyte GP, McConnell AK, Nevill AM, Harries MG. Mid-expiratory flow versus FEV1 measurements in the diagnosis of exercise induced asthma in elite athletes. Thorax. 2006 Feb;61(2):111-4.
6. Boulet LP, O’Byrne PM. Asthma and Exercise-Induced Bronchoconstriction in Athletes. N Engl J Med 2015; 372:641-648
7. Anderson SD, Kippelen P. Exercise- induced bronchoconstriction: pathogenesis. Curr Allergy Asthma Rep 2005 5:116-22.
8. Martin-Smith JD, Chan JC, Power KT, Crowley PJ, Clover AJ. Do helmets worn for hurling fail to protect the ear? Identification of an emerging injury pattern. Br J Sports Med. 2012 Dec;46(16):1134-6.
9. Falvey E, McCrory P, Crowley B, Kelleher A, Eustace J, Shanahan F, Molloy MG. Risk factors for hand injury in hurling: a cross-sectional study. BMJ Open 2013;3:e002634 doi:10.1136/bmjopen-2013
10. Blake C, O'Malley E, Gissane C, Murphy JC. Epidemiology of injuries in hurling: a prospective study 2007–2011 BMJ Open. 2014; 4(6): e005059. Published online 2014 Jun 18.
11. Juniper EF, O'Byrne PM, Guyatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire to measure asthma control. Eur Respir J. 1999 Oct;14(4):902-7.
12. Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M, Gibson P, Ohta K, O'Byrne P, Pedersen SE, Pizzichini E, Sullivan SD, Wenzel SE, Zar HJ. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008 Jan;31(1):143-78.
13. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, Jensen R, Johnson DC, MacIntyre N, McKay R, Navajas D, Pedersen OF, Pellegrino R, Viegi G, Wanger J; ATS/ERS Task Force. Standardisation of spirometry Eur Respir J. 2005 Aug;26(2):319-38.
14. Crapo RO, Casaburi R, Coates AL, Enright PL, Hankinson JL, Irvin CG, MacIntyre NR, McKay RT, Wanger JS, Anderson SD, Cockcroft DW, Fish JE, Sterk PJ. Guidelines for methacholine and exercise challenge testing-1999. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. Am J Respir Crit Care Med. 2000 Jan;161(1):309-29.
15. Ansley L, Kippelen P, Dickinson J, Hull JH. Misdiagnosis of exercise-induced bronchoconstriction in professional soccer players. Allergy. 2012 Mar;67(3):390-5.
16. Bonini M, Gramiccioni C, Fioretti D, Ruckert B, Rinaldi M, Akdis C, Todaro A, Palange P, Carlsen KH, Pelliccia A, Rasi G, Bonini S; AIDA and the Italian Unit of the GA2LEN Olympic Study. Asthma, allergy and the Olympics: a 12-year survey in elite athletes. Curr Opin Allergy Clin Immunol. 2015 Apr;15(2):184-92.
17. Teixeira RN, Teixeira LR, Costa LA, Martins MA, Mickleborough TD, Carvalho CR Exercise-induced bronchoconstriction in elite long-distance runners in Brazil. SOJ Bras Pneumol. 2012 May-Jun;38(3):292-8.
18. Bougault V, Turmel J, Boulet LP. Bronchial challenges and respiratory symptoms in elite swimmers and winter sport athletes: Airway hyperresponsiveness in asthma: its measurement and clinical significance. Chest. 2010 Aug;138(2 Suppl):31S-37S.
19. Parsons JP, Kaeding C, Phillips G, Jarjoura D, Wadley G, Mastronarde JG. Prevalence of Exercise-Induced Bronchospasm in a Cohort of Varsity College Athletes Med Sci Sports Exerc. 2007;39(9):1487-1492.
20. Parsons JP, Cosmar D, Phillips G, Kaeding C, Best TM, Mastronarde JG. Screening for exercise-induced bronchoconstriciton in college athletes. J Asthma. 2012 Mar;49(2):153-7
21. Carlsen KH. Sports in extreme conditions: the impact of exercise in cold temperatures on asthma and bronchial hyper-responsiveness in athletes. Br J Sports Med. 2012 Sep;46(11):796-9.
22. Dijkstra H, Robson-Ansley P. The prevalence and current opinion of treatment of allergic rhinitis in elite athletes. Current Opinion In Allergy & Clinical Immunology. 2011, Apr; 11(2): 103-108 6p
23. Price OJ, Hull JH, Backer V, Hostrup M, Ansley L. The impact of exercise-induced bronchoconstriction on athletic performance: a systematic review. Sports Med 2014;44:1749-61.
24. Rundell KW, Wilber RL, Szmedra L, Jenkinson DM, Mayers LB, Im J. Exercise-induced asthma screening of elite athletes: field versus laboratory exercise challenge. Med Sci Sports Exerc 2000;32:309–16.
25. Weiler JM, Hallstrand TS, Parsons JP, Randolph C, Silvers WS, Storms WW, Bronstone A. Improving screening and diagnosis of exercise-induced bronchoconstriction: a call to action. J Allergy Clin Immunol Pract. 2014 May-Jun;2(3):275-80.
(P655)