Identifying factors that influence the ‘6-hour target’ in the Emergency Department by applying Regression Analysis.
F Borhan1, N Borhan1, S Ahmed2, L Varghese1, E O’Conor1.
1Emergency Department, Connolly Hospital, Blanchardstown, Dublin 15, Ireland.
2Government Health and Human Services Analytics, IBM Watson Health, Dublin 15, Ireland.
Abstract
Aim
To determine factors within the Emergency Department (ED) that have maximum influence on the ‘6-hour target’.
Methods
Regression Analysis methodology employed to analyse the influence of 9 ED variables on the ‘6-hour target’ compliance.
Results
The number of patients waiting to be seen an ED physician at 8pm exerts maximum influence on the ‘6-hour target’ (r = -0.581, p<0.05).
Conclusion
The ‘6-hour target’ compliance rises with lesser number of patients waiting to be seen by an ED physician at 8pm. Also, the ‘6-hour target’ compliance rises by increasing the number of ED Registrar working hours and the number of ED SHO working hours per day.
Introduction
The Emergency Medicine Programme in Ireland recommends a national Total ED Time (TEDT) standard of 95% of patients having their emergency care completed within 6 hours of arrival in an ED1. Numerous factors influence our ability to meet Patient Experience Time (PET) targets. Consequent to our pilot study in May 20152, the aim of this study is to determine those factors within the ED that had maximum influence on the ‘6-hour target’ compliance for all patients presenting to the ED over a 24 hour period.
Methods
A qualitative retrospective study was conducted in the Emergency Department of Connolly Hospital, Blanchardstown, Dublin 15, Ireland. Variables for the study were chosen on the knowledge of our senior physician that were felt to influence PET and recorded for each day from 1st July 2015 to 31st December 2015. The variables included: 1. TBS8AM - Number of patients waiting to be seen by an ED physician at 8am each day, 2. TBS8PM- Number of patients waiting to be seen by an ED physician at 8pm each day, 3. NEWATT- Total number of new ED attendances over 24 hours, 4. ADM8AM- Number of boarded inpatients in ED at 8am each day, 5. ADM8PM- Number of boarded inpatients in ED at 8pm each day, 6. SHOHRS- Total number of ED Senior House Officer working hours per day, 7. REGHRS- Total number of ED Registrar working hours per day, 8. ANP- Total number of Advanced Nurse Practitioner working hours per day, 9. CNS- Total number of Clinical Nurse Specialist working hours per day, 10. PET6- Percentage compliance with the '6-hour target' for all patients over a 24 hour period, 11. PET6NA- Percentage compliance with the '6-hour target' for non-admitted patients over a 24 hour period. These 11 variables were extracted from the ED Nursing handover logbook, the ED electronic database, ’Symphony’ and the clinical staff rosters. Variables for the timings of 8am and 8pm were chosen as these are ED staff changeover timings. A Regression analysis methodology was performed using SPSS to determine variables that had maximum influence on the PET6 and PET6NA.
Results
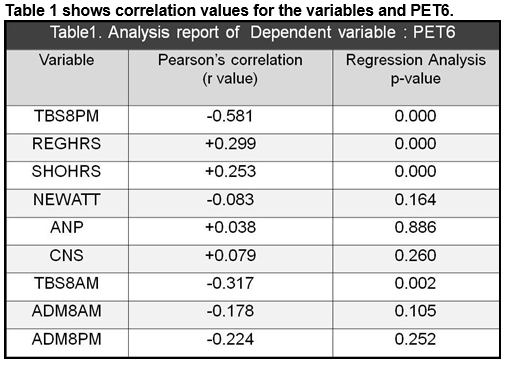 TBS8PM exerts maximal negative and strong association for the PET6 (r = -0.581, p<0.05).
TBS8PM exerts maximal negative and strong association for the PET6 (r = -0.581, p<0.05).
Therefore, the lesser number of patients waiting to be seen by an ED physician at 8pm, the higher the percentage compliance for the '6-hour target' for all patients presenting to the ED over 24 hours. A second important finding was that the REGHRS exerts a positive association for the PET6 (r =+0.299, p<0.05) and SHOHRS exerts a positive association for the PET6 (r =+0.253, p<0.05). Therefore, the compliance for the '6-hour target' rises by increasing the number of ED Registrar working hours per day and by increasing the number of ED Senior House Officer working hours per day. Of the factors influencing PET6NA, TBS8PM held maximum correlation (r = -0.629, p<0.05), similar to the result of our pilot study2.
Discussion
Our study concluded that the ‘6-hour target’ compliance increases with lesser number of patients waiting to be seen by an ED physician at 8pm. Also, the ‘6-hour target’ compliance rises by increasing the number of ED Registrar working hours and ED SHO working hours per day. The total number of new ED attendances per day exerts a negative correlation for the ‘6-hour target’. A study showed that higher-volume EDs may be more crowded, increasing wait times and visit lengths3.The ANP and CNS hours exerts a positive correlation for the ‘6-hour target’. Improved ED performance with nurse practioners has been demonstrated in other studies4. Numerous studies have shown improved wait time or length of visit after improvements in ED throughout, including changes in triage, laboratory testing, staffing, or combinations thereof5-8.Our study was limited in that, factors such as laboratory processing time for blood test results, time delay resulting from radiological imaging and reporting, were not included. Previous studies have looked at the association between overcrowding and the 4-hour rule9,10. Our study is unique in that it employs other factors from the Emergency Department and analyses their influence on the ‘6-hour target’ compliance. Monitoring identified easily retrievable factors in our ED that affect PET targets, help to better understand performance and demonstrate improvement towards achievement of the standard.
Conflict of Interest
The authors report no conflict of interest.
Correspondence:
Dr. Fareeda Borhan, Emergency Department, Connolly Hospital, Blanchardstown, Dublin 15, Ireland.
Email: [email protected]
References
1. The National Emergency Medicine Programme Report , June 2012.
2. Borhan F, Ahmed S, Varghese L, O’Conor E. A Statistical Methodology to determine factors affecting Patient Experience Time Targets in the Emergency Department. IMJ. 2017; 110(1):506.
3. Asplin BR, Magid DJ, Rhodes KV, Solberg LI, Lurie N, Camargo CA., Jr. A conceptual model of emergency department crowding. Ann Emerg Med. 2003 Aug;42(2):173–180.
4. Carter AJE, Chochinov AH. A systematic review of the impact of nurse practitioners on cost, quality of care, satisfaction and wait times in the emergency department. Can J Emerg Med care. 2007;9:286–295.
5. Partovi SN, Nelson BK, Bryan ED, Walsh MJ. Faculty triage shortens emergency department length of stay. Acad Emerg Med. 2001 Oct;8(10):990–995.
6. Holland LL, Smith LL, Blick KE. Reducing laboratory turnaround time outliers can reduce emergency department patient length of stay: an 11-hospital study. Am J Clin Pathol. 2005 Nov;124(5):672–674.
7. Bucheli B, Martina B. Reduced length of stay in medical emergency department patients: a prospective controlled study on emergency physician staffing. Eur J Emerg Med. 2004 Feb;11(1):29–34.
8. Fernandes CM, Christenson JM, Price A. Continuous quality improvement reduces length of stay for fast-track patients in an emergency department. Acad Emerg Med. 1996 Mar;3(3):258–263.
9. Geelhoed G, De Klerk N. Emergency department overcrowding, mortality and the 4-hour rule in Western Australia. Medical Journal of Australia. 2012;196:122-126
10. Vegting IL, Alam N, Ghanes K, Jouini O, Mulder F, Vreeburg M, Biesheuvel T, van Bokhorst J, Go P, Kramer MH, Koole GM, Nanayakkara PW. What are we waiting for? Factors influencing completion times in an academic and peripheral emergency department. Netherlands J Med 2015; 73 7:331–340.
(P699)
