Iron Refractory Iron Deficiency Anaemia: A Rare Cause of Iron Deficiency Anaemia
T McGrath1, M Cotter2
1Temple Street Children’s University Hospital, Dublin
2Consultant Paediatric Haematologist, Temple Street Children’s University Hospital, Dublin
Abstract
We describe the case of a 17-month-old boy with a hypochromic microcytic anaemia, refractory to oral iron treatment. After exclusion of dietary and gastrointestinal causes of iron deficiency, a genetic cause for iron deficiency was confirmed by finding two mutations in the TMPRSS6 gene, consistent with a diagnosis of iron-refractory iron deficiency anaemia (IRIDA).
Introduction
Iron deficiency anaemia (IDA) is the most common nutritional deficiency which represents a major public health problem worldwide1. Infants between the ages of six months and two years are at a high risk of developing IDA2. The most common causes of IDA include insufficient dietary intake coupled with rapid growth, prematurity and excessive consumption of cow’s milk. Other causes include conditions causing malabsorption such as coeliac disease1. IDA can adversely affect neurodevelopment. It is treated with supplemental and increased dietary iron intake. In cases where IDA is non-responsive to oral iron treatment, rarer inherited causes of IDA must be considered3.
Case Report
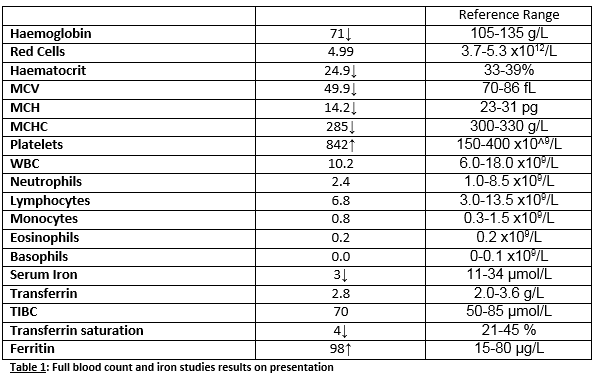
A 17-month-old boy was referred with a six month history of pallor associated with a hypochromic microcytic anaemia and low serum iron. He had no significant past medical history and was thriving on the 91st centile (weight). His full blood count showed a marked hypochromic microcytic anaemia with low iron but normal ferritin levels (Table 1). His blood film showed markedly hypochromic microcytic red cells and plentiful pencil cells. His iron deficiency was not explained by his diet, gastrointestinal or other symptoms. He was commenced on standard treatment doses of oral iron but his anaemia did not respond despite compliance.
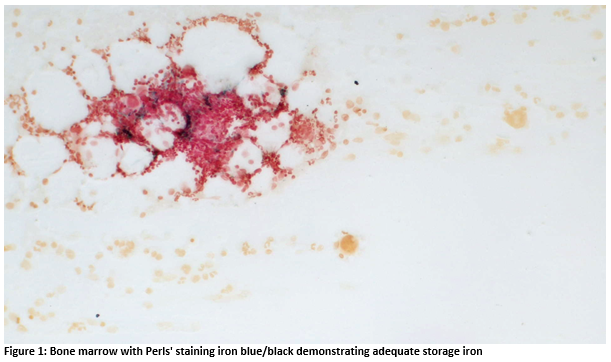
Further investigations revealed a normal haemoglobinopathy screen, globin gene study; negative coeliac screen, occult blood and Meckel’s scan. A bone marrow biopsy showed adequate iron storage in the marrow but none in erythroblasts.
His anaemia was refractory to oral iron and as no other causes of iron deficiency were identified, a diagnosis of iron refractory iron deficiency anaemia (IRIDA) was considered. Sequencing of TMPRSS6 gene revealed compound heterozygosity for mutations (c.1468-1468+3dupGGTG and c.1813delG) consistent with an IRIDA diagnosis. The mutation c.1468-1468+3dupGGTG is predicted to result in abnormal splicing of exon 12. The mutation c.1813delG has previously been reported in homozygous form in a patient with IRIDA, resulting in a frameshift and premature STOP codon4. Subsequently he received several doses of intravenous iron sucrose 200mg with significant improvement in his haemoglobin and red cell indices; Hb 114g/L, MCV 75fL and MCH 25pg. His Hb and MCV has been shown to decrease over time and he has received further intravenous iron infusions when Hb falls to <90g/L, with ferritin monitoring to avoid iron overload.
Discussion
IRIDA is an autosomal recessive condition causing severe iron deficiency, minimally responsive to oral iron therapy. The genetic basis of this disorder was elucidated in recent years, resulting from germline mutations in TMPRSS6, encoding matriptase-24. Matriptase-2 is a type II transmembrane serine protease which plays an essential role in downregulating hepcidin expression in liver cells. Hepcidin is a peptide synthesized by the liver which is now regarded as the master regulator of iron homeostasis. Hepcidin limits iron absorption by the gut and release of storage iron from macrophages4. Typically in iron deficiency, hepcidin levels are reduced. However in IRIDA, the levels are normal or increased. Mutations in TMPRSS6 result in decreased catalytic activity of matriptase-2, which in turn upregulates hepcidin levels, decreasing iron absorption and release from stores3.
Patients with IRIDA are generally diagnosed during childhood. After exclusion of the usual causes of iron deficiency (including inadequate diet, malabsorption or blood loss, and chronic inflammatory conditions), features of IRIDA include a hypochromic microcytic anaemia with a profound degree of microcytosis, very low serum iron and transferrin saturation, in association with a low/normal serum ferritin. The degree of microcytosis (MCV 49.9fL in this case) and hypochromia are usually disproportionate with the level of anaemia. IRIDA diagnosis is supported by failure to respond to oral iron administration; accordingly patients must be treated with parenteral iron4. The response to parenteral iron treatment is variable but it will correct at least partially haemoglobin levels and red cell indices, MCV and MCH3. To our knowledge, this is the first such case identified in the Irish population.
Acknowledgements: We are grateful to the laboratory of Professor Bernard Grandchamp at the Hôpital Bichat Claude Bernard in Paris carried out the genetic analysis.
Conflict of Interest:
The authors declare no conflicts of interest.
Correspondence:
T McGrath, Temple Street Children’s University Hospital, Dublin
Email: [email protected]
References
1. World Health Organization. Iron deficiency anaemia: assessment, prevention and control. 2001. Accessed Nov 2016. Retrieved from: http://apps.who.int/iris/bitstream/10665/66914/1/WHO_NHD_01.3.pdf?ua=1
2. Lozoff B, Kaciroti N, Walter T. Iron deficiency in infancy: applying a physiologic framework for prediction. Am J Clin Nutr. 2006; 84(6):1412-1421
3. De Falco L, Sanchez M, Silvestri L, Kannengiesser C, Muckenthaler MU, Iolascon A, Gouva L, Camaschella C, Beaumont C. Iron refractory iron deficiency anemia. Haematologica. 2013; 98 (6):845-853
4. Finberg KE, Heeney MM, Campagna DR, Aydinok Y, Pearson HA, Hartman KR, Mayo MM, Samuel SM, Strousse JJ, Markjanos K, Andrews NC, Fleming MD. Mutations in TMPRSS6 cause iron-refractory iron deficiency anemia (IRIDA). Nat Genet. 2008; 40(5): 569-571 Available from doi: 10.1038/ng.130 [Accessed 12th May 2016]
5. Keskin EY, Yenicesu I. Iron-Refractory Iron Deficiency Anemia. Turk J Hematol. 2015; 32:1-14
P678