Key Performance Indicators in Paediatric Anaesthesia
K. Doody, D. Barry, C. Holmes
Department of Anaesthesiology, Temple Street Children’s University Hospital, Dublin
Abstract
Aims
Currently no national guidelines on performance measurement exist for paediatric anaesthesia in Ireland1. The purpose of this study was to ascertain if we are achieving Key Performance Indicators (KPIs) in areas of post-operative nausea and vomiting (PONV) and post-operative pain when compared to international standards.
Methods
The study was carried out from January 2018 to February 2018 at Temple Street Children’s University Hospital. In total 743 patients were included.
Results
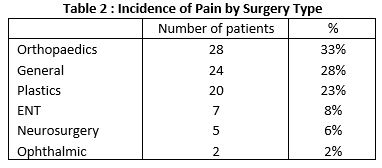
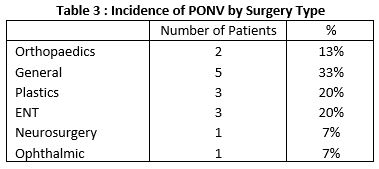
743 patients were included in the study. 86 (12%) were recorded as having a post-operative pain score of >4/10. 15 (1.2%) of patients were recorded as experiencing PONV. Orthopaedic surgery had the highest frequency of post-operative pain accounting for 33% of all cases. General surgery was associated with highest risk of PONV.
Discussion
The results from the study indicate we are achieving results similar to data from international centres. There is a paucity of published data from Irish centres and as national guidelines are developed for a model of care for paediatric anaesthesia we hope this data can be used when comparing other paediatric centres within Ireland.
Introduction
Performance measurement is the process of collecting, analysing and/or reporting information regarding the performance of an individual, group, organisation, system or component1. It has been widely accepted that anaesthesia is at the forefront of patient safety2. Morbidity and mortality are therefore poor performance measures in anaesthesia given their relatively rare occurrence3.According to Benn one method to assess the quality of anaesthetic technique is to “assess the patients’ experience of recovery”. ”. Many Key Performance Indicators can be assessed such as post-operative delirium, respiratory complications and hypothermia. Outcomes such as PONV and post-operative pain in particular have negative consequences for patients and were the focus of this study.The APAGBI 2016 states postoperative vomiting is approximately twice as frequent amongst children. It is one of the leading causes of parental dissatisfaction after surgery and is the leading cause of unanticipated hospital admission following ambulatory surgery with resulting increased health care costs. Post-operative paediatric pain “has remained undertreated because of difficulty in pain assessment and concerns regarding side effects of opioid analgesics”4. It has been shown, despite the increase in scientific knowledge regarding the negative consequences of post-operative pain, many children still “experience unnecessary pain” during their hospital stay5.
Methods
A prospective observational audit was carried out over a 2 month period starting in January 2018.. All patients who attended the post-operative care unit (PACU) had pain scores recorded. Any patients experiencing post-operative nausea and vomiting were recorded. The data was collected by the recovery nursing staff. A standardised form for recording of patient details was utilized to minimize recording bias. The scoring systems utilized by the nursing staff for pain assessment included the visual analog scale, FLACC scale and the Wong-Baker scale depending on the age of the patient and if they were verbal or non-verbal In-service training was carried out to reinforce the importance of accurate pain assessment and record .
An incidence of less than 2% for PONV and less than 10% for post-operative pain was used as a benchmark and are the Key Performance targets set by Great Ormond Street Hospital.6
Results
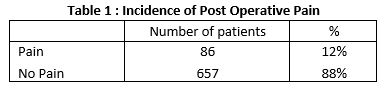
In total 743 patients were included over the 2 month period from 1st January 2018 to the 28th of February 2018. 86 patients (12%) were recorded as having a post-operative pain score of >4/10 (Table 1). The incidence of post-operative pain for different types of surgery can be seen in table 2.
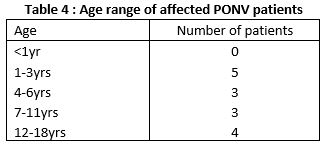
15(1.2%) of patients were recorded as experiencing PONV which was distributed through various types of surgery as seen in table 3. This was distributed evenly through different age groups (table 4)
Discussion
There is recognition in the model of care for paediatric anaesthesia by the HSE that “clinicians and non-clinical personnel working in paediatric anaesthesia require easily measureable, consistent and definable clinical and non-clinical outcomes for paediatric anaesthesia that are applicable nationally”. Post-operative pain and PONV meet both of these criteria and is the reason why the study focused on these parameters as measures of “performance”. A large number of paediatric patients were chosen in an effort to be truly representative of the actual incidence of PONV and post-operative pain in the PACU. The setting of measurable standards and performance targets is important and can be compared to international standards.
There is a greater emphasis on performance and quality measurement both at a national and international level. Post-operative pain and PONV are two of the most important markers of quality of post-operative recovery7. PONV and post-operative pain can have negative consequences in paediatric surgery and can cause unnecessary distress and anxiety.
The results show a low incidence of PONV in PACU with an incidence of just 1.2%. This is well below the Key Performance benchmark used by Great Ormond Street. Previously published work indicate the incidence for PONV is much more frequent in the paediatric population when compared to the adult population with an incidence ranging from 13-42% reported 8,9. These results are comparable with previous audits carried out within the department. One possible reason the incidence is lower than previously published work is that the study looks only at incidence of PONV in the PACU and may be higher if patients followed up for 24 hours after operation. The results however do indicate the incidence of PONV in Temple Street Children’s University Hospital is low and when compared internationally the rates of PONV in PACU we are meeting internationally recognised key performance indicators. We suggest a number of factors may contribute to the low rate. Regional techniques are routinely integrated into the multi-modal analgesia approach to post –operative pain management. There is also strong adherence to shorter fasting times and ensuring children take clear fluids until 60 minutes prior to surgery may result in less dehydration which is a known risk factor for PONV. The use of anti-emetics is at the discretion of consultant anaesthetist depending on type of surgery, age of patient and other risk factors for PONV.
The results from the second KPI shows that 12% or 86 patients experienced a pain score of greater than 4/10.41.9% of these were in the 1-3 year age group. We apply the same target as Great Ormond Street Hospital and Cincinnati Children’s Hospital – seeking to achieve more than 90 per cent of children arriving to recovery with pain score less than 4/10. Despite being just short of this result, we are committed to continuous improvement, so we expect to increase this score over time following departmental feedback and re-audit. It is important to aggressively prevent and treat pain as emerging evidence indicates that pain in paediatric patients can produce changes in sensory processing and future pain responses10. In ensuring appropriate management of post-operative pain it is vital to ensure the safety and efficacy of pain relief in both the immediate recovery phase and upon discharge from the PACU. There is a recognition however that whilst the evidence base for the management of post-operative pain in paediatrics is increasing, it is only through audit and quality improvement strategies we can achieve this11.
Our study demonstrated a very low incidence of PONV and an incidence of post-operative pain which was slightly greater than targets set by Great Ormond Street. As national guidelines currently do not exist exist the results from this study illustrate what is achieved in the second tertiary hildren’s hospital in Ireland. It is important to point out the study has some limitations. The data was recorded exclusively from the PACU. The time to discharge from the PACU varied depending on the age of patient and case complexity but was often less than 30 minutes. The incidence of PONV and post-operative pain may be higher if the patients were followed for a longer time period. In developing guidelines it would be important to consider not only what is appropriate to measure but also when should it be measured. PONV and post-operative pain according to the Model of Care for Paediatric Anaesthesia are amongst the top outcome measures for the evaluation of clinical paediatric anaesthesia service delivery.
The successful implementation of performance measurement within paediatric or any healthcare setting will face obvious barriers. Previous studies have identified several barriers to quality improvement. These include a lack of credible data, clinicians being unaware that an issue exists, lack of hospital resources and lack of supportive management at a local level12. The basis for performance measurement and ultimately quality improvement is to look at current standards of care and where can they be improved upon. If a variation in the level of care delivered is occurring, it is important to ascertain the reasons for this occurring and to evaluate the impact of changes to the service3. The implication of a higher than acceptable level of PONV or post-operative pain can lead to unplanned admissions for ambulatory surgery, causing both distress to patients and a higher associated healthcare cost. The primary aim of this study was to provide data on a large cohort of patients which can be used as a baseline to guide improvements to service delivery.
In conclusion PONV and post-operative pain according to the Model of Care for Paediatric Anaesthesia are amongst the top outcome measures for the evaluation of clinical paediatric anaesthesia service delivery. This study attempts to establish baseline performance standards for paediatric anaesthesia in Ireland using a large patient cohort from Temple Street Children’s University Hospital. The results from the study indicate we are achieving results similar to data from international centres. There is a paucity of published data from Irish centres and as national guidelines are developed for a model of care for paediatric anaesthesia we hope this data can be used when comparing other paediatric centres within Ireland.
Conflicts of Interest Statement
The authors have no conflict of interest in relation to the subject matter in this manuscript.
Corresponding Author
Kevin Doody
Specialist Registrar in Anaesthesiology
Cork University Hospital
E-mail: [email protected]
References
1. HSE. Model for Care for Paediatric Anaesthesia. 2015.
2. DM G. Anaesthesiology as a model for patient safety in health care. Bmj. 2000;
3. Benn J, Arnold G, Wei I, Riley C, Aleva F. Using quality indicators in anaesthesia: Feeding back data to improve care. British Journal of Anaesthesia. 2012.
4. Lee JY, Jo YY. Attention to postoperative pain control in children. Korean Journal of Anesthesiology. 2014.
5. Linhares MBM, Doca FNP, Martinez FE, Carlotti APP, Cassiano RGM, Pfeifer LI,. Pediatric pain: prevalence, assessment, and management in a teaching hospital. Brazilian J Med Biol Res. 2012;
6. Hospital GOS. Anaesthesia Clinical Outcomes Great Ormond Street Hospital [Internet]. [cited 2019 Feb 20]. Available from: https://www.gosh.nhs.uk/health-professionals/clinical-outcomes/anaesthesia-clinical-outcomes
7. Macario A, Weinger M, Carney S, Kim A. Which clinical anesthesia outcomes are important to avoid? The perspective of patients. Anesth Analg. 1999;
8. LUNN JN. Implications of the National Confidential Enquiry into Perioperative Deaths for paediatric anaesthesia. Pediatr Anesth. 1992;
9. Lunn JN, Devlin HB, Hoile RW, Campling Ncepod EA. Editorial II-the national confidential enquiry into perioperative deaths. British Journal of Anaesthesia. 1993.
10. Walker SM. Biological and neurodevelopmental implications of neonatal pain. Clinics in Perinatology. 2013.
11. Walker SM. Pain after surgery in children. Curr Opin Anaesthesiol. 2015;
12 de Vos M, Graafmans W, Kooistra M, Meijboom B, Van Der Voort P, Westert G. Using quality indicators to improve hospital care: a review of the literature. Int J Qual Heal Care. 2009;
Issue: Ir Med J; Vol 112; No. 6; P948
