Magnetic Stent Removal in a Nurse-Led Clinic; a Nine-Month Experience.
O’Connell L, Broe MP, Rooney D, Elhag S, Cheema I, McGuire BB.
Department of Urology, James Connolly Memorial Hospital Blanchardstown, Dublin 15, Ireland
Abstract
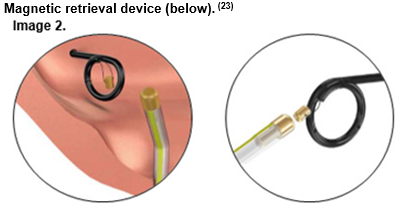
Ureteric stents are frequently inserted post endourological procedures. However, subsequent endoscopic stent removal requires a second procedure for the patient and the availability of necessary resources. Longer duration of indwelling stents can lead to increased risk of symptoms and complications. The use of magnetic stents removed with a magnetic retrieval device (BlackStar©), offers an alternative which obviates the need for cystoscopy. We assessed the outcomes for this novel method of stent removal in our institution. A retrospective analysis was performed of all patients undergoing magnetic stent insertion and subsequent removal in a nurse-led clinic over a nine-month period. Patients were followed up with a prospective validated Ureteral Stent Symptoms Questionnaire (USSQ)3. A cost analysis was also performed. In total, 59 patients were treated using magnetic stents. The complication rate was low (6.7%). The median duration of indwelling stent was 5.8 days (range 1-11 days). Patients reported haematuria and lower urinary tract symptoms but >90% experienced no functional impairment with minimal days of employment lost (mean 0.75 days). All patients reported satisfaction with nurse-led stent removal and 97% were happy to have stents removed via this method in the future. The total financial savings were estimated at €47,790 over this period. Nurse-led removal of magnetic stents is safe and well tolerated by patients and enables expedient stent removal. It also provides a significant cost benefit and frees up valuable endoscopic resources.
Introduction
The double J ureteric stent was first described by Mr Roy Finney in 19781. Since then, they have been one of the most important tools at the disposal of the urologist. They are frequently inserted post endourologic procedures to maintain patency and provide drainage of the upper urinary tract2. However, ureteric stents can be associated with symptoms such as haematuria, frequency, urgency and flank pain in up to 80% of patients2,3. Furthermore, the subsequent removal necessitates a second endoscopic procedure in the form of either rigid or flexible cystoscopy. This procedure can be uncomfortable for patients as it is usually performed under local anaesthetic4. Stent removal also requires significant resources in the form of access to endoscopy services, availability of a day-care bed and a urologist to perform the task.
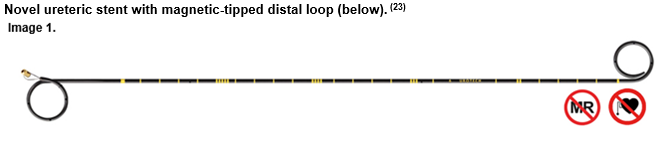
The use of a magnetic tip for stent retrieval was first reported in 19895. However, since then more of the research and development focus has been on stent materials. The ‘BlackStar© System’ was developed more recently. While the main body of the stent is polyurethane, similar to standard double J stents already in use, the distal tip of the stent and retrieval catheter are treated with biocompatible magnetised compounds. This system allowed successful retrieval of all stents in the preliminary technical data published in 2014.7 The magnetic stent is inserted cystoscopically in a manner identical to a standard JJ stent. Care is taken to ensure the ring with magnetic properties slides over the guide wire behind the tip of the stent. The magnetic tipped stent allows for stent removal with a catheter-like retrieval device, negating the need for cystoscopic removal. A new nurse-led stent removal clinic was established in our institution in September 2015. Patients attended for stent removal via the magnetic retrieval device described above. We report our early experience with this novel method, with focus on peri-procedural outcomes, patient satisfaction and cost savings.
Methods
A retrospective analysis was performed of all patients who underwent magnetic stent insertion and subsequent removal in a nurse-led clinic at our institution over a nine-month period. All indications for stent insertion were included. No patients were excluded or lost to follow up. Data collected included: patient demographics, procedure type, indication for stenting, procedure length, nature of admission (elective or emergency), duration of hospital stay, duration of indwelling stent and incidence of complications.
Furthermore, patients were prospectively assessed for stent-associated symptoms and quality of life impact by completing a validated stent symptom questionnaire8. The Ureteral Stent Symptom Questionnaire (USSQ) evaluates 6 domains including urinary symptoms, stent pain, impact on general health and functioning, ability to work and total working days lost due to symptoms. It also used to assess for stent related complications. Additionally, patient satisfaction with the novel nurse led clinic and the catheter retrieval technique were also evaluated in the questionnaire. A cost analysis was carried out to estimate the expense associated with stent removal in the nurse-led clinic setting compared to traditional cystoscopic removal of stent. Costings were obtained from the hospital finance and purchasing departments.
Results
A total of 59 patients were treated with magnetic stent insertion over the nine-month interval (n=59). The indication for stenting in all patients was urinary calculi. Magnetic stents were not used for patients requiring insertion of a long term indwelling stent. The majority of cases were performed as day case elective procedures (63%), the remaining 47% were from emergency admissions or inpatient consultations. The mean length of hospital stay for those who were operated on during an inpatient admission was 2.8 days (range 1-9).
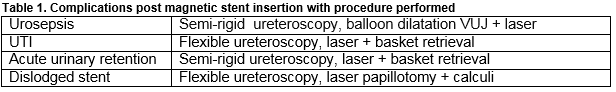
Flexible ureteroscopy was performed in 83.7%, semi-rigid ureteroscopy in 10.8%, and a combination of both methods in 5.4%. Ureteric access sheaths were employed in 32.4% and balloon dilatation of the ureteric orifice was carried out in 8.4% of cases. The median duration of indwelling stent was 5.8 days (range 1-11 days). There was a total of four stent related complication (6.7%). This included one urosepsis, one urinary tract infection and one spontaneously dislodged stent (Table 1). There were no failed stent retrievals by the nurse specialist over the duration of the study period and no stents lost to follow up.
The response rate to the USSQ questionnaire was 67.8%. Patients reported a high incidence of stent related symptoms such as haematuria (52%), dysuria (63%) and stent discomfort (69%). However, only 30% of patients were significantly bothered by their symptoms. One quarter described debilitating pain secondary to the indwelling stent. Most patients (>90%) experienced no functional impairment due to their symptoms. Symptoms resulted in few working days lost (mean 0.75 days) for those in employment. With regard to stent removal, 90.7% patients reported that they were either ‘satisfied’ or ‘very satisfied’ with their experience in the nurse-led clinic. In total, 97% of respondents stated that they would be happy to have a stent removed via this method in the future. Of the 22 patients who had had previous cystoscopic removal of ureteric stent 71% preferred the magnetic method of removal versus the traditional method.
The potential financial benefits were estimated via Health Inpatient Enquiry (HIPE) analysis at mean savings of €200-€810 per procedure, with a total potential savings of €47,790 over the nine months.
Discussion
Ureteric stents perform a vital role in maintaining patency and drainage of the upper urinary tract. As mentioned above, they are unfortunately associated with significant symptoms and also complications. Up to 80% of patients with indwelling ureteric stents experience symptoms which are sufficiently severe to affect their quality of life and functional capacity2,9,10,11,12,13. In addition, up to 45% of patients require some leave of absence from work due to stent symptoms in the first two weeks, with a further 32% of patients who remained stented at 30 days unable to return to work during this time3. The substantial economic cost of this morbidity has been previously reported.14 Whilst stent composition does not appear to exert an influence, certain technical factors such as excessive stent length, stent diameter and the presence of a distal loop crossing the midline seem to increase symptoms3,15,16. Patient factors including age, sex and BMI also play a role15. Haematuria and lower urinary tract symptoms were the most frequent and bothersome stent symptoms described by patients in this study, with rates comparable to those reported elsewhere in the literature2,3. Stent symptoms typically persist for the duration of the stent dwell time, and therefore the ideal method of minimizing them is timely removal of the stent. One significant benefit of a nurse-led clinic is that it facilitates early stent removal. The mean time of indwelling stent in our study was less than 6 days. No complications arose as a result of early stent removal.
The process of cystoscopic stent removal can be uncomfortable for patients4. Alternative non-endoscopic methods of stent removal have been investigated. These include magnetic retrieval devices such as in this study and stents with extraction strings. Extraction stringed stents do not appear to cause any increase in morbidity while the stent is indwelling17 and cause less discomfort at the time of removal than flexible cystoscopy18. However, they are prone to inadvertent early dislodgement19. Patients in this study reported overall satisfaction with the magnetic system of stent removal. The majority of those who had undergone previous stenting preferred magnetic retrieval to the alternative method of removal via flexible cystoscopy.
Dissolvable or biodegradable stents are an alternative solution to the issue of the optimal method of stent removal which have been under investigation since the 1990s20. The obvious benefits include the absence of a second procedure for stent removal and the avoidance of the situation of a forgotten stent. The most recent biodegradable stents are dissolved over a period of 2-8 weeks. Whilst in-vitro trials appear promising, no in-vivo studies have yet been undertaken10. Therefore, the benefits of the stent removal system reported in our study are particularly relevant in the absence of established non-endoscopic alternatives.
Finally, the cost of cystoscopic stent removal is an important factor, not only the financial cost but also time and resource allocation. The absolute financial cost of cystoscopic stent removal has been estimated at 128USD per procedure21. This is based on the American system of office-based urological procedures, whereas in Ireland it is certainly more expensive. In addition to the financial cost, there remains the burden on diagnostic cystoscopy services and the opportunistic cost of the urologist’s time. In Australia, the introduction of nurse-led flexible cystoscopy for surveillance of bladder tumours has been successful in reducing waiting times for this service by 65%22. Our study has found significant cost savings associated with the avoidance of formal cystoscopy of up to €47,790 over a nine-month period. The nurse-led format and non-endoscopic system will also produce other tangible benefits in the form of decreased waiting times and increased resources allocated to diagnostic cystoscopy.
This study is limited by its relatively low power and the retrospective nature of the analysis. However, the questionnaire data were collected prospectively, with a high questionnaire response rate (67%) and no patients lost to follow-up. This is the first study to date reporting on outcomes from a nurse-led stent removal clinic using a magnetic stent and retrieval device.
In conclusion, magnetic tipped stents represent a safe alternative to traditional double J ureteric stents with added benefits clearly illustrated in this study. Stent removal in a nurse-led clinic is effective, well tolerated and acceptable to patients. Magnetic tipped stents are associated with a similar side effect profile to that of traditional indwelling stents. Nurse-led removal frees up valuable resources such as access to diagnostic endoscopy and urologist manpower, with notable potential cost savings.
Compliance with Ethical Standards
There was no conflict of interest regarding any author involved in the study. There was no funding for the study. There were no studies carried out on animals. Informed consent was performed with all participants prior to completion of the questionnaire.
Corresponding author
Ms Lauren O’Connell, Surgical Trainee, James Connolly Memorial Hospital Blanchardstown
Email: [email protected]
Tel: +35316465000
References
1. Finney RP. Experience with new double J ureteral catheter stent. J Urol. 1978;120(6):678-81.
2. Joshi HB, Okeke A, Newns N, Keeley FX, Timoney AG. Characterization of urinary symptoms in patients with ureteral stents. Urology. 2002;59(4):511-6.
3. Leibovici D, Cooper A, Lindner A, Ostrowsky R, Kleinmann J, Velikanov S. Ureteral stents: morbidity and impact on quality of life. Isr Med Assoc J. 2005;7(8):491-4.
4. Kim JH, Park SY, Kim MG, Choi H, Song D, Cho SW. Pain and satisfaction during rigid cystoscopic ureteral stent removal: a preliminary study. BMC urology. 2014;14:90.
5. Macaluso JN, Jr., Deutsch JS, Goodman JR, Appell RA, Prats LJ, Jr., Wahl P. The use of the Magnetip double-J ureteral stent in urological practice. J Urol. 1989;142(3):701-3.
6. Park HK, Paick SH, Kim HG, Lho YS, Bae S. The impact of ureteral stent type on patient symptoms as determined by the ureteral stent symptom questionnaire: a prospective, randomized, controlled study. Journal of endourology. 2015;29(3):367-71.
7. Wang J, Feng J, Hu W, Song Y, Xu X, Fan M. Preclinical evaluation of a newly designed ureteral stent and magnetic retrieval catheter for minimally invasive stent removal. Urology. 2014;84(4):960-6.
8. Joshi HB, Newns N, Stainthorpe A, MacDonagh RP, Keeley FX, Timoney AG. Ureteral stent symptom questionnaire: development and validation of a multidimensional quality of life measure. J Urol. 2003;169(3):1060-4.
9. Scarneciu I, Lupu S, Pricop C, Scarneciu C. Morbidity and impact on quality of life in patients with indwelling ureteral stents: A 10-year clinical experience. Pak J Med Sci. 2015;31(3):522-6.
10. Chew BH, Lange D. Advances in ureteral stent development. Curr Opin Urol. 2016;26(3):277-82.
11. Tolley D. Ureteric stents, far from ideal. Lancet. 2000;356(9233):872-3.
12. Pengfei S, Yutao L, Jie Y, Wuran W, Yi D, Hao Z. The results of ureteral stenting after ureteroscopic lithotripsy for ureteral calculi: a systematic review and meta-analysis. J Urol. 2011;186(5):1904-9.
13. Jeong H, Kwak C, Lee SE. Ureteric stenting after ureteroscopy for ureteric stones: a prospective randomized study assessing symptoms and complications. BJU Int. 2004;93(7):1032-4; discussion 4-5.
14. Giannarini G, Keeley FX, Valent F, Manassero F, Mogorovich A, Autorino R. Predictors of morbidity in patients with indwelling ureteric stents: results of a prospective study using the validated Ureteric Stent Symptoms Questionnaire. BJU Int. 2011;107(4):648-54.
15. Pryor JL, Langley MJ, Jenkins AD. Comparison of symptom characteristics of indwelling ureteral catheters. J Urol. 1991;145(4):719-22.
16. Staubli SE, Mordasini L, Engeler DS, Sauter R, Schmid HP, Abt D. Economic Aspects of Morbidity Caused by Ureteral Stents. Urol Int. 2016;97(1):91-7.
17. Barnes KT, Bing MT, Tracy CR. Do ureteric stent extraction strings affect stent-related quality of life or complications after ureteroscopy for urolithiasis: a prospective randomised control trial. BJU Int. 2014;113(4):605-9.
18. Kim DJ, Son JH, Jang SH, Lee JW, Cho DS, Lim CH. Rethinking of ureteral stent removal using an extraction string; what patients feel and what is patients' preference? : a randomized controlled study. BMC Urol. 2015;15:121.
19. Althaus AB, Li K, Pattison E, Eisner B, Pais V, Steinberg P. Rate of dislodgment of ureteral stents when using an extraction string after endoscopic urological surgery. J Urol. 2015;193(6):2011-4
20. Schlick RW, Rettberg N, Planz K. [Trials with a new potentially biodegradable ureteral stent. In vitro results with GX 100-15 LB]. Urologe A. 1999;38(3):242-5.
21. Kawahara T, Ito H, Terao H, Yamagishi T, Ogawa T, Uemura H. Ureteral stent retrieval using the crochet hook technique in females. PLoS One. 2012;7(1):e29292.
22. Sapre N, Bugeja P, Hayes E, Corcoran NM, Costello A, Anderson PD. Nurse-led flexible cystoscopy in Australia: initial experience and early results. BJU Int. 2012;110 Suppl 4:46-50.
23. BlackStar™ © www.Urotech.com
P687