Neonatal Bacteraemia Among 112,360 Live Births
D Huggard, R Drew, N McCallion
Rotunda Hospital, Dublin1, Ireland
Abstract
Our aims were to determine the incidence of bacteraemia in a cohort of neonatal patients over a 14 year period, to describe the organisms involved, and to establish the rates of sepsis with regard to both early onset sepsis (EOS) and late onset sepsis (LOS). Lastly, we investigated the trends of neonatal sepsis, to determine whether changes in clinical practice influenced the rate of blood culture positivity. With regards to EOS, GBS was the predominant pathogen, followed by E.coli, CoNS, and S. aureus . The overall mean EO rate per 1000 live births (LBs) was 1.19. Looking at LOS, S. aureus , CoNS , Enterococcus spp. were the most common bacteria cultured. The mean LOS rate was 1.88 per 1000 live births. The overall rate of EOS remained fairly steady. GBS remains the major pathogen in EOS; however its incidence has remained largely unchanged over time in relation to both EOS and LOS. Conversely the rate of LOS peaked from ’05-’09, mainly due to an increase in Staphylococcus aureus , CoNS and Enterococcus spp. cases, and then improved dramatically in the following years. This was likely due to a change in hospital policies in relation to hand hygiene and intravenous line placement and maintenance.
Introduction
The profile of neonatal sepsis has changed, even over the last 20 years1, improvements in modern medicine have reduced the incidence of neonatal sepsis, but the pathogens responsible for causing early onset sepsis (EOS) and late onset sepsis (LOS) have also changed2. Since the widespread introduction of screening and intrapartum antibiotics, the incidence of EOS due to group B Streptococcus (GBS) has fallen. EOS due to non GBS species has remained largely unchanged3, however. Unlike EOS, LOS tends to affect those infants who are more premature, who have lower birth weights and who have indwelling catheters in situ. According to a recent report, the most prevalent bacterial isolates in LOS overall are coagulase-negative Staphylococci (CoNS) and Gram negative bacilli4. It is worth mentioning, however, that there are geographical variations in the rates of sepsis4. It stands to reason that centres may differ in NICU design, patient population, patient management and protocols, all of which may impact on the incidence of neonatal sepsis. Surveillance of neonatal sepsis is critical so we can detect trends in both incidence and pathogenicity, and provide data to guide policy development to reduce the incidence of neonatal sepsis, and to establish whether new approaches to prevention are efficacious.
The primary aim of this study was to determine the incidence of bacteraemia in a very large cohort of neonatal patients over a 14 year period from 2001-2014 in a tertiary neonatal unit. The secondary aim was to describe the organisms involved (e.g. E.coli, Group B Streptococcus) and also to establish the rates of sepsis per 1000 live births with regard to both EOS and LOS. Finally this study aimed to investigate the trends of neonatal sepsis in our centre and to determine whether changes in clinical practice influenced the rate of blood culture positivity.
Methods
This was a retrospective review of the incidence of bacteraemia in the Rotunda Hospital, a tertiary neonatal unit, over a 14 year period (2001-2014 inclusive). Data was obtained from computerised hospital laboratory records. As per CDC guidelines5, and for the purposes of this study, early onset sepsis was defined as culture positivity within the first 7 days of life, and late onset sepsis was bacteraemia after 7 days of life, up until discharge from the neonatal unit. All clinically significant blood cultures were included in this review. If a patient had a single positive blood culture with a pathogenic organism (e.g. E.coli, Klebsiella spp., Group B Streptococcus) they were included in the figures. If the patient had persistent positive blood cultures with the same organism, only the first blood culture per episode was counted. For organisms that could potentially be skin contaminants from the taking of the blood culture (e.g.CoNS, Diptheroids), patients had to have two consecutive positive blood cultures with the same organism within 72 hours to be considered as significant. All data was obtained from the computerised laboratory information system. The cultures were drawn from both term & pre-term neonates, representing infants admitted to both NICU and the postnatal wards in a tertiary centre with over 110,000 live births during the study period.
Results
From 2001–2014 there was a total of 112,361 live births in our unit. With regards to EOS there were 135 cases in total. GBS was the predominant pathogen with 52 (38.5%) isolates over this timeframe, followed by E.coli 19 (14.1%), CoNS 19 (14.1%), and S. aureus 17 (12.6%). Of the 19 cases of EOS due to CoNS, the mean age of the patient when the first culture became positive was 4.9 days. For early-onset Group B Streptococcal bacteraemia, 50 of the 52 children (96%) had positive blood cultures by 2 days of age, with the other two cases presenting at 5 days of age and 6 days of age respectively. All cases of early-onset E.coli bacteraemia presented on the date of birth or the next day. For early-onset S. aureus bacteraemia, four of the 10 cases presented by 2 days of age, and the others presented at 5 days of age (n=3) and six days of age (n=3). These six cases that presented at five and six days of age with S. aureus bacteraemia may not have been related to perinatally acquired sepsis, but due to hospital acquired S. aureus bacteraemia in the postnatal period. The overall mean EO rate per 1000 live births (LBs) over the study period was 1.19. The range was from 0.57 per 1000 live births in 2002 & 2007 to a high of 2.16 in 2008. In general the incidence of EOS has remained fairly static over the 14 year period. The mean EO rate per 1,000 LBs due to GBS alone was 0.46. The range was from 0.00 in 2002 to 0.79 in 2009
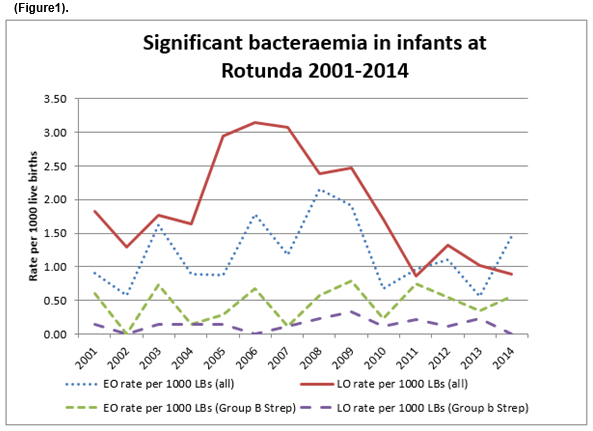
From 2001 to 2014 there were 208 cases of late onset sepsis. The most prevalent bacteria isolated were; S. aureus 56 (26.9%), CoNS 46 (22.1%), Enterococcus spp. 23 (11.1%), E.coli 22 (10.6%), Klebsiella spp. 22 (10.6%) and GBS 16 (7.7%). The mean LOS rate over 14 years was 1.88 per 1000 live births. The range was from 0.86 in 2011 to a high of 3.14 in 2006. As shown in figure 1 the rate of LOS increased significantly from 2005 – 2009 to around 3 per 1000 LBs, however it then drops to around 1 per 1000 from 2010 – 2014. The mean rate of GBS late onset sepsis per 1000 LBs was 0.13. The range was from 0.00 in several years (’02, ’06,’14) to 0.34 in 2009. As is demonstrated in the figure, the incidence has remained low and largely unchanged over the study period.
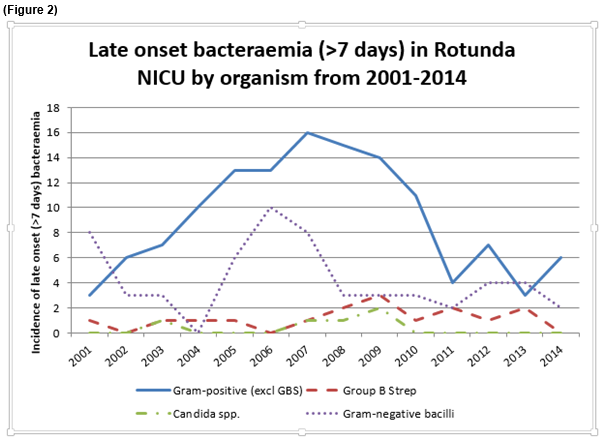
The aetiologies and rate of LOS were examined further in Figure 2. We found that when GBS is excluded, Gram positive organisms were responsible for the vast majority of LOS bacteraemia, 128 cases. This reflects the predominance of S. aureus and CoNS in causing culture positivity in LOS, often related to indwelling venous catheters. As is discussed above there is a peak of cases from 2005-2009 (13-16 cases), and a dramatic decrease from 2011- 2014 (3-7 cases). Gram negative bacilli (GNB) were another significant group of microorganisms responsible for LOS. There were 59 positive cultures in total, with a range of 0 in 2004, to 10 in 2006. This is representative of sepsis mainly due to Klebsiella spp., E. coli and Enterobacter spp. often secondary to necrotizing enterocolitis. From 2005 – 2007 there was a spike in the rate of GNB sepsis, with 6 cases in 2005, 10 cases 2006, and 8 cases 2007. There has been a reduction in LOS due to GNB since then with an average of 2-4 cases per year. LOS due to candida was found to be low, with 5 cases in total. As discussed above the rate of LOS due to GBS has remained static over time, with 16 cases in total, averaging 1 to 3 cases per year.
Discussion
A study in the U.S. showed that the overall incidence of EOS due to GBS has decreased over the years since screening & intrapartum antibiotics; to an incidence of 1.59 cases per 1,000 live births6. We have demonstrated that over 14 years in our centre GBS remains the predominant pathogen in EOS, with a mean rate per 1000 LBs of 0.46. Our figures demonstrate a cyclical pattern of EO GBS culture positivity occurring approximately every 3 years, but overall there has been no real change in this rate over this time (Figure 1). Likewise the rate of EOS from all microorganisms has also remained fairly static, with a mean rate per 1000 LBs of 1.19. Of note throughout the study period there were no cases of Listeria detected.
Conversely with LOS there was a significant decrease in the rate of LOS due to all causes. In our population LOS was mainly due to S. aureus , CoNS, Enterococci, followed by GNB such as E.coli and Klebsiella spp. It is well recognised that LOS attributable coagulase-negative Staphylococci and Staphylococcus aureus is associated with significant morbidity and mortality3. As seen in figure 1, there was a spike in the rate of LOS from 2005- 2009, peaking at 3 per 1000 LBs, this rate is seen to then drop off to a rate of approximately 1 per 1000 from 2011- 2014. The increased incidence of LOS from 2005-2009 may be have been due to a couple of significant factors. In common with many other units, the NICU at the Rotunda has experienced increased case numbers and acuity at the same time as experiencing challenges with staffing the unit, and meeting with nursing to patient ratios in particular. These factors may account for some of the increase in LOS rates found in recent times. This observed improvement in LOS bacteraemia coincided with several steps taken by the unit to improve the rate of nosocomial infection. Firstly, the Neonatal Infection Prevention and Control Group (NIPCG) implemented training and education in hand hygiene and undertook regular hand hygiene audits. A dedicated PICC Team of Non-Consultant Hospital Doctors (NCHDs) and Advanced Nurse Practitioners evaluated practice and made changes relating to skin asepsis. Peripheral and PICC vascular catheter maintenance was regularly assessed, and any indwelling catheters no longer required were promptly removed. Similarly a paper looking at reducing the rate of central line associated infections in NICUs found that a collaborative structure targeting team development, family partnership, unique bundle elements and strict reporting on line care produced a large reduction in infection rates7. The relatively simple changes we have implemented made a huge difference to our LOS rates as well as significantly reducing our costs associated with nosocomial infections.
It has been established that Gram negative bacteria such as Klebsiella spp., E. coli and Enterobacter spp.remain responsible for significant morbidity and mortality, especially in very low birth weight infants8. Indeed one paper stated that GNB account for 20% of episodes of LOS among VLBW infants9. Our data shows that 28% of LOS is due to GNB, which is often secondary to necrotizing enterocolitis, however fluctuations in GNB LOS rates were not matched by variations in the incidence of NEC in this cohort.
On further inspection of the aetiologies of LOS, it was found that there was a rise in GNB culture positivity in ’05, ‘06’, 07 with 6, 10 and 8 cases respectively per annum. This is a rise from 0-3 cases p.a in the preceding years. This spike is mainly related to a rise in Klebsiella spp., there were 10 cases (6 in ’06) during these years. There were no outbreaks of Klebsiella during this period, although the hospital was monitoring the number of cultures positive for same carefully. Otherwise, Enterobacter spp. (5 cases), and 7 cases of E.coli were the other significant pathogens detected in this timeframe. However, after 2007 and up to 2014 we see a drop in the incidence of GNB positivity to a mean of 3 cases per year. On reviewing our figures, this fall in GNB culture positivity has not been shown to be related our incidence of NEC during these years. With regards to candida, there has been no change in antifungal prophylaxis practice, as the candida LOS rates remain extremely low on the unit.
We have demonstrated that over 14 years and 112,000 live births that the overall rate of EOS remained fairly steady. In our institution, we follow the RCOG guidelines and don’t do routine antenatal screening for GBS on our patients. GBS remains the major pathogen in EOS; however its incidence has remained largely unchanged over time in relation to both EOS and LOS. Conversely, the rate of LOS peaked from ’05-’09, mainly due to an increase in S. aureus , CoNS and Enterococcus spp. cases, and then improved dramatically in the following years. This was likely due to a change in hospital policies in relation to hand hygiene and intravenous line placement and maintenance.
Despite the advance in neonatal medicine over the past decades, the burden of neonatal sepsis remains high as it is associated with increased morbidity, mortality and poorer neurodevelopmental outcomes10. Improvement in neonatal sepsis rates must be a priority in the NICU. Although we successfully reduced neonatal bacteraemia rates with certain microorganisms in LOS, we did not show any reduction in the incidence of GBS sepsis over time. Minimizing the incidence of culture positive GBS sepsis should now be a priority. The much heralded advent of a GBS vaccine may play a key role in achieving this reduction.
Conflict of Interest:
The authors have no conflicts of interest to declare.
Correspondence
Dean Huggard, Rotunda Hospital, Dublin1, Ireland
Email: [email protected]
References
1. Philip AG, The changing face of neonatal infection: experience at a regional medical centre. Pediatric Infectious Disease Journal. 1994 13:1098-1102
2. Bizzarro MJ1, Raskind C, Baltimore RS, Gallagher PG. Seventy-five years of neonatal sepsis at Yale: 128-2003. Pediatrics. 2005 Sep;116:595-602.
3. Shane AL1, Stoll BJ. Recent developments and current issues in the epidemiology, diagnosis, and management of bacterial and fungal neonatal sepsis. Am J Perinatol. 2013 Feb;30:131-41.
4. Dong Y, Speer CP. Late-onset neonatal sepsis: recent developments. Arch Dis Child Fetal Neonatal Ed. 2015 May;100.
5. Centres for Disease Control and Prevention. www.cdc.gov/groupbstrep/about/newborns
6. Puopolo KM, Eichenwald EC. No change in the incidence of ampicillin-resistant, neonatal, early-onset sepsis over 18 years. Pediatrics. 2010 May;125.
7. Fisher D1, Cochran KM, Provost LP, Patterson J, Bristol T, Metzguer K, Smith B, Testoni D, McCaffrey MJ. Reducing central line-associated bloodstream infections in North Carolina NICUs. Pediatrics. 2013 Dec;132.
8. Cordero L1, Rau R, Taylor D, Ayers LW. Entericgram-negative bacilli bloodstream infections: 17 years' experience in a neonatal intensive care unit. Am J Infect Control.2004 Jun;32:189-95.
9. Smith A1, Saiman L, Zhou J, Della-Latta P, Jia H, Graham PL 3rd. Concordance of Gastrointestinal Tract Colonization and Subsequent Bloodstream Infections WithGram-negativeBacilli in Very Low Birth Weight Infants in the Neonatal Intensive Care Unit. Pediatr Infect Dis J. 2010 Sep;29:831-5.
10. Mitha A1, Foix-L'Hélias L, Arnaud C, Marret S, Vieux R, Aujard Y, Thiriez G, Larroque B, Cambonie G, Burguet A, Boileau P, Rozé JC, Kaminski M, Truffert P, Ancel PY; EPIPAGE Study Group. Neonatal infection and 5-year neurodevelopmental outcome of very preterm infants. Pediatrics. 2013 Aug;132:e372-80.
P467