Opportunity Costs in Paediatric Training: The Specialist Registrars Experience.
MB O’Neill, T Nabialek, N Kandamany
Dept. of Paediatrics, Mayo University Hospital, Castlebar, Co Mayo
Abstract
In the training process, there is a tension between the work life and home life of trainees. This study explored both the personal impact and the opportunity costs of training from the Specialist Paediatric Registrar (SPR) perspective. The survey explored 1) career progression2) perceived functional effectiveness at work 3) psychological impact of hospital based training and 4) the personal and social cost of training. Fifty-three (71%) SPRs responded of whom 47 (89%)were married or in long term relationships. Seventy-five percent of trainees had a definite career plan with 86% intending to undertake fellowship training. Seventy percent believed they were efficient time managers but 53% had difficulty in making time for academic pursuits and fifty percent experienced negative feelings, which lingered after work and interfered with their relationships at home. Seventy-four percent stated training was undertaken at significant personal cost with only 21% achieving a very satisfactory work/life balance. To address these difficulties trainee wellbeing should be addressed at the Basic Specialist Training (BST) level and the career path clearly explained outlining the challenges that are likely to be encountered.
Introduction
Entry into the Higher Specialist Training (HST) in Paediatrics is by competitive interview after satisfactory completion of the Basic Specialist Training (BST) programme. On successful completion of training candidates are eligible to apply for consultant paediatric posts, however there is currently no matching of training numbers to the availability of consultant paediatric posts. Trainee career decisions are influenced by lifestyle choices1 and while satisfaction with the HST in paediatrics is high2 there is an ongoing tension to achieve an appropriate work/life balance. This study explored both the personal impact and the opportunity costs of HST in Paediatrics
Methods
A mixed model questionnaire was utilised to survey SPRs, by email, utilising the Royal College of Physicians (RCPI) database. The survey was developed by the authors (MO’N and NK) and tested for internal validity by piloting it in a group of 4 SPRS. Demographic data obtained included sex and relational status inclusive of the number of children. The survey explored, from the SPR perspective a) career progression b) perceived functional effectiveness at work c) psychological impact of hospital-based paediatrics and d) the personal and social costs of a career in paediatrics. The questionnaire utilised three strategies to obtain the data which included 1: a Likert scoring system; cuing at 1, not at all and cuing at 6, extremely, 2: questions that allowed for a narrative response and 3: binary questions with a Yes/No answer. An unsure option was allowed in the binary questions to prevent inappropriate skewing of results. Ethical approval was obtained from the research committee at Mayo University Hospital. The survey was conducted in March 2011 when 75 trainees were enrolled in the program.
Results
Fifty-three (71%) SPRs responded. The male-female ratio was 1 to 1.9. Forty-seven (89%) were married or in long-term relationships and 18 (34%) had children. The response rate by year was year 1,10(66%), year 2, 11(73%), year 3, 10(66%), year 4, 9(60%), and year 5, 13(87%).
Career progression
Forty (75.5%) SPRs had a definite career plan with 30 (56.6%) believing that they should organise their higher degree and further training. Forty-six (86.8%) SPRs were engaged in or intended to undertake fellowship training with 34 (64.2%) pursuing an MD degree,16 (31.1%) a Masters, 4 (7.5%) a PhD degree and 11 (20.8%) a diploma. The mean Likert score career progressing as envisaged was 3.8, with a positively skewed Likert score (Likert 5 to 6 score) in 18 (34.6%).
Functional effectiveness at work
Thirty-nine (71.7%) SPRs believed that they were efficient time managers with 45 (84.9%) undertaking a self-analysis of performance and 53 (100%) undertaking clinical reflection. Forty-six (86.8%) indicated an ability to self-initiate and 35(67.8%) had considered methods to improve their efficiency at work. The most challenging aspects of SPR training were 1: making time for research and academic pursuits cited by 28 (53%), 2: relocating to centres outside Dublin cited by 8 (15%) and 3: uncertainty relating to consultant post availability cited by 7 (13.2%). Solutions to these challenges included 1: enshrining protected teaching time was cited by13 (24.5%), 2: increasing the numbers of non-consultant hospital doctor (NCHD) numbers cited by 9 (17%), 3: improved matching and tailoring of schemes to individual preferences cited by 7(13.2%) and 4) decreasing the service component of SPR posts cited by 2(3.7%).
The mean Likert score for the beneficial nature of end of year assessments was 2.8, with a positively-skewed Likert (5 to 6) score cited by 5 (9.3%) trainees. The mean Likert score for the utility of the portfolio was 3.3 with a positively skewed Likert score cited by 8 (18.1%).
Impact of hospital-based paediatrics
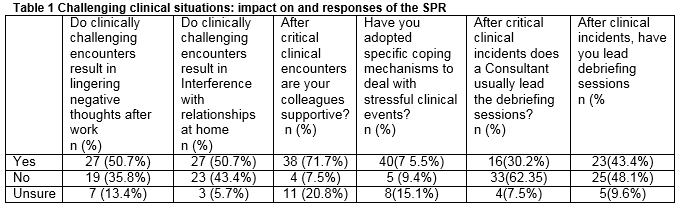
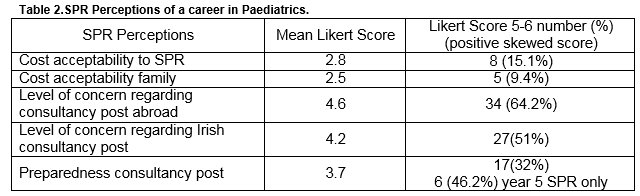
The impact of challenging situations both clinical and non-clinical in the work environment are outlined in Table 1. The preferred coping strategies, utilised by SPRs included exercise for 23(43.4%), discussions with supportive individuals for 19 (35.8%) and socialising for 11 (20.8%). The mean Likert score for an appropriate work/life balance was 3.3 with a positive Likert score cited by 11(21. 1%). The career perceptions of the SPRS are outlined in Table 2.
The impact of a career in paediatrics
Thirty-nine (73.6%) trainees felt they had incurred significant personal costs in pursuing a career in paediatrics, with 26 (49.1%) compromising their personal or family time and 15 (28.3%) having borne significant financial or emotional burden from relocating. Five (14.2%) female trainees deferred having children to pursue their career. The mean Likert score, inclusive of the number and percentage of positively skewed Likert scores for the achievement of work/life balance, were 3.3 and 11 (21.1%) respectively.
Discussion
This qualitative study was undertaken to assess the perception and the impact of training from the SPR’s perspective. While doctors are more familiar with quantitative research, qualitative research allows for the exploration of perceptions and personal impacts of training, which must be undertaken to enhance the training process. The high response rate, with an equal spread over all years of training, suggests the results are generalizable. The results however, are both positive and negative. Three-quarters of SPRs are content and have a definite career plan which is progressing very satisfactorily for 34.6%. This compares favourably with 13% for non SPRs3. One-third (30.2%) of SPRs feel that the expectations placed on them are very realistic, but despite this low percentage, the attrition rate from the HST programme is very low. SPRs indicate that they are effective at work with over 80% undertaking an analysis of performance, clinical reflection and having an ability to self-initiate. However, we are unable to quantify these perceptions. Despite these positive findings, over half (53.3%) of the SPRs have difficulty in making time for clinical research and academic pursuits. One-quarter cite the lack of protected time as a core issue despite it being an integral part of the SPR contract, but this percentage is reduced from 37% cited in a 2005 study of SPRs2 indicating that progress is being made. The introduction of the European Working Time Directive (EWTD) should allow all SPRs to have planned half day releases.
The strong focus on clinical research and academic pursuits may hide a flaw in the current training curriculum. In Canada, the Royal College of Physicians and Surgeons has developed the CanMEDs (Canadian Medical Education Directives for specialties)4 programme which is an educational framework that describes the abilities physicians require to effectively meet the healthcare needs of the people they serve. It outlines the competencies that a trainee must achieve in their role as medical expert, communicator, collaborator, manager, advocate, scholar, and professional. Such a curriculum modification would focus the SPRs training goals and objectives, and may help alter the negative views that they express relating to the end-of-year assessments and their portfolio, and would also provide a focus for their half-day a week protected time. It could also serve as a template for their study days5.
The emotional impact of challenging cases in the hospital environment is difficult to quantify, but this survey indicates that it transfers to the home life of SPRs with 50% indicating they reflect on cases at home and similar number indicating interference with relationships. Studies indicate that HST training is challenging and the stress experienced by trainees is significant, with the odds ratio for burnout increasing from 1 for medical students to 1.38 (95% CI, 1.2 – 1.58) for residents and fellows in training. However it decreases to 1.10(95% CI, 0.90 -1.34) after training is complete6. The preferred coping mechanisms which include exercise (43.4%), discussion with supportive individuals (35.8%) and socialising (20. 8%), do not address the core issue of the stress that the experience. The development of resilience training should be undertaken by all trainees prior to the entry onto the SPR programme. However the impact of these interventions is modest7, with a pooled Standard mean difference of 0.37 (95% CI,0.18-0.57). Trainee wellbeing should commence at the BST level and be incorporated into all levels of training.
The number of SPRs citing positive skewed Likert score for satisfaction with work /life balance was 11(21%), with 26(49.1%) experiencing significant compromise of both personal and family lives which is reflective of the tension that occurs between the training process and the trainee’s home life. This cost was very acceptable for only 8 (15.1%) of SPRS and for 5(9.4%) of their partners. Thirty-four (64.2%) SPRs were very concerned that consultant posts would not be available for them after training, and 17 (32.1%) felt that they would be very well-trained for these posts. This figure compares favourably with 34.7% Canadian and American graduates who felt they were very well-trained and prepared for consultancy8. These negative impressions relating to career prospects can be countered, to some degree, through structured dissemination of information and counselling with regard to career planning during the training process9. However, the absence of the defined manpower plan for paediatrics in Ireland will exacerbate these negative perceptions.
This qualitative study has several limitations, given that it relied on SPRs self-reports and consequently is subject to bias. Incorporating a psychologist-lead interview of senior SPRs, at the end of year assessments, could provide more useful information on the trainees’ experience and help to both clarify and elaborate the themes explored in this study. Some SPRs may have perceived this study as voyeuristic, given the personal nature of the themes explored. However the high response rate suggests an active interest in the themes explored. To our knowledge, no other Irish training programme has undertaken a study similar to this one and consequently, comparison to other trainees cannot be inferred. The training process for consultants has always required a degree of sacrifice. However it would appear prudent to modify this process, where possible, to ensure trainees have an appropriate work/life balance while maintaining high training standards 10.
Conflict of Interest
The authors state that they have no conflict of interests.
Correspondence: Dr Michael O’Neill, Dept. of Paediatrics, Mayo University Hospital, Castlebar, Co. Mayo
Mobile number 087 8046896
Email: [email protected]
References
1)Freed GL, Dunham KM Douglas Jones M, McGuinness GA, Althouse L and research committee of the American board of paediatrics. General paediatrics resident perspectives on training decisions and career choice. Paediatrics 2009; 123: S 26 – S 30
2)Byrne OC, Boland B, Nicholson AJ, Waldron M, O’Neill MB. Training and manpower issues for specialist registrar in paediatrics. How are we doing and where are we going? Ir Med J. 2005; 98 (1): 13-15
3) O’Neill MB, Kumar A. The non-specialist paediatric registrar in the healthcare systema.Ir Med J. 2012; 105 (7): 247-249
4) Frank JR, Snell L, Sherbino J, editors. CanMEDS 2015 Physician Competency Framework. Ottawa: Royal College of Physicians and Surgeons of Canada; 2015.
5)DiGenova TD, Valentino PL, Gosselin R, Bhanji. The academic half-day redesigned: Improved generalism, promoting CanMEDS and developing self-directed learners. Paediatric child health. 2015; 1:30 – 34
6) Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J,Shanafelt TD. Burnout among US medical students, residents, and early career physicians relative to the general US population. Acad med. 2014; 89:443 – 451
7) Leppin Al, Bora PR, Tilburt JC, Gionfriddo MR, Zeballos -Palacios C, Dulohery MM,Sood A, Erwin PJ, Brito JP ,Boehmer KR, Montori VM. The efficacy of resiliency training programs: a systematic review and meta-analysis of randomised trials.PloS One. 2014, 27; 9: e111420
8)Lieberman L, Hilliard RI. How well do paediatric residency programs prepare residents for clinical practice and their future careers? Medical education 2006 40:539 – 546
9)Garci RL, Windish DM, Rosenbaum JE Resident career planning in internal medicine: A qualitative assessment.J Grad Med Educ.2010 Dec 518-522
10) Dornhorst A, Cripps J, Goodyear H, Marshall J, Waters E, Boddy SA on the half of the working lives intercollegiate committee. Improving hospital doctors working lives: online questionnaire survey of all grades. Postgrad med J 2005; 81:49- 54
(P602)