Portal Hypertensive Colopathy with Pelvic Varices presenting as Severe Lower GI Bleed treated with TIPSS
SF Murphy, M Durand, JP McMorrow, JF Meaney, M Guiney
Department of Radiology, St James’s Hospital, Dublin 8
Abstract
We present the case of a 71-year-old lady with a background of significant alcohol intake who presented with frank lower gastrointestinal (GI) bleeding, lower abdominal pain and haemoglobin 6.3g/dL. CT abdominal angiogram showed right-sided colonic thickening, atrophic liver and enlarged superior mesenteric vein (SMV) and right-sided pelvic varix. This lead to a diagnosis of portal hypertensive colopathy secondary to alcoholic liver cirrhosis. The patient failed conservative management and underwent a Transjugular Intrahepatic Portosystemic Shunt (TIPSS) procedure. This lead to an immediate resolution of her lower-GI bleeding. Repeat CT at three weeks showed a decompressed SMV and resolution of the right-sided pelvic varix. The patient was discharged after three months following optimization of medical condition and social circumstances.
Introduction
Cirrhotic liver disease is an important cause of upper-GI bleeding but is less recognised in lower-GI bleeding1. Portal hypertensive colopathy (PHC) refers to colorectal mucosal lesions in patients with portal hypertension2. It commonly presents surreptitiously with iron deficiency anaemia, but rarely, can also manifest as acute severe lower-GI bleed3. We present a case of acute severe GI bleeding secondary to PHC from our institution.
Case
We present the case of a 71-year-old lady who presented with a 48-hour history of frank lower-GI bleeding and diffuse lower abdominal pain. The patient had a history of alcohol dependence and no previous GI bleeding. On examination the patient was in Grade II shock (pulse 115bpm, BP 140/70mmHg), abdomen was soft, non-tender and there was fresh blood with clots on rectal examination. The patient had a Hb 6.3g/dL(11.5-16.5), platelets 130x109/L(150-400), bilirubin 27umol/L(0-21), INR 1.7, ALP 93iu/L(35-104), GGT 157iu/L(6-42), AST 45iu/L(0-32), ALT 15iu/L(0-33), albumin 31g/L(35-50) and Childs-Pugh score was 8. Initial management included 2g fibrinogen and fresh frozen plasma, IV fluids, 2 units red cell concentrate (RCC), IV co-amoxiclav, IV omeprazole and high dependency unit (HDU) admission under the colorectal surgical team.
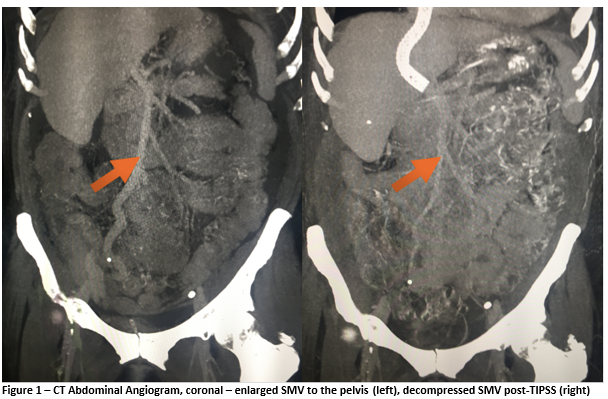
CT abdominal angiogram on day 1 (Figures 1 and 2) showed right-sided colonic thickening, high-attenuation material within the caecum suggestive of intra-luminal blood with no active bleeding vessel identified. An atrophic liver and moderate ascites and an enlarged superior mesenteric vein with portosystemic variceal shunting in the right hemipelvis with the gonadal vein were noted. There was no splenomegaly, oesophageal varices or other portosystemic shunts. Colonoscopy showed a significant volume of intraluminal blood but poor visibility made it difficult to identify any mucosal abnormalities. This lead to a working diagnosis of portal hypertensive colopathy secondary to chronic alcoholic liver disease.
The patient was monitored in HDU over the following two days given the lack of active bleeding on CT and commenced on propranolol. PR bleeding persisted, with another three units RCC required. Repeat CT on day three was unchanged, showing high-attenuation material within the lumen of the colon suggestive of blood but no active bleeding point identified. It was decided to proceed with a TIPSS procedure on day three. The hepatic venous pressure gradient dropped from 13 to 4mmHg post-procedure. The patient returned to HDU, had no further bleeding and Hb stabilized at 8.5g/dL. She developed mild hepatic encephalopathy which self-resolved. Repeat CT on day 16 (Figures 1 and 2) showed markedly reduced calibre SMV, resolution of the pelvic varix and no intra-luminal blood. She returned to the ward and was discharged after three months following optimization of medical and social circumstances. She has been followed-up as an outpatient for two years, having no further episodes of bleeding.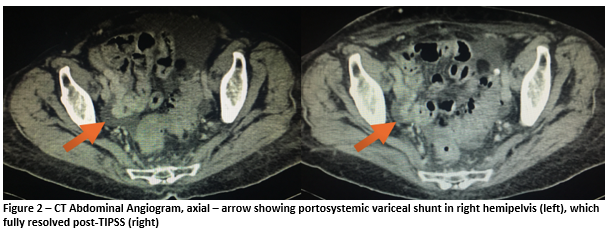
Discussion
PHC is underrepresented in the literature and there are no formal guidelines on its management. The bleeding risk from PHC has been reported as up to 8% of cases4. The use of TIPSS, first described in 1969 by Rosch et al., has previously been recommended for control of acute or recurrent oesophageal or gastric variceal bleeding unresponsive to endoscopic and pharmacological treatment5. TIPSS has been used in PHC previously but no reports describe a pelvic shunt as seen in our case6. In a case of a 75-year-old lady with a diagnosis of liver cirrhosis secondary to hepatitis B, TIPSS was used for recurrent bleeding secondary to PHC refractory to propranolol7. In conclusion, this represents a rare case of life-threatening haemorrhage from PHC secondary to cirrhotic liver disease treated with TIPSS. The imaging findings are impressive and demonstrate a grossly dilated SMV and a large varix in the right hemipelvis, both of which resolved following decompression of the portal venous system.
Conflict of interest statement:
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Correspondence:
Stephen F Murphy
Department of Radiology, St James’s Hospital, Dublin 8
Email: [email protected]
References
1. Kalafateli M, Triantos CK, Nikolopoulou V, Burroughs A. Non-variceal Gastrointestinal Bleeding in Patients with Liver Cirrhosis : A Review. 2012;2743–54.
2. Kozarek RA, Botoman VA, Patterson DJ, Ball TJ, Bredfeldt JE, Roach JM. Portal Colopathy : Prospective Study of Colonoscopy in Patients With Portal Hypertension. 1991;1192–7.
3. Yoshie K, Fujita Y, Moriya A, Kawana I, Miyamoto K, Umemura S. Octreotide for severe acute bleeding from portal hypertensive colopathy: a case report. Eur J Gastroenterol Hepatol. 2001;13(9):1111–3.
4. Ganguly S, Bhatia V. The Prevalence and Spectrum of Colonic Lesions in Patients With Cirrhotic and Noncirrhotic Portal Hypertension. Hepatology. 1995;21(5):1226–31.
5. Tralka SUE. Special Article The Role of Transjugular Intrahepatic Portosystemic Shunt for Treatment of Portal Hypertension and Its Complications : A Conference Sponsored by the National Digestive Diseases Advisory Board. Hepatology. 1994;22(5):1591–7.
6. Malki S, Allen R, Pavli P. Transjugular intrahepatic portosystemic shunt for intractable colonic bleeding in a patient with cirrhosis. J Gastroenterol Hepatol. 2000;15(January):962–3.
7. Balzer C, Lotterer E, Kleber G, Fleig WE. Transjugular Intrahepatic Portosystemic Shunt for Bleeding. Gastroenterology. 1998;115(1):167–72.
(P696)