The Case for Shared Medical and Psychiatric Units: Are They Needed and How They Could Run?
R.M Duffy1, M. Sadlier1, A.H. Van Der Ploeg2, J. Sheehan1
- Department of Liaison Psychiatry and UCD School of Medicine and Medical Science, Mater Misericordiae University Hospital, Ireland
- Academic Centre of Psychiatry, University of Groningen, Hanzeplein 1, 973 GZ Groningen, The Netherlands
Introduction
A diagnosis of major mental illness is associated with a 15-20 year reduction in life expectancy1. Individuals with mental illness face many difficulties accessing and receiving healthcare, many of these barriers exist in secondary care. On medical and surgical wards, the majority of mental healthcare is delivered by consultation liaison services. Hospital based psychiatry is increasingly important; well designed services are often cost-effective and can reduce patient’s length of stay2. Some individual’s care needs, however, exceed the capacity of such a service. There is a significant unmet need for individuals with severe co-morbid mental and physical illness, due to their increased lengths of stay, costs and readmission rate3. In these cases ‘both medical and psychiatric safety features form a prerequisite for the physical settings’ 4. This paper examines the need for shared care units (SCU), with additional mental health input.
A Vision for Change proposes one adult liaison mental health services for 300,000 people and a national 6-10 bed neuropsychiatry unit5. While the proposed neuropsychiatry unit does not currently exist it would only address a small proportion of the individuals who could benefit from a SCU.
In Ireland there are currently just over 10,000 acute inpatient beds6. Overall 52.5 people per 100,000 require inpatients mental health services7. Based on these numbers there is a need for 5 inpatient beds nationally where medical and psychiatric needs can be addressed simultaneously. This calculation however falsely assumes no association between physical and mental health morbidity. In reality a bidirectional association is well established. Psychological morbidity is higher in medical inpatients. A study of general medical and trauma orthopedic admissions, showed that 64% of those over 70 had significant psychiatric morbidity including 8% with delusions and 6% with hallucinations8. Patients with major mental illnesses have increased levels of mortality9, even in highly income countries greatly reduced life expentancy1. Kishi and Kanthol suggest that one percent of patients admitted to general hospital would benefit from a SCU4. Compounding this association between physical and psychological illness is the fact that Ireland’s population is aging, older patients have higher rates of inpatient care for both physical and mental health reasons7.
A review of four studies of such wards demonstrated that SCUs reduce psychiatric symptoms, shorten in length of stay, improve functional outcomes and a decrease the need for long-term care10. A medical and mental health unit for older individuals with delirium and dementia has been trialed in the UK with initially favorable and cost effective results11.
We identify three cohorts of patients who may benefit from this service. The interventions such a ward could deliver are examined and some of the potential practical considerations are discussed. Key potential benefits that this shared model could provide are highlighted.
Cohorts that would benefit from a SCU
Individuals with mental illness often experience misdiagnosis and delays in treatment. Shefer et al identified three key factors which lead to these negative outcomes: behaviours that challenge, poor communication and diagnostic complexity12. Noblett et al surveyed liaison psychiatrists and identified their main concerns, these were: “diagnostic overshadowing”, poor communication with the patient, failure to respect dignity and delays in receiving investigation and treatment13. One of the main contributing factors noted by Noblett et al was the level of diagnostic complexity. This complexity can be greatly increased when the role of medically unexplained symptoms is a potential factor. Medically unexplained symptoms are common in secondary care and in some outpatient clinics they make up the majority of cases. The impact of such symptoms is significant and results in disability, reduced quality of life and large costs to the health service14. In the UK their investigation and treatment takes up 10% of the NHS budget for individuals of working age.
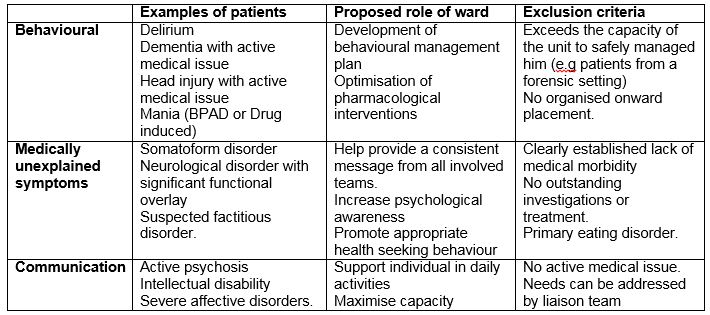
The results of these studies, which highlight the challenges and limitation of mental health care provision in a secondary care setting, have helped identify three cohorts of patients who would benefit from a SCU. Firstly, individuals who present with behaviours that challenge, secondly, individuals that present with severe communication difficulties and, thirdly, individuals with medically unexplained symptoms. These are summarised in table 1.
Tables 1
Proposed admission groups (based on Noblett et al and Shefer et al).
Individuals may present with behaviours that challenge for a variety of reasons, these include organic illness (such as dementia, delirium or head injury), mental health problems (such as psychosis or mania), intellectual disability and autism. Where an acute medical issue is present a SCU may provide the appropriate therapeutic environment for the delivery of necessary medical care.
Individuals with communication difficulties may present with similar diagnoses but without the same level of challenging behaviour. Individuals with very severe psychosis or affective illness or individuals with severe obsessive compulsive disorder who find hospitals unmanageable may also be considered for admission. Where the communication difficulty does not relate to a mental health problem, speech and language input would be the appropriate course of action. Individuals requiring admission to a SCU for communication problems would be those requiring higher levels of support with daily activities that cannot usually be provided on a medical or surgical ward.
Cases with pure, well established somatoform or functional disorders should be treated outside of a medical setting, however, for many individuals the diagnosis remains uncertain or a degree of functional overlay is thought to contribute to the diagnostic picture. Messages from different teams about diagnosis and future investigations may vary and this can greatly compound an individual’s distress and uncertainty. A SCU may provide the appropriate environment for further investigation and treatment.
For all patients, once either the physical or psychological issues has been addressed, the individual would be transferred from the SCU to the appropriate ward to address the remaining issues. While there could be substantial overlap between our proposed SCU and an inpatients service for individuals with eating disorders, individuals with eating disorders should be managed in a specialised unit designed specifically for their needs.
The interventions of a SCU
We would propose that a shared care ward would build on the interventions already proven by Tanajewski et al in an older population11. This would include the five following steps. Firstly, employing mental health staff (nurses, occupational therapists, physiotherapists), to work alongside acute hospital staff in the SCU. This would provide individuals with health professionals trained to meet their mental health needs and create a safe ward environment. This will lessen the perception among general nurses that they are working outside of their field of specialisation. Such interventions would also help maximise the capacity of individuals on the ward to support them in getting appropriate, timely treatment for their medical conditions. Secondly, all staff on the SCU would receive training in the management of individuals with mental health problems. This would equip all staff to be aware of the mental health needs of patients and to identify signs of decline in mental health or the emergence of risk issues. Thirdly, organized therapeutic interventions could be delivered on the ward. These could include occupational therapy groups, mindfulness classes, and psychological interventions. Fourthly, the ward environment would be adapted to maximize psychological well being, and minimize stress and risk. This could include the provision of individual rooms, the removal of ligature points, clear lines of sight for nursing staff, the provision of group rooms and appropriately furnished interview rooms. Finally, a proactive approach to involving family in treatment and recovery would be promoted on the ward.
Discussion
Individuals with severe mental illness are not being well served in general hospitals, their life expectancy is much lower than that of individuals without major mental illness. Steps need to be identified and taken that can promote the physical health of those with mental illness.
Staff working outside of their field of expertise are in an uncomfortable position. Ross and Goldner have examined how this lack of training, lack of resources to provide safe care and the perceived fragmentation of care can all result in nursing staff stigmatising individuals with mental health problems on medical wards15. A SCU would provide a setting to address the needs of the most challenging general hospital patents in an accepting and therapeutic environment.
Many pragmatic issues would need to be addressed in the running of such a ward. These would include level of medical care that could be provided, precise admission and discharge criteria and funding for such a unit. A potential issue in the shared care model is where clinical responsibility lies; this issue is not new to liaison psychiatry and has been identified as an issue in emergency departments12.
Conclusion
Ireland has a need for a SCU. Current practices are likely contributing to major delays in investigation and treatment. The majority of psychiatry input for medical and surgical patients can occur through a consult liaison service. However, groups of patients exist who simultaneously require a high level of medical or surgical input alongside psychiatric care. Consult liaison psychiatry is unable to meet this need in its present form. Consequently SCUs should be a standard part of model 4 hospitals, their role should be carefully considered and additional research may help quantify their need.
Conflict of Interest
The Authors have no conflict of interests
Correspondence:
Richard Duffy
[email protected]
0857362332
References
1. Wahlbeck K, Westman J, Nordentoft M, Gissler M, Laursen TM. Outcomes of Nordic mental health systems: life expectancy of patients with mental disorders. Br J Psychiatry. 2011, 199(6):453-8.
2. Wood R, Wand AP. The effectiveness of consultation-liaison psychiatry in the general hospital setting: a systematic review. J Psychosom Res. 2014, 76(3):175-92.
3. Jansen L, van Schijndel M, van Waarde J, van Busschbach J. Health-economic outcomes in hospital patients with medical-psychiatric comorbidity: A systematic review and meta-analysis. PLoS One. 2018, 13(3):e0194029.
4. Kishi Y, Kanthol RG. Integrating Medical and Psychiatric Treatment in an Inpatient Medical Setting, The Type IV Program. Psychosomatics. 1990, 40: 345-355.
5. Department of Health and Children. A vision for change: Report of the expert group on mental health policy. 2006. Government publication office, Dublin.
6. Department of Health. Health in Ireland, Key trends 2016. 2016. Department of Health, Dublin.
7. Daly A and Craig HRB Statistics Series 32 Irish Psychiatric Units and Hospitals Census 2016
8. Goldberg SE, Whittamore KH, Harwood RH, Bradshaw LE, Gladman JR, Jones RG; Medical Crises in Older People Study Group. The prevalence of mental health problems among older adults admitted as an emergency to a general hospital. Age Ageing. 2012, 41(1):80-6.
9. Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 2014, 13(2):153-60.
10. Hussain M, Seitz D. Integrated Models of Care for Medical Inpatients With Psychiatric Disorders: A Systematic Review. Psychosomatics. 2014, 55:315-325
11. Tanajewski L, Franklin M, Gkountouras G, Berdunov V, Harwood RH, Goldberg SE, Bradshaw LE, Gladman JR, Elliott RA. Economic Evaluation of a General Hospital Unit for Older People with Delirium and Dementia (TEAM Randomised Controlled Trial). PLoS One. 2015, 10(12):e0140662.
12. Shefer G, Henderson C, Howard LM, Murray J, Thornicroft G. Diagnostic overshadowing and other challenges involved in the diagnostic process of patients with mental illness who present in emergency departments with physical symptoms--a qualitative study. PLoS One. 2014, 9(11):e111682.
13. Noblett J, Caffrey A, Deb T, Khan A, Lagunes-Cordoba E, Gale-Grant O, Henderson C. Liaison psychiatry professionals' views of general hospital care for patients with mental illness: The care of patients with mental illness in the general hospital setting. J Psychosom Res. 2017, 95:26-32.
14. Bermingham SL, Cohen A, Hague J, Parsonage M. The cost of somatisation among the working-age population in England for the year 2008-2009. Ment Health Fam Med. 2010 Jun;7(2):71-84.
15. Ross CA, Goldner EM. Stigma, negative attitudes and discrimination towards mental illness within the nursing profession: a review of the literature. J Psychiatr Ment Health Nurs. 2009, 16(6):558-67.
P823
