The Physical Examination on Admission to the Acute Psychiatric Unit -complete Audit cycle
M.Elzain1, I. Elimam2, S. Barry2
1.Psychiatric Registrar limerick Mental Health services, Ireland
2.North Lee Mental Health Services, Ireland.
Abstract
While suicide and injury account for increased mortality, a large volume of premature deaths in psychiatry are due to medical conditions. The Royal College of Psychiatrists recommend that every new psychiatric admission should have a thorough physical examination within 24 hours of their admission. We randomly reviewed charts of 50 new admission to the Acute Psychiatric Unit to check the adherence to these guidelines. Forty patients (80%) had complete physical examination, nine patients (18%) had incomplete physical examination, and one patient (2%) had no physical examination in the Re Audit. This compares to 32 patients (64%) had complete physical examination, 16 patients (32%) had partial physical examination, and two patients had no physical examination (4%), in the first audit.There has been overall improvement in the physical examination since the first audit. However documentation of vital signs and weight remained and issue. Chaperon documentation had improved in the re-audit, although further improvement still required.
Introduction
While suicide and intentional injury account for increased mortality in psychiatry, a large volume of premature death in the person with schizophrenia are due to medical reasons such as cardiovascular disease, metabolic syndrome, and infectious diseases.
Historically patients with psychiatric disorders are discriminated against in A&E and primary care with regards to their physical care needs in comparison with patients with no psychiatric disorders when they presented with the same physical complaints.
Age-adjusted annual death rate from all causes among psychiatric patients are 2–4 times higher than in the general population (1).The risks of reliance on the believes that the patient’s general practitioner or other referring doctors have done a thorough physical examination have been emphasized by the psychiatrist(2).
Research evidence has showed that the recording of physical examination carried out on admission by psychiatric trainees to be ‘uniformly poor’ (3) or ‘variable’ (4).The earlier studies found that significant positive findings were unrecorded by the psychiatry trainees , especially in the locomotor and neurological systems. The recent studies showed little progress, with less than 60% of patients were having a comprehensive central nervous system examination (5). Studies have also shown that, in many cases, physical diseases will not be diagnosed or well treated when a patient is admitted to a psychiatric unit , which has potentially serious implications for patients’ overall health, delaying recovery and increasing the length of hospital stay (6)(7).
The Royal College of Psychiatrists and the Acute psychiatric unit local policy‘s (8) recommend that every psychiatric inpatient should have a thorough physical examination within 24 hours of their admission to the psychiatric ward .An open case of pulmonary Tuberculosis emerged in one of the acute psychiatric unit patients in July 2014 that highlighted the importance of screening for medical comorbidities at the time of admission.
Methods
Retrospective cross-sectional review of randomly selected charts of 50 new patients admitted to the Acute Psychiatric Unit in Mercy Hospital Cork-Ireland. The initial audit was performed on October 2014 to check the quality of the physical examination carried out on the new admitted patients during that period of time. Re audit was performed on October 2015.
For the purpose of the audit we developed a proforma designed for the study purpose to capture basic patient information’s. Examination would be classified into: Complete, Partial and None.
Following presentation of the initial audit results, the Clinical Director convened a committee involving psychiatric junior doctors, staff nurses, unit nurse manager and consultant psychiatrist to revise the admission sheet to the acute psychiatric unit which was to include the physical examination. A new physical examination template with prompt guidance and diagrams was introduced, a new tuberculosis screening questionnaire was also included. The aim of the re-audit was to complete the audit cycle and to determine if the revised template’s had led to an improvement in the standard of documentation of the psychiatric unit admission’s physical examination.
Results
From the 50 patients, 49 (98%) had a physical exam within 24 hours, one patient (2%) (Involuntary patient) didn’t have physical examination, we found no reason was documented to explain why no physical examination carried out. This compares to 48(96%) had physical exam within 24 hours, 2 patients (4%) refused the physical (both involuntary), in the first Audit. One of the latter 2 patients had a physical examination after 72 hours of his admission, the other patient continued to refuse the physical examination.
Forty patients (80%) had a complete physical examination, nine patients (18%) had a partial physical examination, and one patient (2%) had no physical examination. This compares to 32 patients (64%) had a complete physical examination, 16 patients (32%) had partial physical examination, and two patients (4%) had no physical examination in the first audit. Vitals were recorded in 33 patients (66%), vitals were not recorded in 16 patients (32%).
Weight documented in ten patients (20%) and was not documented in 40 patients (80%). This compares to vitals being recorded in 36 patients (75%), and weight documented in four patients (8.33%) in the first Audit.
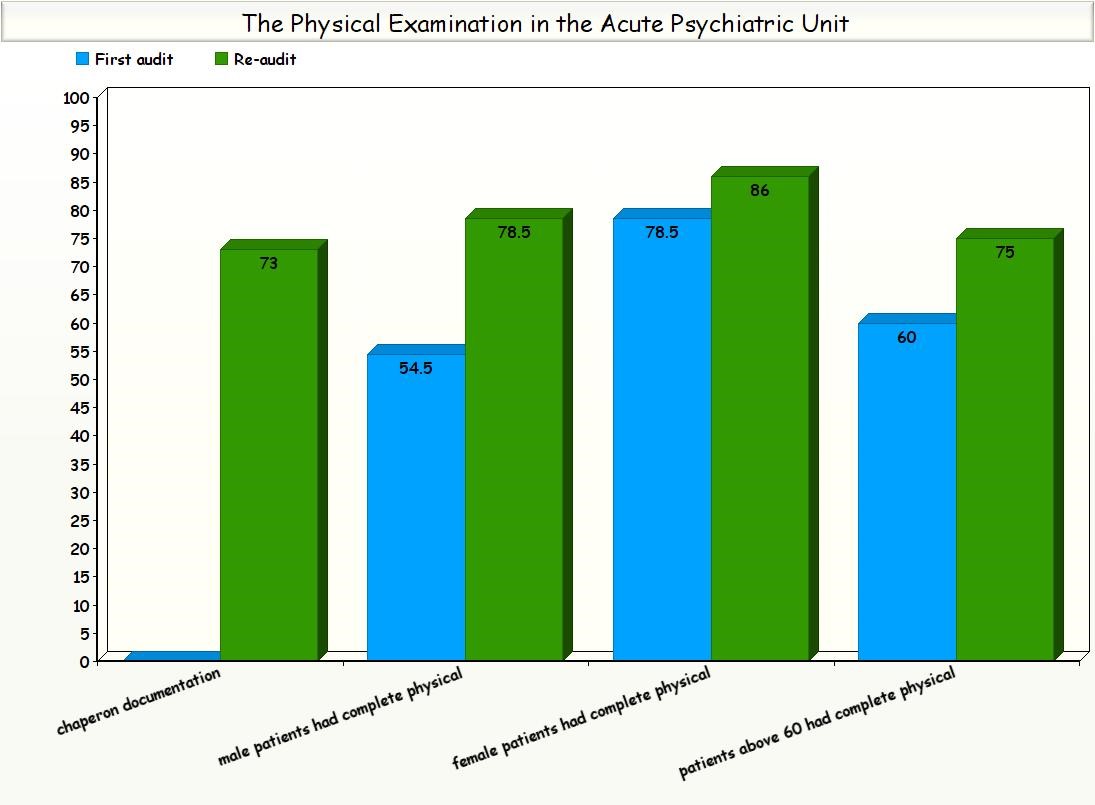
Of the 28 male patients, 22 patients (78.5%) had complete physical examination, and 6 patients (21.4%) had partial physical examination. Of the 22 female patients, 19 patients (86%) had complete physical examination, 2 patients (9%) had partial physical examination and one patient (2%) had no physical examination. This compare to the first audit, of the 22 male patients, 12 patients (54.5%) had complete physical examination and 10 patients (45.4%) had partial physical examination.
Of the 28 female patients, 22 patients (78.5%) had complete physical examination and 6 patients (21.4%) had partial physical examination in the first Audit.
Of the 12 patients older than 60 years, nine patients (75%) had complete physical examination, and three patients (25%) had partial physical examination .This compares to sex patients out of ten (60%) had complete physical examination in the first audit.
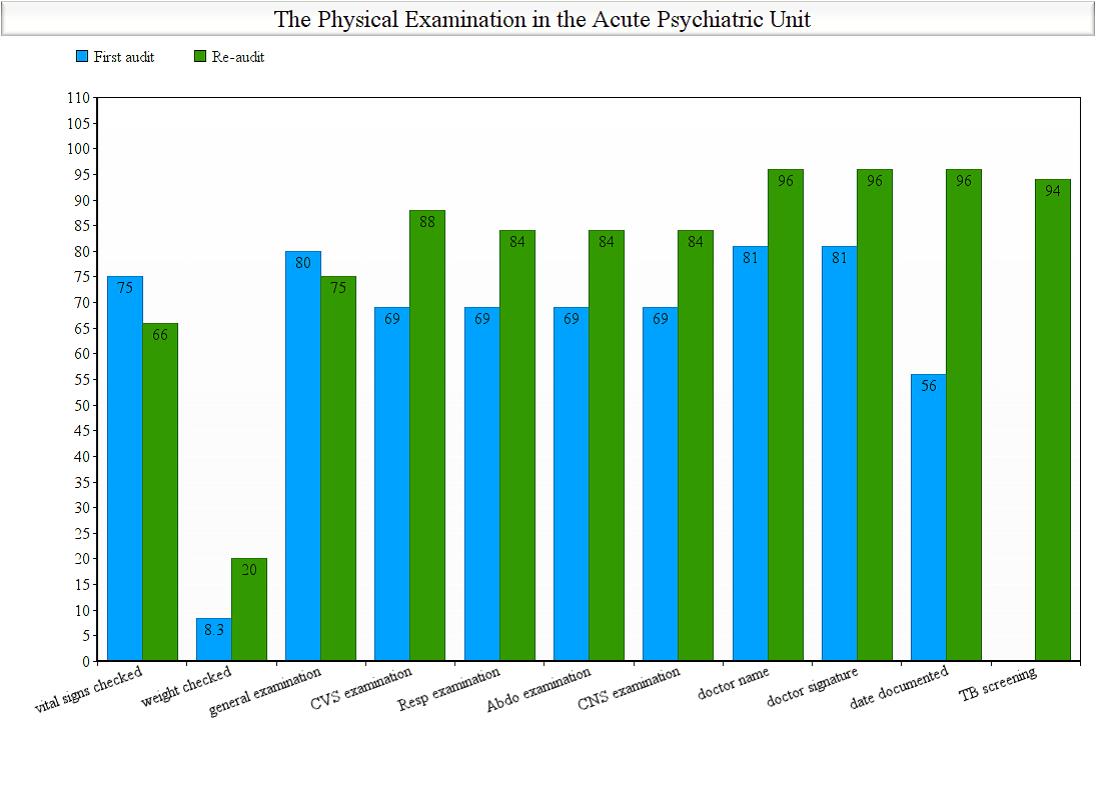
In term of the physical examination quality: (88%), (84%), (84%), (84%) had complete: cardiovascular, respiratory, abdominal and central nervous system, respectively. This compares to: (69%) for each of the four systems in the first audit. There was a remarkable improvement in documentation of doctor‘s name, signature, the date and time on which the physical examination took place (96%) for each in the second audit .This compares to (18.7%) in doctor’s name and signature and to (43.7%) for date documentation in the first Audit.
There was a notable improvement in chaperon documentation when appropriate from (0%) in the first audit to (70%) in the second audit .The TB screening questionnaire was completed in 47 of the 50 patients (94%) in the second audit.
Discussion
There has been an overall improvement in the quality and quantity of the physical examinations carried out on patients admitted to SMU (8) since the last audit. Documentation has improved with regards to the examiner’s name, time and date of the exam being carried out. Vitals documentation has declined since the last audit. Weight documentation still remains an issue since the last audit.
Male patients were more likely to have a partial physical examination in comparison to female patients , especially in the first audit, this could be explained by presentation factor(male patients are more are likely to be more agitated on admission than the female patients ), however this finding warrant further exploration in the future .
Although there has been a notable improvement in chaperon documentation when appropriate in the second audit, further improvement still required in this important area , as best medical practice guidelines.
Potential improvement may include addition of a new section in the physical examination sheet to document the nurse's name and signature of who helped with the vitals and weight recording.
Physical disease is more prevalent in people with mental disorder than in the general population.
It is important for psychiatrists to maintain skills in physical examination to ensure that physical illness is diagnosed and treated appropriately in their patients.
Physical examination and medical management is one of the main domains on the policies of the current Irish Royal college of Psychiatrist training requirement for both Basic and High Speciality Training, the current vision is ‘’ A Psychiatrist is able to assess physical health and comorbidity, as well as physical complications of psychiatric treatment, and is aware of physical morbidity presenting with psychiatric symptoms.
Physical Examination is therefore an integral part of psychiatric assessment. A Psychiatrist does not always have direct access to medical expertise and therefore is able to provide basic management of certain medical conditions’’ (9).However the evidence has showed that there is a real need for improving quality of the psychical examinations in the acute psychiatric unit as well overcoming barriers and obstacles.
One may think of those barriers as, Psychiatrist attitude towards patient’s physical examination: evidence has showed that psychiatrists didn’t physically examine their patients routinely (10). Some psychiatrists believe that physical examination should be done by other physician, not a psychiatrist.
Training: despite the colleges of psychiatry guidelines, there is still mileages to go, for attaining high standards in improving quality of the physical examination in the psychiatric settings. The fact that with the exception of vocational training in general practice, postgraduate medical training programmes are increasingly focused on specialty, which may be to the detriment of holistic patient care. As a consequence, the mental disorders of mentally ill patients may deter clinicians in acute hospitals from adequately managing medical illness, diagnosis and treatment of a physical disorders may be overlooked by their counterparts in psychiatric services (11).
Isolation from the general hospital: Although majority of the Acute Psychiatric Unit in Ireland are allocated in the general hospital buildings; there is a sense of isolation and difficulty of communications with the medical colleagues among the psychiatry doctors. Possibility of this may be due to the fact that, psychiatrist spend more time in the community than in hospital, and not sharing ground rounds, and other activities with their medical colleagues.
Suggestions of improvement would be routine demonstrations of physical examination in the teaching sessions in the acute psychiatric unit that would cover major systems e.g. Cardiovascular, Central Nervous System, Respiratory System, Gastro-intestinal system and Locomotors system, with supervision by visiting physicians. On those sessions trainees can both observe and be observed how to perform standard physical examination.
Those training sessions may be videotaped and kept available for new psychiatry doctors and may be included in the six month induction program.
Advocate a health passport for psychiatric patients aged over 60(attended to by GPs), that would result in a better communication of the general medical status of admitted patients, appropriate treatment of their physical problems and shortening of their psychiatric admission.
Conflicts of Interest
The authors of this audit have no conflicts of interest to disclose.
Ethical standards
The authors of this audit assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committee on human experimentation with the Helsinki Declaration of 1975, as revised in 2008.
Acknowledgements
Thanks to Dr. Sinead O'Brien Clinical Director-North Lee Mental Health Services –Cork.
Financial Support
The authors of this audit received no specific grant from any funding agency, commercial or not-for-profit sectors.
Correspondence:
Dr. M. Elzain
Psychiatric Registrar limerick Mental Health services,
Co. Limerick
Ireland
E-mail: [email protected]
Tel: +353877044270.
References:
1. Harris, E. C. & Barraclough, B. (1998) Excess mortality of mental disorder. British Journal of Psychiatry, 173, 11–53.
2. Sternberg, D. E. (1986) Testing for physical illness in psychiatric patients. Journal of Clinical Psychiatry, 47, 3–9.
3. Rigby, J. C. & Oswald, A. G. (1986) an evaluation of the performing and recording of physical examination by psychiatric trainees. British Journal of Psychiatry, 150, 533– 535.
4. Hodgson, R. & Adeyemo, O. (2004) Physical examination performed by psychiatrists. International Journal of Psychiatry in Clinical Practice, 8, 57–60.
5. Gill Garden, Physical examination in psychiatric practice, Advances in Psychiatric Treatment (2005).
6. Felker, B., Yazell, J. J. & Short, D. (1996) Mortality and medical comorbidity among psychiatric patients: a review. Psychiatric Services, 47, 1356–1363.
7. Moos, R. H. & Mertens, J. R. (1996) Patterns of diagnoses, comorbidities, and treatment in late-middle-aged and older affective disorder patients: comparisons of mental health and medical sectors. Journal of American Geriatric Society, 44, 682–688.
8. Saint Michael Acute Psychiatric Unit-Cork-Ireland.
9. CURRICULUM FOR BASIC AND HIGHER SPECIALIST TRAINING IN PSYCHIATRY, revision 5 July 2016.
10. S. Krummel and R. G. Kathol. (1987) What You Should Know About Physical Evaluations in Psychiatric Patients Results of a Survey. General Hospital Psychiatry 9, 275-279, 1987.
11. Bunce, D.F., et al., 1982. Medical illness in psychiatric patients: barriers to diagnosis
and treatment. South. Med. J. 75, 887–891.
P803
