The Profile of Women Attending the National Maternity Hospital Emergency Out Of Hours Service – Two Decades On. A Retrospective Review
O.F. O’Brien1, S. Lee2, A. Baby3, F.M. McAuliffe4, M.F. Higgins4
1. School of Medicine, University College Dublin
2. Obstetrics, National Maternity Hospital
3. Midwifery, National Maternity Hospital
4. UCD Perinatal Research Centre, National Maternity Hospital, University College Dublin
Abstract
Introduction
This study aimed to review the profile of women attending an out of hours emergency service (OHS) in a maternity hospital and compare it to a previous study.
Methods
Retrospective study. Demographic information was recorded including timing of presentation, reason and outcome.
Results
In 2017, 9,020 women attended the OHS, a 334% increase since 1993. On detailed review of 2,143 charts, most (84.7%, n=1,815) were antenatal. The most common reason for presenting to the OHS then was first trimester bleeding. In 2017, over half of antenatal women (51%, n=1,092) presented with “other” reasons, such as vomiting, hypertension or suspected pre-eclampsia. Admission rates significantly decreased from 1993 (38% (n=1,053) in 1993 vs. 16% (n=338) in 2017; p<0.05).
Discussion
Numbers attending for emergency maternity care have increased in both numbers and variety of presentations. It is important that women are seen and cared for in a compassionate, kind and evidence based manner.
Introduction
By its very nature obstetrics is a time dependent speciality. Women should be able to access emergency care at any time of the day or night whether their symptoms are minor or major. Waiting lists cannot and should not apply when a woman presents with early pregnancy bleeding, or a baby that has quietened in its movements, or severe hyperemesis. Maternal deaths due to haemorrhage, sepsis and hypertensive disorders still occur1. The maternity emergency department plays an important role in the recognition and prevention of maternal morbidity and mortality.
Two decades ago a review of the emergency service in the National Maternity Hospital was published2. At the time over 2,500 women presented for care outside of what is considered core working hours - that is, presented as an emergency for review between 4pm and 8am Monday to Friday or any time at the weekend (“out of hours –OHS”). Over three-quarters were women in the antenatal period (as opposed to women with postnatal or gynaecological issues) and many of these presented with symptoms of early pregnancy bleeding. This was in a year that just over 7,500 women had births within the hospital, so the OHS represented one third of the work of the labour ward3.
This study aimed to review again the profile of women attending the OHS and to compare this to two decades ago.
Methods
The National Maternity Hospital is a tertiary level stand-alone maternity hospital. The hospital provides obstetrics, neonatal, obstetric anaesthesia, community midwifery and allied health care to pregnant women and their babies. The gynaecology departments provide general gynaecology, urogynaecology, fertility and colposcopy care.
Within the hospital women can attend for either obstetric or gynaecology emergency care at any time of the day or night. Outside of “normal” working hours this care is provided within the OHS (“out of hours”) service. This service is staffed full time by one advanced midwife practitioner, three senior midwives with qualifications to perform early pregnancy ultrasound and supported by the on call obstetric team, both non-consultant and consultant hospital doctors.
Patient data is prospectively recorded by the midwife in charge in the OHS attendance record books. The total number of presentations by women attending for care in OHS in 2017 was recorded.
For more detailed examination, the OHS attendance books from the months of February-April 2017 were accessed in January 2018 and the data was recorded, specifically studying factors that would allow comparison to the previous study.
Women attending were classified based on timing of presentation – antenatal (AN), postnatal (PN) and gynaecological. Women in labour attend the labour ward directly. Home address was recorded.
Reason for referral was recorded based on symptoms or signs and then grouped to allow comparison with the previous paper. Route of referral was recorded as either self-referral, general practitioner (GP), clinic, other hospital or other. Numbers of ultrasound examination were recorded to allow comparison to the previous study.
Outcome of the attendance was recorded as either discharge home, admission, referral to other hospital (e.g. referral for second opinion to a general hospital) and other. Women were also recorded as having already attended the hospital for maternity care (“booked”) or attending for the first time in pregnancy (“unbooked”).
Results
In 2017, over 9,000 women delivered a baby under the care of the National Maternity Hospital. During this time 9,020 women attended the OHS for urgent or emergency care. This represents a 334% increase since the last review in 1993.
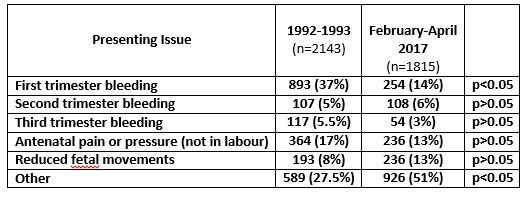 Table 1: Indications for women’s presentation to the Out of Hours Emergency Service in 1993 compared to February-April 2017. “Other” included vomiting, hypertension, suspected pre-eclampsia, an outside ultrasound suggestive of miscarriage or ectopic pregnancy
Table 1: Indications for women’s presentation to the Out of Hours Emergency Service in 1993 compared to February-April 2017. “Other” included vomiting, hypertension, suspected pre-eclampsia, an outside ultrasound suggestive of miscarriage or ectopic pregnancy
Focusing in on more detailed review over three months, 2,141 women attended the OHS during February-April 2017. Of these, 731 (34%) women were in the first trimester, 378 (17.6%) were in the second trimester, 706 (33%) were in the third trimester, 208 (9.7%) were postnatal and 117 (5%) were gynaecological. Antenatal patients comprised 1,815 of the women presenting (84.7%).
Most women (53%, n=1,135) were from Dublin City. One fifth (21%, n=446) came from County Dublin, 16% from County Wicklow and 4% from County Kildare. Six percent of women were from other places, including other Irish counties and foreign countries. Numbers attending from outside Dublin have increased since 1992 (40% (1992) vs 73% (2017) p<0.01).
The previous review had six options for presentation to OHS: first trimester (vaginal) bleeding, second (mid) trimester bleeding, third trimester bleeding (antepartum haemorrhage), pressure or pains not in labour, reduced fetal movements (RFM) or “other”. The most common reason for presenting to the OHS then was first trimester bleeding. Comparison with 1993 data is shown in Table 1. In 2017, over half of antenatal women (51%, n=1,092) presented with “other” reasons, such as vomiting, hypertension or suspected pre-eclampsia.
Postnatal and gynaecological patients accounted for just 15% (n=321) of the workload. The most common reason for referral (23%) of postnatal women to the OHS was suspected episiotomy/caesarean section wound infection, while 63% presented with ‘Other’ reasons, mainly increased lochia and urinary tract infection. Gynaecological patients presented for a wide variety of reasons, the main reason being abnormal uterine bleeding.
Most women self-referred, a total of 1534 patients (72%). One in ten women were referred by their GP, a slight decrease from the 1993 figure of 12%. ‘Other’ accounted for 5% of referrals, consisting of referrals from public health nurses, community midwives, and transfer from another hospital.
One-third of women (n=758; 35%) had an ultrasound scan, while 40% had a laboratory test (e.g. mid-stream urine specimen or blood test). This shows an increase in scans performed since 1993, while this is not statistically significant (28% vs 35%, p>0.05) it is clinically significant to the workload of the department.
Regarding discharge, the majority (81%, n=1,724) of women were discharged home, while 16% (n=338) were admitted. A small proportion (2%) of women were referred to other hospitals. There was a statistically (and clinically) significant decrease in admissions from 1993 (38% in 1993 vs. 16% in 2017; p<0.05).
Women who were not formally booked to the hospital continued to account for a large proportion of the workload of the OHS (35% in 2017 vs 30% in 1993, p>0.05); while this was not statistically significant it was also clinically significant.
Discussion
This study has identified striking differences over the last twenty years in the profile of women attending for emergency maternity care. A clinically and statistically significant difference is the huge increase in numbers as well as different reasons for presentation. In 2002 the hospital opened an Early Pregnancy Assessment Unit (EPAU), allowing women with first trimester bleeding or pain to present for review during working hours and be seen by a fully qualified ultrasonographer. This is now standard of care; women who ring for advice are often provided with the next available EPAU appointment and do not have to present as an emergency. Instead of presenting with early pregnancy bleeding, women now present with multiple other concerns - as an example, in the third trimester women’s reasons for presentation ranged from constipation to facial lesions to spontaneous rupture of membranes (SROM) or administration of anti-D. It is perhaps this group that best represents the ‘catch-all’ service that the OHS has become.
Women are now travelling further distances to attend, though this may well represent changing demographics due to the increasing commuter distance noted over the last two decades.
Many women self-referred to hospital, while only 10% had GP referral letters. The low proportion of women with GP referral letters may indicate that pregnant women attend OHS directly. A Dutch study found that pregnant women there attend their GP more frequently than non-pregnant women4. The possibility and capability of GP care in pregnancy should be reinforced in the Irish setting, though limitations will be discussed later in this discussion.
An ultrasound was performed on 35% of women attending the OHS. This is a large workload but is necessary for the diagnosis of women with miscarriage or ectopic pregnancy or, quite often, for the reassurance of a woman with RFM or threatened miscarriage 5. This increase in USS may be related to the decrease in admission rates seen. All obstetricians in training must complete a mandatory ultrasound course as part of their basic specialist training; midwives working in the unit complete a formative assessed course to gain a standard of expertise to provide ultrasound assessment.
Only 16% of women required admission to the hospital. As noted previously, an increased number of midwives working within the unit with the ability to perform ultrasounds and make diagnoses, as well as support by senior obstetric staff, means that management decisions need not to be deferred until the morning. Increasingly women with hyperemesis receive intravenous fluids in the OHS and are then discharged home rather than being admitted. Some of the women presenting to the OHS need reassurance rather than medical care. Many women are working while pregnant and may not be able to attend a GP within normal working hours. The nature and timing of the complaint, their concerns with regard to their pregnancy, the cost of a GP visit, distance from the hospital all play a part in determining who may present for care. “Unbooked” women accounted for 35% of the referrals to the OHS. These women contribute to a greater workload due to the necessity to include a booking visit - a highly detailed history as well as several blood tests - in their visit to the OHS.
The number of women presenting with RFM has nearly doubled. This may be due to increased awareness of the OHS and encouragement of women by NMH staff to present should this occur, especially after a major educational programme encouraging women to present early if they had RFM.
A review of the workload of the Emergency Room (ER) in the Rotunda Hospital, Dublin, showed some similarities and differences6. The number of women attending the ER remained relatively stable over a three-year period, with 7828 women attending in 2009 and 7704 women in 2012. More antenatal women attend (91% in 2009), probably because women in suspected labour are triaged through the ER. The remaining 9% approximately evenly split between postnatal and gynaecological patients. This means that while the number of gynaecological patients seen in the NMH OHS is relatively similar, the NMH sees approximately double the proportion of postnatal women. Also of note is the significant difference in admission rates – 36.6% in the Rotunda Hospital in 2009 versus 16% in the NMH in 2017, though this may be because of admission of women in labour rather than increased non-labour emergency admissions.
The strengths of this review are the prospective collection of data and the large sample size studied. Limitations of the study are that only three months of the year were studied, so seasonal variation in the profile of women attending may be a factor.
This study established the importance of an emergency service in maternity care and the need for dedicated skilled staff to provide this service. In February 2018, a dedicated area for emergency care was opened in the hospital further highlighting this service. Women deserve to be able to present at any time of the day or night with an issue of concern to them and to be seen by a skilled compassionate clinician who can provide care to them. The Emergency Service is the door for this care for many women.
Conflicts of Interest Statement
The authors have no conflict of interest to declare.
Corresponding Author
Mary F. Higgins,
UCD Perinatal Research Centre,
National Maternity Hospital,
University College Dublin
Email: [email protected]
References
1. Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels JD, Gulmexoglu AM, Temmerman M, Alkema L. Global Causes of Maternal Death: A WHO Systematic Analysis. Lancet Global Health. 2014;2(6): e323-e333.
2. McAuliffe F, Hoey M, Geary M. The National Maternity Hospital Casualty department – a review. Ir Med J 1997 Jan-Feb 90(1):19
3. National Maternity Hospital Annual Report, 1993. Dublin, Ireland
4. Feijen-de Jong EI, Baarveld F, Jansen DE, Ursum J, Reijneveld SA, Schellevis FG. Do pregnant women contact their general practitioner? A register-based comparison of healthcare utilisation of pregnant and non-pregnant women in general practice. BMC Fam Pract. 2013;14:10.
5. Sotiriadis A, Papatheodorou S, Makrydimas G. Threatened miscarriage: evaluation and management. BMJ. 2004;329(7458):152-5.
6. Talukdar S, Eogan M, Connolly G, Coulter-Smith S. The emergency room at the Rotunda Hospital: evidence of an improving service over the past 3 years. Ir J Med Sci. 2014;183(4):681-3.
P895
