IgG4 Related Disease, A Case of Large Vessel Vasculitis
A. O’Sullivan, S. Ghazi Al Qatari, G. Murphy
Rheumatology Department, Cork University Hospital
Abstract
Aim
This report describes a case of large vessel vasculitis highlighting diagnostic and therapeutic challenges. It describes the use of the B cell depleting agent Rituximab in this setting. This is the case of a 50 year old lady with bipolar disorder presenting with lower limb pain.
Method
PET CT and CT angiography were employed in the diagnosis of a large vessel vasculitic process. Serum IgG4 was elevated. Histological sampling was not clinically feasible. A presumptive diagnosis of IgG4 related disease was made.
Results
The patient responded well to steroids and later rituximab. A prompt taper of steroids was required due to labile mood and Rituximab proved to be effective in this case as a maintenance therapy.
Conclusion
This case demonstrates that a combination of clinical findings, laboratory results and radiological imaging may be necessary for diagnosis for IgG4 related disease, especially in the absence of a histological diagnosis. Rituximab was used in this case as a maintenance therapy allowing for a relatively rapidly reducing course of steroids.
Introduction
IgG4 related disease is a systemic condition which can affect virtually any organ1. Autoimmune pancreatitis is the most frequent manifestation of IgG4 related disease. The epidemiology is poorly reported2.
IgG4 related disease is a distinct cause of vasculitis and can have a variety of vasculitic manifestations3.
Case Report
A 50 year old lady with a background of bipolar affective disorder and mild intellectual disability presented to the hospital due to fluctuating mobility and lower limb pain. She was a non smoker.
Her mobility problems began four months prior to presentation. She complained of intermittent lower limb pain with associated ‘weakness’. The patient’s sister, and carer, noted a recent increase in elation and a regression in self- care. A neurological examination was normal. There was no clinical evidence of fracture or Deep Vein Thrombosis. Medications on admission included; olanzapine, biperidin, sodium valproate and diazepam.
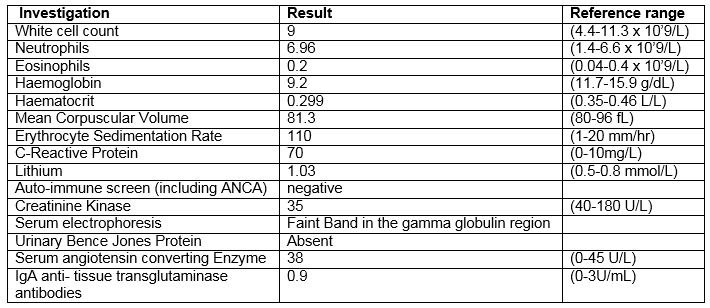
Initial investigations can be viewed in Table 1 below.
The patient was admitted for investigation of an infective or inflammatory cause of her symptoms in the setting an elevated ESR and CRP. Chest X-Ray, blood and urine cultures failed to identify any abnormality. A CT thorax, abdomen and pelvis identified ground glass change at the lung bases. MRI lumbar spine demonstrated degenerative disk disease.
Fluctuating mobility was noted throughout her admission with limitations noted to be secondary to pain. Her psycho-active medications were altered in conjunction with the liaison psychiatry team and her mood stabilised.
Shortly thereafter she described ‘knife like’ pains localised to the thighs. She did not report lower limb weakness or paraesthesia. She described a sensation of weakness of the right upper limb as well as numb fingers. There was decreased right sided grip strength and sensation was intact.
A PET CT showed increased uptake in the subclavian, axillary and proximal brachial arteries as well as the femoral arteries. Dedicated CT angiography of the upper limbs showed bilateral axillary arteritis with mild multi -level stenosis. Lower limb CT angiography similarly identified multilevel occlusive disease.
The decision to implement steroid therapy for the new diagnosis of large vessel vasculitis was made after careful consideration and discussion with the psychiatry team. The patient’s recent labile mood and episodes of elation made the risk of worsening symptoms or steroid psychosis concerning. However, prednisolone 0.5mg/kg was initiated and the psychiatry team provided daily monitoring.
During this period the serum IgG4 subclass was noted to be elevated at 1.64 (0.039-0.864). This made the diagnosis of IgG4 related disease a possibility. Although diagnosis of this condition is aided by histological examination of affected tissue, there were no suitable biopsy sites in this case. Treatment was instigated based on the clinical diagnosis. Rituximab was the steroid sparing agent used. The patient has received the first cycle of rituximab and remains on a slowly tapering dose of steroid. She has symptomatically improved and her inflammatory markers are trending downwards.
Discussion
Diagnosis of IgG4 related disease is aided by histopathological analysis. The classical histological appearance is a lymphoplasmacytic infiltrate in a storiform pattern with associated obliterative phlebitis. An isolated elevated serum IgG4 is not a specific diagnostic test1. Expert consensus recommends a combination of clinical findings in association with laboratory investigations and radiological findings for diagnosis4. In this case, the patient was treated for IgG4 related disease based on the clinical diagnosis and responded well to therapy.
Several chronic inflammatory conditions potentially including ANCA associated vasculitis can be associated with raised serum IgG45,6. Careful consideration must be given when interpreting the results of raised serum IgG4. For example, in this case other large vessel vasculitides such as Takayasu’s arteritis should be considered as a differential diagnosis.
The first line treatment for IgG4 related disease is steroids. Rituximab is a second line agent4.
In our clinical case, the decision to start steroid therapy presented a challenge. The patient had poorly controlled bipolar disorder. Rituximab implemented early was used to good effect.
Conflict of Interest
The authors have no conflicts of interest to declare.
Correspondence:
Aoife O’Sullivan
Address: Department of Rheumatology, Cork University Hospital, Cork, Ireland.
Fax: 021 4920131
phone: 00353 851342232
Email: [email protected]
References
1. Stone JH, Zen Y, Deshpande V. IgG4- Related Disease. The New England Journal of Medicine. 2012;366(6):539-51.
2. Pieringer H, Parzer I, Wöhrer A, Reis P, Oppl B, Zwerina J. IgG4- related disease: an orphan disease with many faces. Orphanet Journal of Rare Diseases. 2014;9:110-.
3. Perugino CA, Wallace ZS, Meyersohn N, Oliveira G, Stone JR, Stone JH. Large vessel involvement by IgG4-related disease. Medicine. 2016;95(28):e3344.
4. Khosroshahi A, Wallace ZS, Crowe JL, Akamizu T, Azumi A, Carruthers MN, et al. International Consensus Guidance Statement on the Management and Treatment of IgG4-Related Disease. Arthritis & rheumatology (Hoboken, NJ). 2015;67(7):1688.
5. Perez Alamino R, Martínez C, Espinoza LR. IgG4-associated vasculitis. Current rheumatology reports. 2013;15(8):348.
6. Della-Torre E, Lanzillotta M, Campochiaro C, Bozzalla E, Bozzolo E, Bandiera A, et al. Antineutrophil cytoplasmic antibody positivity in IgG4-related disease: A case report and review of the literature. Medicine. 2016.
P824
