Quality Improvement of Clinical Handover in a Liaison Psychiatry Department: A Three-Phase Audit
L Alexander,1,2 N Bechan, 1 S Brady, 3 L Douglas, 1 S Moore, 1 R Shelley. 1
1St Vincent’s University Hospital, Dublin
2University College Dublin
3St John of God of God Community Services.
Abstract
Aims
To audit and improve quality of clinical handover in a Liaison Psychiatry Department.
Methods
An 11-item Handover Checklist was used to carry out a baseline audit and immediate and delayed post-intervention re-audits. The intervention consisted of checklist posters, an electronic database and staff training.
Results
There was an immediate and sustained improvement in most areas, including baseline demographics and components of SBAR communication (Situation, Background, Assessment, Recommendation). The improvement between baseline and delayed re-audit was statistically significant (P=0.007).
Conclusion
Poor handover practices contribute to negative outcomes in healthcare but there remains a dearth of guidelines in most specialties.This audit is important as it describes an intervention which improved clinical handover at a time of significant clinical risk. This practice could be applied effectively to other services and is relevant to all specialties. Six to twelve-monthly re-audit and longitudinal assessment of clinical outcomes are recommended to maintain the practices implemented in this audit.
Introduction
Clinical handover has been identified as a period of high risk in healthcare, with increased incidence of adverse outcomes and near-misses. The purpose of handover is to communicate relevant information between medical professionals, with emphasis on completing management tasks and preventing patients from ‘falling through the cracks’1. Poor handover practices contribute to catastrophic but avoidable adverse events in healthcare. In Ireland, one such high profile incident has been a particular catalyst in the development of comprehensive handover guidelines in maternity settings2. Other specialities have yet to follow suit and there remains a dearth of guidance on handover practices, particularly guidance that can be applied to highly specialised and logistically unique areas, such as psychiatry.
Good communication of relevant information between professionals involved in patient care has been highlighted by the Royal College of Psychiatrists (UK)3. The National Self-Harm Programme identifies clinical handover as an essential component of risk management4. These documents, along with the HSE-generated guidelines around clinical handover in maternity and paediatric settings2 recommend that handover should take place at a designated time and in a designated, private space, with no interruptions except for emergencies. All patients should be discussed at clinical handover and transfer of responsibility should be made clear. The World Health Organisation (WHO) and Joint Commission International (JCI) guidelines emphasize that handover of excess information that has no impact on immediate management can cause important information to become lost among other details5. Studies have indicated that written protocols are superior to verbal guidance alone6. Checklists have been shown to improve clinician compliance with guidelines and patient safety overall in a variety of medical settings7. SBAR (Situation, Background, Assessment, Recommendation) is a well-supported tool which facilitates effective communication in clinical settings. SBAR is a simple mechanism which enables professionals to focus a conversation to include relevant information and reduces the need for repetition5.
The aim of this study was to audit the existing handover practices in a Liaison Psychiatry Service against a Gold Standard and to implement an intervention to improve quality of handover. In lieu of specific guidelines, the Gold Standard consisted of basic patient demographics, SBAR guidelines and other information specific to our service. The target was to achieve consistent, high quality handover that is concise and complete, while avoiding unnecessary detail. The aim was therefore to reach 100% compliance.
Methods
The present audit took place in the Liaison Psychiatry Department of a Dublin-based 500-bed Academic Teaching Hospital. The Liaison Psychiatry and Psychiatry On Call Services provide 24-hour psychiatric cover to the Emergency Department. Handover in this service is multidisciplinary (psychiatry consultant/senior registrar, psychiatry registrars, self-harm nurses, social worker) and takes place at the start of the day shift in the team office between the psychiatry night staff and the Liaison Psychiatry Team. Handover is led by either a consultant or senior registrar. The handover leader is responsible for ensuring that all management plans are followed through. Evening and weekend handovers were not audited in this study as it was important for the checklist to be completed consistently by the same individual, which was only possible for weekday morning handover.
An 11-item checklist was devised using criteria agreed upon by the Liaison Psychiatry Multidisciplinary Team. This checklist was completed on consecutive days for a period of three weeks by an impartial observer, a psychiatric doctor whose handovers were not included in the audited data. This observer also provided useful insight regarding the degree to which handovers were concise, structured and consistent. The items on the checklist were: patient name, age, address/catchment area, situation, background, assessment, recommendation (SBAR), follow-up phone call (by self-harm nurse), and GP communication. Doctors were also required to explicitly state whether or not each case was discussed with the consultant on call, although there was no obligation to discuss every case.The intervention consisted of Training and Prompting components. The Training Intervention comprised: a) a focused meeting with the Liaison Psychiatry Team to summarise the audit details and achieve buy-in; b) a mandatory training session targeting the registrars on the on-call rota.
The Prompting Intervention comprised: a) guideline checklists were displayed on A2 posters in the handover office; b) the poster guidelines were matched to an electonic database (Excel) in a Liaison Psychiatry shared drive. Data is entered by the assessing clinician prior to handover in the same format as verbal presentation. Self-harm nurses cross-match database entries with ED attendance records on a daily basis to ensure full adherence. Handovers were re-audited immediately following the intervention for two consecutive weeks. This was followed by a two week interval and then a third audit in order to establish stability of change. The differences between each of the audit groups were compared using a two-tailed paired T-Test. P-Values were obtained to evaluate statistical significance.
Results
Baseline
Handovers on consecutive weekdays over a period of three weeks were included in this part of the study. A total of 44 patients were discussed in this time period. None of the cases handed over were fully compliant with the handover checklist. On average, each handover was 62% compliant. Regarding use of the SBAR format, quantitatively the compliance level was reasonably good, with information provided for all headings in 32 cases out of 44. However, the researcher completing the checklist observed that in most cases the information was excessive and lacked the intended structure of SBAR. Therefore, this figure of 72% compliance cannot be taken at face value. All results are illustrated in Table 1.
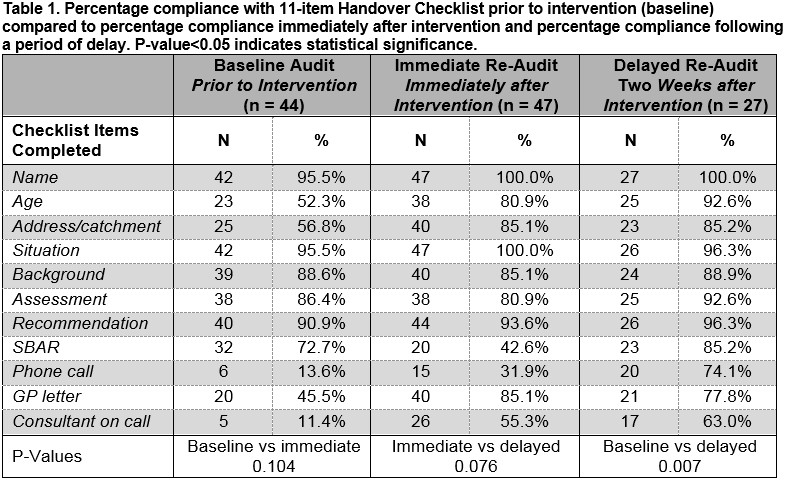
Post-Intervention Audit: Immediate
Immediate re-audit following implementation of the intervention demonstrated an improvement in communication of basic demographics (name, age, catchment area) with a modest improvement in situation and recommendation parts of SBAR. Full SBAR compliance, where all four components were included, appeared to have reduced to 44%, which probably reflected the initial efforts to reduce excess information. Differences noted in checklist compliance between the immediate re-audit and the baseline audit were not statistically significant (P-value=0.104). The handovers were generally observed to be more structured and concise.
Post-Intervention Audit: Delayed
A delayed re-audit following implementation of the intervention found a sustained improvement in basic demographics. Compliance with SBAR was at its highest in this part of the audit process (85%), from which we inferred that this method of communication requires experiential learning. There was a statistically significant improvement in checklist compliance between baseline audit and delayed re-audit (P=0.007) and a statistically insignificant improvement between immediate and delayed re-audits (P=0.076).
Discussion
This audit is important as it describes an intervention which improved clinical handover at a time of significant clinical risk. Individuals who have presented to an Emergency Department are 50 times more likely to eventually complete suicide8,9 but risk of suicide overshadows a variety of other important risks including self-neglect, neglect of dependents, harm to others and risk of further deterioration. Models of Change in management fields emphasize the value of incremental progress when it comes to making sustainable improvements10. Small, gradual changes are more palatable than complete systemic overhaul and many change processes fail because they are too ambitious. It is essential to have commitment from a cohesive multidisciplinary team in order to create change. In this study, we achieved stakeholder buy-in by implementing Kotter’s concept of creating short term wins10. We highlighted the potential benefits as they applied to both the service (enhanced efficiency, improved patient outcomes, reducing multiple presentations) and the individual clinician (saving time at the end of shift, avoiding excessive questioning and repetition).
Prior to undertaking this intervention, handover in the Liaison Psychiatry Department was overly inclusive and lacked consistency. Large quantities of information were handed over concerning patients who had already left the Emergency Department, but important details about future management were omitted. The SBAR communication technique was selected as it is widely used and prevents clinicians becoming bogged down in small details, thereby losing sight of the bigger clinical picture5. Having invested substantial staff resources into the intervention phase and successfully engaging the stakeholders in training, we had expected to observe an initial surge of compliance immediately following the intervention with a plateau or slight reduction in compliance after an interval period. In fact, the results indicated a further improvement in compliance in the second month after the intervention. These findings suggest that it was initially a challenge for the on-call doctors to assimilate to the abridged style of communication but, with time, practice and guidance, they adapted well to the change. The upward trend of compliance is a reassuring indication that this change has the potential to be sustainable long-term.
Other interventions exist that may assist teams with improving quality of clinical handover. Some studies have considered handover to rely on the combination of ‘technical skills’ and ‘non-technical skills’11. Technical skills are procedure-specific (e.g. adherence to the checklist structure). Interventions to improve technical skills may include providing prompt cards for doctors at handover, although previous studies have found poor uptake of this intervention12. Non-technical skills refer to the cognitive, social and personal resource skills that complement technical skills. Non-technical skills (e.g. communication, teamwork, situational awareness) contribute to competence but are difficult to teach and transfer. While non-technical skills may be learned by individuals over time, this is not an immediately practicable intervention to improve quality of handover. It therefore may be the case that the presence of an already skilled senior night nurse is needed to supplement any non-technical skills deficits in the junior doctor. Presence of a nurse manager at handover meetings has been beneficial in other studies12.
Outcomes in Liaison Psychiatry are acknowledged to be inherently difficult to measure, in large part due to the heterogeneity of activities, presentations and environments13 and it would be impracticable, within the scope of this study, to measure whether implementation of this strategy actually improved efficiency or patient outcomes. This is a limitation of our study but long term clinical outcomes could be evaluated in the future using a longitudinal approach to build on the existing body of research advocating for clear clinical handover guidelines. The sustained improvement, especially SBAR compliance, demonstrated on delayed re-audit and the positive response from stakeholders should be considered measures of success. A second limitation in this study was the difficulty in measuring the quality of communication in handover. Quantitative data was easily obtained in this audit using the checklist approach but the way in which information was communicated was difficult to qualify, even having incorporated SBAR. We therefore relied on the observation of the independent participant to describe the conciseness and orderliness of handover. A third limitation was that weekend and evening handovers were excluded. This may have an impact of the results, although it is expected that improving handover practices at one time will coincide with improved practices in general.
Clinical audit is an important component of clinical governance which contributes to the maintenance of high standards of healthcare delivery14. The focus of this audit, clinical handover, is an important area of risk management that transcends any specific medical speciality. This practice could be adapted effectively to other services. In such cases, we recommend that the time devoted to SBAR training should be sufficient to achieve buy-in, participate in practice cases and engage stakeholders in critical discussion. The temptation within a busy service can be to rush through this phase, which will ultimately compromise the success of the intervention. Change should be anchored by eliciting feedback from stakeholders on an ongoing, regular basis in order to sustain momentum and random re-audits should be undertaken on a six to twelve month basis.
Declaration of Conflicts of Interest
The authors declare no conflicts of interest
Correspondence
Lauren Alexander,St Vincent’s University Hospital, Dublin,
Email: [email protected]
References
1. Marmor G, Li M. Improving emergency department medical clinical handover: Barriers at the bedside. Emergency Medicine Australasia: Emergency Medicine Australasia. 2017; Jun;29(3):297-302.
2. Communication (Clinical Handover) in Maternity Services: National Clinical Guideline No. 5ISSN 2009-6259. Published November 2014.
3. The Royal College of Psychiatrists. College Report CR154: Good Psychiatric Practice. Third edition, 2009. Available from: http://www.rcpsych.ac.uk/pdf/REVAL2013%203%20Good%20Psychiatric%20Practice.pdf. Accessed 9th June 2017.
4. The Health Service Executive and the Irish College of Psychiatrists. National Clinical Programme for the Assessment and Management of Patients Presenting to Emergency Departments following Self-Harm. March 2016. Available from: http://www.hse.ie/eng/services/publications/Clinical-Strategy-and-Programmes/National-Clinical-Programme-For-the-Assessment-and-Management-of-Patients-Presenting-to-Emergency-Departments-following-Self-Harm.pdf. Accessed 1st December 2017.
5. World Health Organisation. Communication During Patient Handovers. Patient Safety Solutions volume 1, solution 3, May 2007.
6. Brook J, Amaro Calcia M. Improving the quality of handover in a liaison psychiatry team. BMJ Quality Improvement Reports. 2016 Jun; 6;5(1).
7. Thomassen Ø, Storesund A, Søfteland E, Brattebø G. The effects of safety checklists in medicine: a systematic review. Acta anaesthesiologica Scandinavica. 2014 Jan; 58(1):5-18.
8. Hawton K, Bergen H, Cooper J, Turnbull P, Waters K, Ness J, Kapur N. Suicide following self-harm: findings from the multicentre study of self-harm in England, 2000-2012. Journal of Affective Disorders. 2015;175:147-51.
9. Bergen H, Hawton K, Waters K, Ness J, Cooper J, Steeg S, Kapur N. Premature death after self-harm: a multicenter cohort study. Lancet. 2012; 380:1568-74.
10. Steven H. Appelbaum, Sally Habashy, Jean‐Luc Malo, Hisham Shafiq. Back to the future: revisiting Kotter's 1996 change model. Journal of Management Development. 2012; 31: 8, pp.764-782
11. Pezzolesi C, Manser T, Schifano F, Kostrzewski A, Pickles J, Harriet N, Warren I, Dhillon S. Human factors in clinical handover: development and testing of a ‘handover performance tool’ for doctors' shift handovers. International Journal of Quality in Healthcare. 2013 Feb; 25(1):58-65
12. Walton H, Munro W. Improving the quality of handover by addressing handover culture and introducing a new, multidisciplinary, team-based handover meeting. BMJ Quality Improvement Reports. 2015 Jul; 14;4(1).
13. Fossey M, Parsonage M. Outcomes and Performance in Liaison Psychiatry: Developing a Measurement Framework. Centre for Mental Health, 2014. https://www.centreformentalhealth.org.uk/Handlers/Download.ashx?IDMF=eb1da521-16f9-4beb-9c34-a6064b0e9950. Accessed 7th July 2017.
14. Quality and Patient Safety Directorate: A Practical Guide to Audit QPSD-D-029-1. August 2013. Available from http://www.hse.ie/eng/about/Who/qualityandpatientsafety/Clinical_Audit/clauditfilespdfs/practicalguideclaudit2013.pdf. Accessed 9th June 2017.
(P767)
