Scope and Safety of Paediatric Surgery in a Model III Hospital
D.P. Joyce1, R. Craig1, A. Dakin1, H. Elsheik1, T. Ejaz1, S. Mansoor1, D.P. Toomey1
1. Department of Surgery, Regional Hospital Mullingar, Co. Westmeath
Abstract
Introduction
Elective and emergency paediatric general surgery is performed in numerous hospitals but with differing exclusion and transfer thresholds. Recent national guidelines detail necessary surgical, anaesthetic and nursing resources for safe and efficient delivery of services.
Methods
A retrospective review of paediatric surgical admissions was performed from January 2015 to December 2016. Charts of prolonged admissions or readmissions were reviewed.
Results
There was a total of 2,079 surgical admissions. 575 (27.2%) were elective and 1504 (71.2%) were emergency admissions. Significantly more surgical procedures were performed in 2016 (n=546, 56% versus n=433, 44.2%). Laparoscopic appendicectomy was the most commonly performed procedure. Re-admission rates were lower in 2016 (n=9, 0.8% versus n=21, 2.2%). All complications were Clavien-Dindo Grade I or II.
Discussion
Paediatric general surgery can be safely and efficiently performed by staffed and resourced Model III hospitals.
Introduction
In 2016 the Faculty of Paediatrics in the Royal College of Physicians of Ireland, in conjunction with the Royal College of in Surgeons Ireland and the Health Service Executive, published the National Clinical Programme for Paediatrics and Neonatology: improving services for general paediatric surgery1. The purpose of these guidelines was to ensure the provision of safe and efficient paediatric general surgery outside of specialist paediatric hospitals in both local and regional paediatric surgical facilities.
These guidelines were necessitated by a variety of factors including the retirement of a generation of consultant surgeons with paediatric surgical skills, a lack of paediatric surgical training for core trainees, increasing sub-specialisation within the field of general surgery with the resultant de-skilling of supporting anaesthetic, radiology and nursing colleagues, and inadequate funding of paediatric surgical services. These challenges are compounded by Ireland having the lowest number of paediatric surgeons per capita when compared to other European countries, despite having the highest birth rate in Western Europe1.
Core recommendations included the presence of appropriately trained staff, 24 hour anaesthetic, surgical and nursing services, onsite inpatient paediatric medical unit (or access to paediatiric consultant opinion), a dedicated anaesthetist subspecializing in paediatrics, and the presence of a clear transfer pathway to paediatric hospitals1. The Regional Hospital Mullingar serves a total population of 291,0002, with a high demand for general paediatric surgical services. The aim of this study was to examine the volume and outcomes for paediatric general surgery in a model III hospital catering for children aged greater than 12 months of age.
Methods
A retrospective review of surgical admissions to the paediatric ward in the Regional Hospital Mullingar from January 2015 to December 2016 was performed. Data were collated by interrogating the Hospital In Patient Enquiry (HIPE) system and In Patient Management System (IPMS). All elective and emergency general surgical admissions to the paediatric ward were examined. Management strategies employed in all cases and outcomes were recorded. Charts of prolonged admissions (hospital stay greater than 7 days), transfers to paediatric hospitals, and re-admissions within 30 days of discharge were reviewed. Management and outcomes for all cases were compared to that of the National Clinical Programme for Paediatrics and Neonatology: improving services for general paediatric surgery guidelines1.
Data were analysed using SPSS version 12. Comparisons were made between groups using Chi-square for categorical variables. Results are presented for 2015 and 2016 in an effort to measure the effect of the National Clinical Programme for Paediatrics and Neonatology report on patient outcome.
Results
Patient demographics
There were a total of 2,079 paediatric surgical admissions between January 2015 and December 2016. Patients were managed by 1 of 4 consultant surgeons. Of these, 575 (27.2%) were elective admissions and 1504 (71.2%) were emergency admissions. In 2015, the majority of admissions were male (n=587, 61.4%, versus n=369, 38.6% for females, P<0.05, Table 1). A similar trend was also noted for 2016 (n=711, 63.3% males versus n=412, 36.7% for females, P<0.05, Table 1). Among the surgical admissions, 597 (28.7%) were under the age of 5, 700 (33.7%) were between 5 and 10 years old and 782 (37.6%) were aged greater than 10 years and less than 16 years of age (P<0.05, Table 1).
Length of stay
Seven hundred and thirty one patients (76.5%) of admissions lasted less than 24 hours in 2015 and 849 (75.6%) in 2016 (P=0.65).
Caseload
Nine hundred and seventy nine procedures were performed on children 15 years and under in the 2-year period with significantly more being performed in 2016 (n=433 (44.2%) in 2015, n=546 (56%) in 2016, P<0.05). Two hundred and thirty eight (55%) of operations were performed electively in 2015. Similarly, 285 (52.2%) of operations were performed electively in 2016 (P=0.39).
Commonly performed procedures
Laparoscopic appendicectomy was the most commonly performed surgery across both years of the study accouting for 22.6% (n=98) and 24.9% (n=136) of procedures in 2015 and 2016 respectively (P=0.41). Two hundred and thorty four appendicectomies (99.2%) were completed laparoscopically (n=234), with only 0.85% (n=2) necessitating conversion to open. The youngest age at which this procedure was completed laparoscopically was 2 years. The majority of appedices were uncomplicated (n=127, 53.8%) on histological examination, followed by impacted faecolith (n=35, 14.8%), perforated appendicitis (n=19, 8.1%), lymphoid hyperplasia (n=17, 7.2%), entoerobius vermicularis (n=12, 5.1%), entoerobius vermicularis plus impacted faecolith (n=1, 0.4%), and neuroendocrine tumour (n=1, 0.4%). Twenty four (10.2%) specimens were reported as being histologically normal. Male circumcision was the second most common procedure which was performed during the study period with 67 (15.5% of all procedures) in 2015 and 90 (16.5% of procedures) in 2016 (P= 0.67). In 2015, the ten procedures depicted in Table 2 accounted for 70.2% (n=304) of the 433 which were carried out that year. Similarly, the same ten procedures accounted for 70.9% (n=387) of the 546 which were performed the following year (P= 0.82). Eighty five different types of procedure were undertaken in 2015, compared to 73 in 2016.
Re-admission rates
Re-admissions were defined as an in-patient admission within 30 days of the initial admission. Eleven emergency re-admissions following surgery and 10 re-admissions following conservative management were recorded in 2015, giving an overall re-admission rate of 2.2%. Re-admissions following surgical management in 2015 were comprised of 8 wound complications and 3 surgical site infections. Re-admissions following conservative management in 2015 included 4 cases of abdominal pain that were re-admitted and underwent laparoscopy (3 out of 4 of these cases underwent an appendicectomy at the time of laparoscopy); 3 cases of abdominal pain that were re-admitted for conservative management only; 2 cases of testicular pain that were re-admitted for cyst of Morgani excision and intravenous treatment of epididymo-orchitis; and 2 cases of persistent vomiting following a head injury (both patients had a normal CT Brain). All re-admissions were for complications classified as Clavien-Dindo 1 or 23. A lower re-admission rate was observed in 2016 with 9 emergency re-admissions, 3 following surgical management and 6 following conservative management. This gave a 0.8% re-admission rate. Reasons for re-admissions in 2016 included 1 surgical site infection post toenail avulsion; 2 for non-specific abdominal pain post-laparoscopy; 1 hospital acquired lower respiratory tract infection following admission for non-specific abdominal pain; 3 for persistent non-specific abdominal pain following admissions with abdominal pain; 1 re-admission with persistent vomiting post head injury (normal CT Brain); and 1 with unrelated testicular pain following head injury.
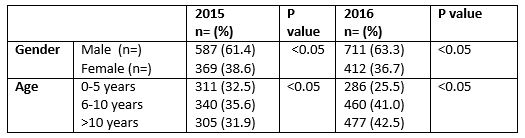 Table 1. Patient demographic details
Table 1. Patient demographic details
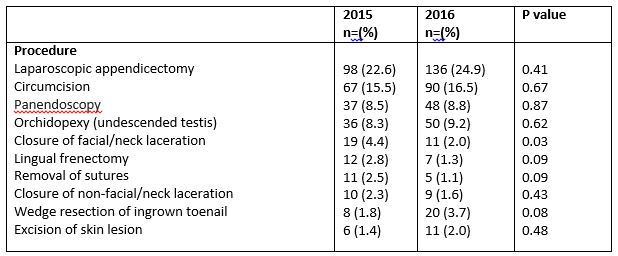 Table 2. Most commonly performed procedures across 2015 and 2016
Table 2. Most commonly performed procedures across 2015 and 2016
Discussion
This study was conducted following the 2016 publication of the National Clinical Programme for Paediatrics and Neonatology guidelines for hospitals providing a non-specialist paediatric surgical service1. Audit of services provided was highlighted as a key component of providing a general paediatric surgery service. Regular audit is crucial for training purposes and for the allocation of resources4. This regional facility provides an effective day case, elective and unscheduled paediatric general surgery service that is fully compliant with the guidelines. The Regional Hospital Mullingar provides 24-hour consultant delivered surgical and anaesthetic services, with an on-site paediatric medical ward with specialist nurses. This service is supported by appropriate consultant paediatric radiologist and paediatrician support. This unit runs one dedicated elective paediatric surgery list per week.
Our facility meets the standards outlined in the document mentioned surrounding provision of day case surgery. All surgical cases are undertaken by a surgeon with adequate experience in the relevant procedure. In addition to this, steps have been taken to ensure that there is always at least one a member of staff present who is trained in paediatric advanced life support. A 24-hour on site registrar call ensures the presence of a senior decision-maker throughout a child’s admission. There are clear guidelines for assistance, transfer and communication with tertiary referral centres if necessary. Pain management policies including take home analgesia are clearly documented. Although our service could facilitate the provision of surgical services to children less than 1 year of age, this unit does not routinely operate on children in this age group. This was a common finding by the National Clinical Programme when reviewing services across the country. Our facility does however routinely operate on children less than 2 years of age, a cut off shared by most units around the country.
The published guidelines concluded that the case bundle of operative procedures in most units is limited to appendicectomy, circumcision, herniotomy, orchidopexy, as well as lesion excision and abscess drainage1. Our study reflected these findings, with just 10 procedures accounting for 70.6% of procedures performed across two years. The low overall re-admission rates across the 2 year study period illustrates the safe, effective service that is provided by this regional hospital. High laparoscopic rate reflects the skillset of consultants specialised in adult general laparoscopic and luminal surgery.
Our service currently operates effectively and alleviates workload on tertiary, specialist paediatric surgery centres. Potential for improvement of the paediatric general surgical services is dependent on the future sustainability of the service. The inevitable retirement of surgeons with general paediatric surgical skills, the lack of mandatory paediatric surgical training for general surgery trainees and the growing trend towards sub-specialisation, mean that it will be difficult to replace our current service providers in regional hospitals. Inevitable centralisation of general paediatric surgery to tertiary centres will also lead to de-skilling of anaesthesia and nursing staff, further compounding this issue.
This study verifies that correctly staffed and resourced model III hospitals provide safe and effective paediatric general surgical services. They are a key component of the national service that should not be allowed to diminish. We conclude that formal teaching of surgical trainees around these core general paediatric surgical competencies would be possible with mandatory rotations through regional hospitals providing these services. This initial training could be supplemented with rotation through tertiary paediatric centres late in the training scheme for those interested in this subspecialty. This would have positive implications for the future of general paediatric surgery in Ireland, limiting the inevitable dependence on tertiary referral centres.
Conflicts of Interest Statement
The authors to not have any conflict of interest to declare.
Corresponding Author
Doireann Joyce,
Regional Hospital Mullingar,
Co. Westmeath
Email: [email protected]
References
1. Faculty of paediatrics RCPI, RCSI, HSE. National Clinical Programme for Paediatrics and Neonatology: improving services for general paediatric surgery. February 2016.
2. http://www.midlands103.com/wp-content/uploads/2017/07/Regional-Hospital-Mullingar-2016-.pdf
3. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336patients and results of a survey. Ann Surg. 2004 Aug;240(2):205-13.
4. Paton JY, Ranmal R, Dudley J; RCPCH Clinical Standards Committee. Arch Dis Child Educ Pract Ed. Clinical audit: still an important tool for improving healthcare. Arch Dis Child Educ Pract Ed. 2015 Apr;100(2):83-8. doi: 10.1136/archdischild-2013-305194. Epub 2014 Aug 13.
P896
