Surgical Parathyroidectomy Services
E. Burke1, A. Waris1, G. O’Donoghue1
1. Department of Breast and Endocrine Surgery, University Hospital Waterford.
Abstract
Aims
Retrospectively audit our experience with surgical parathyroidectomy over a 5 year period from the beginning of 2013 to June 2018.
Methods
Hospital In-patient Enquiry (HIPE) data, NIMIS radiology and theatre logs were used to identify the study cohort of a single specialist parathyroid surgeon. Demographic data plus pre and post-op calcium and parathyroid Hormone (PTH) levels were analysed. Data were coded and entered into SPSS 24 statistical software package for analysis.
Results
Thirty-one surgical parathyroidectomy cases were identified comprising four male and twenty seven females. Average age was 59.81 years (SD 14.75). The median pre-op and post-op calcium levels were 2.81[elevated] (Range 2.37-4.06 mmol/L) and 2.42[normal] (2.16-3.31 mmol/L) respectively and were statistically significant therapeutic reductions (p<0.05). The median pre-op and post-op PTH levels were 168.0[elevated] (Range 69-3171 pg/ml) and 41.7 [normal] (7.30-1628 pg/ml) respectively. All patients were discharged on post op day 1.
Conclusion
Parathyroidectomy is a safe and cost-effective treatment for PHPT in University Hospital Waterford.
Introduction
Primary hyperparathyroidism (PHPT) is a pathology characterised by the inappropriate secretion of parathyroid hormone from the parathyroid glands independent of the normal negative feedback inhibition[i]. The pathology in primary hyperparathyroidism is most commonly a single secretory adenoma followed by four gland hyperplasia and, least commonly, primary parathyroid carcinoma[ii].
PHPT is a relatively common endocrine disorder, with a prevalence estimated to be between one and seven cases per 1000 adults. It predominantly affects elderly populations and women two to three times as often as men[iii].
PHPT is believed to be the most common cause of hypercalcemia. The classic symptoms and signs of primary hyperparathyroidism, namely “renal stones, abdominal groans and psychic moans”, are rare today, but nephrolithiasis still occurs in 4 to 15% of cases[iv]. Symptomatic patients often present with vague initial symptoms including weakness, easy fatigability, anxiety, and cognitive impairment even when the level of serum calcium is modestly increased. Low bone mineral density occurs in more advanced stages and presents major issues such as pathological fractures. Similarly nephrolithiasis presents a major cause of morbidity and a frequent cause of recurrent admission in this patient group.
However currently the most common presentation for PHPT is asymptomatic hypercalcaemia detected on blood tests performed for another reason. In this setting an intact index parathyroid hormone (PTH) blood level should be sent to assess for PHTH.
Intervention, if surgically fit, with parathyroidectomy is the only definitive intervention for patients with symptomatic PHPT. Parathyroidectomy has been shown to cure the pathology, decrease the risk of nephrolithiasis, improve bone mineral density and decrease fracture risk[v]. The management of patients with asymptomatic PHPT is guided by the findings of the fourth international workshop on asymptomatic primary hyperparathyroidism with surgery being advocated should the patient meet any one of the criteria outlined in table 1[vi].
Table 1:
Candidates for surgery in asymptomatic primary hyperparathyroidism
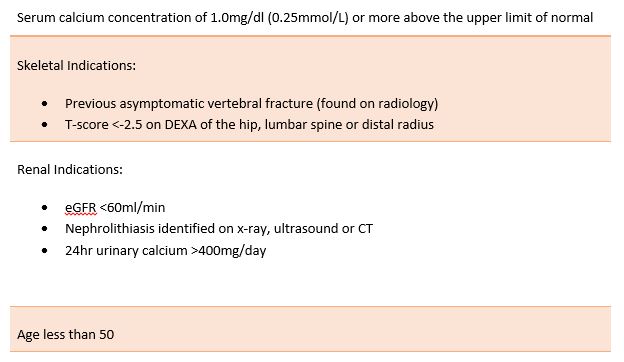
Fourth international workshop on asymptomatic primary hyperparathyroidism guidelines on selecting candidates for surgery. As per this workshop all symptomatic PHPT patients should be offered parathyroidectomy and any asymptomatic patients who meet any one of the above criteria may also be offered surgery. Asymptomatic patients who do not meet any of the above criteria may be offered surveillance, medical management or parathyroidectomy.
By undertaking this study we hope to highlight the effectiveness of parathyroidectomy in the management of PHPT in University Hospital Waterford and ultimately increase awareness amongst our colleagues in the community of the availability and success of the program.
Methods
We conducted a retrospective review of a prospectively maintained database of parathyroidectomies performed by a single specialist endocrine surgeon in University Hospital Waterford from January 2013 to June 2018. The hospital in-patient enquiry system (HIPE) and theatre logs were used to identify the study cohort of thirty one patients and collect demographic data. The national integrated medical imaging system (NIMIS) was interrogated to assess pre-operative imaging used to localise the pathology and the lab enquiry system to assess pre-operative and post-operative calcium and PTH levels for each patient. PTH was measured using a standard Elecsys 1010 analyzer with reference range being 10-65pg/ml in UHW. Similarly we used the lab enquiry system to assess the histology of the surgical pathology specimens for each patient.
Results
Thirty-one patients (comprising four male and twenty seven females) underwent parathyroidectomy for PHPT from January 2013 to June 2018 in University Hospital Waterford (fig.1).
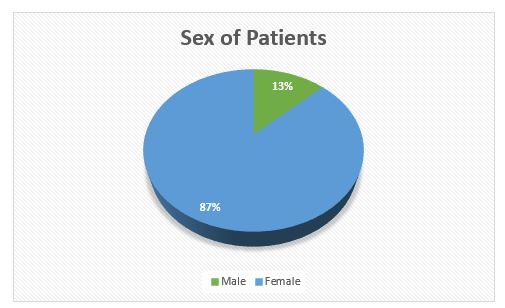
Fig.1 Sex of patients undergoing parathyroidectomy. Of the thirty one patients four were male and twenty seven were female with an average age of 59.8.
The average age was 59.81years (SD 14.75). Twenty-seven patients underwent ultrasound scanning by radiologist in UHW as part of workup. Nuclear Medicine Sestamibi scanning was performed in UHW on all patients to localize pathology. Based on this imaging there was a clear predilection of pathology to the inferior glands (27 out of 31 cases with the remainder in the superior glands) with right being more commonly affected than the left (18 of the 27 inferior glands and 3 of the 4 superior glands) with concordance between imaging modalities.
In all cases, surgery successfully identified a single parathyroid adenoma. The median pre-op and post-op calcium levels were 2.81[elevated] (Range 2.37-4.06 mmol/L) and 2.42 [normal] (Range 2.16-3.31 mmol/L) respectively and were statistically significant therapeutic reductions (p<0.05) (fig.2). Normal reference range: 2.2-2.7mmol/L.
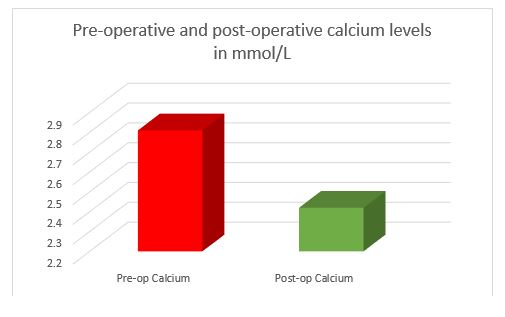
Fig.2 Pre-operative and post-operative calcium levels in mmol/L. The median pre-op and post-op calcium levels were 2.81 (Range 2.37-4.06) and 2.42(Range 2.16-3.31) mmol/L respectively and were statistically significant (p<0.05). Normal reference range: 2.2-2.7mmol/L.
The median pre-op and post-op PTH levels were 168.0 [elevated] (Range 69-3171 pg/ml) and 41.7 [normal] (Range 7.30-1628 pg/ml) respectively and were shown to be statistically significant therapeutic reductions (p<0.05) (fig.3). Normal reference range: 10-65pg/ml.
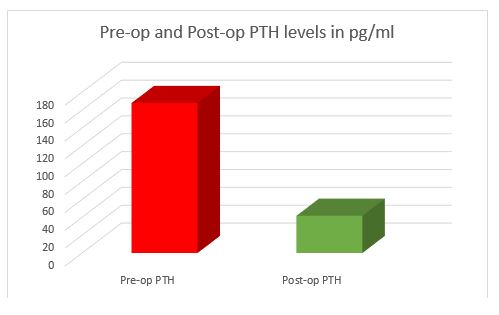
Fig.3 Pre-operative PTH and post-operative PTH levels in pg/ml. The median pre-op and post-op PTH levels were 168.0 (Range 69-3171 pg/ml) and 41.7 (Range 7.30-1628 pg/ml) respectively and were shown to be statistically significant (p<0.05). Normal reference range: 10-65pg/ml.
All patients were discharged on post op day one. Two patients suffered mild hypocalcaemia post op (2.18 and 2.16 mmol/L) which had resolved by 6 week follow up.
Discussion
PHPT is a common pathology with the potential for major morbidity if left untreated. Unlike other endocrine pathologies which are often chronic in nature and difficult to treat PHPT is potentially curable with parathyroidectomy.
In our study, we reinforced the finding that PHPT is more common in female patients (fig.1). By assessing pre-and post-operative calcium and PTH levels we were able to show that parathyroidectomy successfully decreased both biochemical parameters to within normal limits in the vast majority of patients. Two patients experienced mild hypocalcaemia post operatively (2.16 and 2.18mmol/L) which resolved. A single patient was found to have post-operative PTH of 1628pg/ml and post-operative calcium of 3.31mmol/L. Following CT scanning of the thorax this patient was found to have ectopic parathyroid tissue in the mediastinum and was referred for suitable treatment.
All patients were discharged home on the first post-operative day.
In summary, we have shown that parathyroidectomy is an effective treatment for PHPT and can be performed safely and cost effectively as a 24-hour procedure.
Alarmingly, however, Shapey et al, in their paper titled “Primary hyperparathyroidism: how many cases are being missed?”, found that 63% of patients with PHPT in Worcestershire in the UK remained untreated and without a referral to a specialist[vii]. They suggested a need for improvements in GP education and referral systems.
Our paper highlights the effectiveness of parathyroidectomy in the management of PHPT and will serve to increase awareness amongst our colleagues in the community of the need to refer patients with PHPT to a specialist promptly to avoid unnecessary morbidity and health care costs.
In conclusion parathyroidectomy is an effective surgical treatment for PHPT and all symptomatic patients or asymptomatic patients meeting criteria as outlined above should be referred promptly to an endocrinology and surgical specialist.
Conflict of Interest:
The authors report no conflict of interest.
Corresponding Author:
Eoghan Burke
Email: [email protected]
[i] Marcocci C, Cetani F “Primary Hyperparathyroidism”, New England Journal of Medicine 365;25
[ii] Ruda JM, Hollenbeak CS, Stack BC Jr ,”A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003” Otolaryngol Head Neck Surg. 2005;132(3):359.
[iii] C Marcocci, Gatti D, “Epidemiology of primary hyperparathyroidism in Europe”. J Bone Miner Res. 2002;17:N18–N2312412773”
[iv] Rejnmark L, Vestergaard P, Mosekilde L. “Nephrolithiasis and renal calcifications in primary hyperparathyroidism”. J Clin Endocrinol Metab 2011;96:2377-85.
[v] Silverberg S. “A 10-year prospective study of primary hyperparathyroidism with or without parathyroid surgery.” New England Journal of Medicine, Volume 341 Number 17
[vi] Bilezikian J. “Guidelines for the Management of Asymptomatic Primary Hyperparathyroidism: Summary Statement from the Fourth International Workshop”. J Clin Endocrinol Metab. 2014 Oct; 99(10): 3561–3569.
[vii] Shapey IM, Ann R “Primary hyperparathyroidism: how many cases are being missed?”, Coll Surg Engl 2011; 93: 294–296
P916
