Dedicated Orthogeriatric Service Saves the HSE a Million Euro
E Shanahan1, C Henderson1, A Butler2, B Lenehan2, T Sheehy3, A Costelloe3, S Carew3, C Peters1, M O’Connor1, D Lyons1, J Ryan1
Departments of 1Geriatric Medicine, 2Orthopaedics, and 3Clinical Age Assessment, University
Hospital Limerick, Dooradoyle, Co Limerick
Abstract
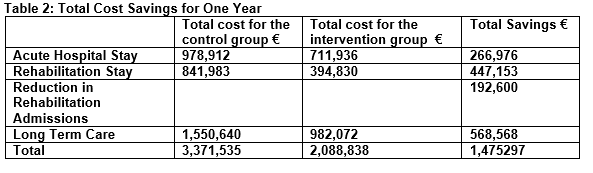
Hip fracture is common in older adults and is associated with high morbidity, mortality and significant health care costs. A pilot orthogeriatrics service was established in an acute hospital. We aimed to establish the cost effectiveness of this service. Length of hospital stay, discharge destination and rehabilitation requirements were analysed for a one year period and compared to patients who received usual care prior to the service. We calculated the costs incurred and savings produced by the orthogeriatric service. Median length of stay was reduced by 3 days (p=<0.001) saving €266,976. There was a 19% reduction in rehabilitation requirements saving €192,600. Median rehabilitation length of stay was reduced by 6.5 days saving €171,093. Reductions in long term care requirements led to savings of €10,934 per week. Costs to establish such a service amount to €171,564. The introduction of this service led to improved patient outcomes in a cost effective manner.
Introduction
In 2011, health care costs in Ireland amounted to almost fourteen billion euro or 27% of government expenditure. A ceiling of just over thirteen billion for health expenditure was set for 20141. Deliverance of high quality patient care in a cost effective manner has become of the upmost importance. This will become an even greater challenge as Ireland’s population continues to age. Eleven point-six percent of the population of Ireland, or 535,393 people, were aged 65 years or over in 20112. It is estimated that this figure will increase to up to 728,606 people, or 14.8% of the population, by 20213. Research has shown that older adults are greater users of in-patient services than their younger counterparts, with those aged over 80 years using 1.9 bed days per year compared to 0.5 bed days for those aged 50 to 54 years4. Hip fracture is the most common fracture occurring in older adults5. It is associated with increased mortality and a 25% reduction in life expectancy compared to age and gender matched controls6. The lifetime cost to health services is three times higher for patients post hip fracture than their aged matched counterparts7. Half of costs encountered relate to long term care facilities6. The annual cost of managing acute hip fracture patients in a single university hospital in Ireland in 2005 amounted to over €1.3 million for 143 patients treated. The mean cost for acute hospital stay per patient was €9,2368. These figures do not incorporate the additional costs of rehabilitation and admissions to long term care institutions. A multidisciplinary management approach with orthogeriatric input has been shown to reduce hospital length of stay9, and the number of admission to long term care10, thereby reducing the cost associated with management of hip fractures. A pilot orthogeriatric service was established in University Hospital Limerick in July 2011 to ascertain if such a service would improve patient outcomes and reduce costs associated with managing patients with fractured neck of femur in a hospital in which such a service did not previously exist. University Hospital Limerick is a university teaching hospital with a catchment population of 379,327 people in 2011; 47,254 of whom were aged over 65 years2.
Methods
A pilot orthogeriatic liaison service was established in University Hospital Limerick in July 2011 as a collaboration project between the geriatric and orthopaedic departments. All patients admitted with a fractured neck of femur were assessed in the perioperative period by a geriatrics research fellow with consultant geriatrician support. Patients received a geriatric assessment which included optimization of medical condition, bone health and falls assessment. Patients were offered follow-up in a dedicated fracture liaison secondary prevention clinic. All patients seen by the service for the one year period beginning July 2011 were included in the intervention group. A comparative control group was selected from the National Hip Fracture Database and comprised patients admitted to the same hospital with fractured neck of femur in the one year period beginning July 2009. This allowed a one year washout period, during which time discussion regarding the pilot service were ongoing and changes in practices may have occurred as a result. Systematic sampling was used to ensure an equal number of patients in both groups.
Patient data was collected prospectively on a newly developed orthogeriatric database using Filemaker Pro 12 (FileMaker Inc.). Hospital length of stay, number of patients requiring rehabilitation, rehabilitation length of stay and discharge rates to long term care were recorded and used as a means of comparing the two groups. The cost per bed day was obtained from the accounts department of University Hospital Limerick. The cost per day of rehabilitation was obtained from the management of Older Person’s Residential Services Mid-West. Nursing home costs were based on nationally available figures11. Statistical analyses were performed using IBM Statistical Product and Service Solutions (SPSS) Version 20. Age, length of hospital stay and length of rehabilitation stay were not normally distributed. Therefore, non-parametric tests were used including median, minimum (min), maximum (max) and interquartile range (IQR). Medians were compared using the Mann-Whitney U test. A Chi-square test was used to compare the proportion of patients discharged to long term care. Prior to commencement of the study ethical approval was obtained from University Hospital Limerick’s Research Ethics Committee.
Results
There were 206 patients in the intervention group with a median age of 81 years (min=53, max=100, IQR=14). Seventy-three percent (150 patients) were female. The control group consisted of 206 patients selected using systematic sampling from the 248 patients with fractured neck of femur admitted the year beginning July 2009. The median age of this group was 81.5 years (min=43, max=96, IQR=11). 66% (136 patients) were female.
Hospital Length of Stay
The median length of stay in the acute hospital was reduced from 11 days (min=2, max=54, IQR=11) in the control group to 8 days (min=2, max=72, IQR=7) in the intervention group (p=<0.001). The average cost of a bed day on the trauma ward in University Hospital Limerick is €432. The 3 day reduction in length of stay thereby amounts to a cost saving of €1,296 per patient, or €266,976 for the 206 patients over the year.
Rehabilitation
One hundred and twenty-two patients in the control group (59%) were referred for rehabilitation. In the intervention group 82 patients (40%) required rehabilitation. This is a 19% reduction in patients requiring rehabilitation (z=3.94, p<0.01). The median length of stay in the second year was 15 days and the cost per bed day is €321, thus the reduction in rehabilitation admissions saved €192,600. In addition the median length of stay for those requiring rehabilitation was reduced from 21.5 days (min=9, max=132, IQR=14) in the control group to 15 days (min=8, max=103, IQR=8) in the intervention group (p=0.05). This 6.5 day reduction in length of stay provides a further saving of €2086.50 per person or €171,093 in total for the 82 patients in the intervention group who required rehabilitation.
Long Term Care
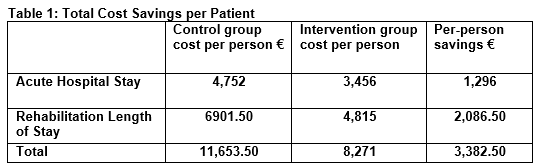
166 patients (80.6%) from the control group were residing at home prior to admission with the fracture. Of these, 109 patients (65.7%) were discharged home and 30 patients (18%) were admitted to a long term care facility following discharge from hospital. In the intervention group an equal number of patients were residing at home prior to hospital admission. Of these, 138 patients (83.1%) were discharged home and 19 patients (11%) were admitted to long term care following discharge from hospital. Therefore 11 less patients were admitted to long term care from the intervention group compared to the control group (p=0.03). With an average cost per person of a week of care in a nursing home of €99411 this provides a saving of €10,934 per week or €568,568 in one year. Within both groups, all patients admitted from long term care who survived to discharge were discharged back to long term care. Table 1 shows a summary of the total cost savings per patient while Table 2 shows the total savings to the health service over a one year period.
Discussion
Fractured neck of femur is a condition associated with high morbidity and mortality rates12,13. It adds significant cost to the health service7. Orthogeriatric services have previously been shown to improve patient outcomes post hip fracture. One and three month mortality rates are significantly lower for patients treated by an orthogeriatric service than those receiving standard orthopaedic treatment alone14. Patients admitted post fractured neck femur have reduced hospital stay and reduced rated of discharge to long term care when a multi-disciplinary approach is taken to their care15-17. Given recent reductions in health budgets, it is essential that these improvements in patient outcomes continue to be achieved, while at the same time allowing care to be coordinated in a cost-effective manner. The reduction in length of hospital stay achieved by our pilot orthogeriatric service reduced bed day costs by €266,976. This saving should to be offset by the cost of running the service. The pilot service was run by a geriatric research fellow, the average salary of whom would have been €73,079. Secretarial support was provided by pre-existing staff and was estimated to provide a quarter of a whole time equivalent to the service, with an average cost of €6,325. Employer Pay Related Social Insurance (PRSI) of 10.75% for both would cost €8,534. The pilot service therefore required funding of €87,938 but in doing so saved the acute hospital €179,038 for the twelve month period.
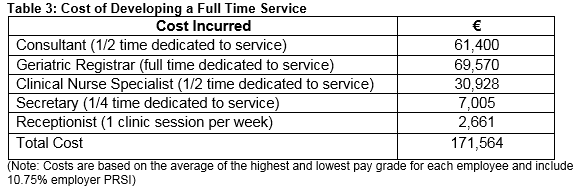
However, the costs above are based on the pilot study only, and are not an adequate reflection of the cost that would be required to develop a full time service. The service input that we estimate to be required are shown in Table 3 along with the associated cost. The estimated cost amounts to €171,564, which still leaves an annual saving of €95,412 to the acute hospital. Consideration was given to loss of insurance revenue associated with the reduction in length of hospital stay. However, following review of this income with the finance department it was felt that the revenue from this population was negligible and was therefore not considered in our calculations. In additional to savings to the acute hospital, the pilot service provided additional savings to the health service as a whole. The reduction in both the number of patients requiring rehabilitation and the length of stay in rehabilitation provided a saving of €363,693. The reduction in long term care requirements provides a weekly saving of €10,934. If all patients were to remain in long term care for a period of two years this would cut nursing home costs by over a million euro. These are savings to the health service without the requirement of any additional resources. The argument therefore arises as to whether some of these savings should be reallocated into the acute hospital sector to further develop a service which has been shown to improve patient outcomes in a cost effective manner.
Correspondence:
Elaine Shanahan
Departments of Geriatric Medicine, University Hospital Limerick, Dooradoyle, Co Limerick
Email: [email protected]
References:
1. Expenditure DoPRa. Comprehensive Expenditure Report 2012-2014. 2012.
Office CS. Profile 2 Older and Younger – An Age Profile of Ireland. 2012.
Connell P PDNCoAaOP. http://www.nuim.ie/staff/dpringle/ncaop-report.pdf. 2004.
2. Aoife McNamara CN, Brendan Whelan. Patterns and Determinants of Health Care Utilisation in Ireland; The Irish Longitional Study on Aging (TILDA). 2013.
3. Commings SR RS, Black D. The future of hip fractures in the United States. Numbers costs and potential effects of postmenopausal estrogen. Clin Orthop. 1990;252:163-6.
4. Braithwaite RS, Col NF, Wong JB. Estimating hip fracture morbidity, mortality and costs. Journal of the American Geriatrics Society. 2003 Mar;51:364-70.
5. Haentjens P LG, Boonen S. Costs and consequences of hip fracture occurrence in old age: an economic perspective. Disability and Rehabilation. 2005;27:1129-41. Epub Sept.
6. Azhar A, Lim C, Kelly E, O’Rourke K, Dudeney S, Hurson B, Quinlan, W, Cost induced by hip fractures. Irish medical journal. 2008 Jul-Aug;101:213-5.
7. González-Montalvo JI, Alarcón T, Mauleón JL, Gil-Garay E, Gotor P, Martín-Vega A. The orthogeriatric unit for acute patients: a new model of care that improves efficiency in the management of patients with hip fracture. Hip international : the journal of clinical and experimental research on hip pathology and therapy. 2010 /;20:229-35.
8. Halbert J, Crotty M, Whitehead C, Cameron I, Kurrle S, Graham S, Handoll H, Finnegan T, Jones T, Foley A, Shanahan M; Hip Fracture Rehabilitation Trial Collaborative Group. Multi-disciplinary rehabilitation after hip fracture is associated with improved outcome: A systematic review. Journal of rehabilitation medicine : official journal of the UEMS European Board of Physical and Rehabilitation Medicine. 2007 Sep;39:507-12.
9. McEnery B. Nursing Home Cost of Care ; A Fair Price – Ireland HSE Open Access Publishing: 2007.
Dzupa V, Bartonicek J, Skala-Rosenbaum J, Prikazsky V. [Mortality in patients with proximal femoral fractures during the first year after the injury]. Acta chirurgiae orthopaedicae et traumatologiae Cechoslovaca. 2002;69:39-44.
10. Hannan EL, Magaziner J, Wang JJ, Eastwood EA, Silberzweig SB, Gilbert M, Morrison RS, McLaughlin MA, Orosz GM, Sui AL, . Mortality and locomotion 6 months after hospitalization for hip fracture: Risk factors and risk-adjusted hospital outcomes. JAMA. 2001;285:2736-42.
11. Adunsky A, Lerner-Geva L, Blumstein T, Boyko V, Mizrahi E, Arad M. Improved survival of hip fracture patients treated within a comprehensive geriatric hip fracture unit, compared with standard of care treatment. Journal of the American Medical Directors Association. 2011 Jul;12:439-44.
12. Elliot JR1, Wilkinson TJ, Hanger HC, Gilchrist NL, Sainsbury R, Shamy S, Rothwell A. The added effectiveness of early geriatrician involvement on acute orthopaedic wards to orthogeriatric rehabilitation. The New Zealand medical journal. 1996 03/;109:72-3.
13. Street PR, Hill T, Gray LC. Report of first year’s operation of an ortho-geriatric service. Australian health review : a publication of the Australian Hospital Association. 1994;17:61-74.
14. Kauh B, Polak T, Hazelett S, Hua K, Allen K. A pilot study: post-acute geriatric rehabilitation versus usual care in skilled nursing facilities. Journal of the American Medical Directors Association. 2005 Sep-Oct;6:321-6.
P385