Dysphagia in the Elderly Following Anterior Cervical Surgery: A Multidisciplinary Approach
C N. Osuafor1, B Greene2, N El-Kininy1, C Donegan1
1Geriatric and General Medicine Department, Beaumont Hospital, Dublin, Ireland.
2Speech and Language Department, Beaumont Hospital, Dublin, Ireland.
Abstract
Dysphagia is a risk factor for adverse health outcomes like aspiration, recurrent chest infections and malnutrition. Here, we describe a case of an 82-year-old lady who presented with a two-month history of dysphagia after an anterior odontoid screw fixation for a type II odontoid process fracture. This case highlights the importance of a multidisciplinary approach to patient care.
Introduction
Dysphagia in the elderly may be caused by disease entities associated with either oropharyngeal or oesophageal dysfunction. Swallowing can also be disrupted by encroachment from within or outside (mechanical dysphagia) the oropharyngoesophageal conduit1. Identifying the distinctions between mechanical, oropharyngeal or oesophageal dysphagia is both important in relation to aetiology and key in management1.
Case Report
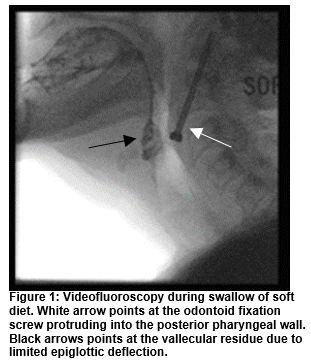
An 82-year-old lady presented to our service with a two-month history of dysphagia to solids, dry retching, and unintentional weight loss of about 6 kg. The patient reported intermittent choking episodes on large tablets and a sensation of pharyngeal residue during and after meals. She denied odynophagia. Laryngoscopy and oesophago-gastro-duodenoscopy showed no significant deficits. A clinical bedside assessment carried out by Speech and Language Therapy (SLT) found no overt signs of penetration or aspiration on oral intake and a mildly dysphonic vocal quality. A Fibreoptic Endoscopic Evaluation of the Swallow (FEES) was carried out which showed a bulge in the posterior pharyngeal wall. The epiglottis was noted to meet the posterior pharyngeal wall at times at rest. Severe vallecular residue and mild airway penetration were observed on all diet consistencies. A Videofluoroscopy (Figure 1) completed to support the findings of the FEES, visualised an odontoid screw which was protruding into the posterior pharyngeal wall at the level of the fourth cervical vertebrae. The protrusion resulted in limited epiglottic deflection and therefore reduced airway protection. The 4.6cm odontoid screw had been inserted anteriorly by Neurosurgery two months earlier for an odontoid process fracture type II secondary to a fall. The patient had been self-modifying her diet and was provided with further information from the SLT regarding diet consistencies which were easiest and safest to swallow. The patient was also referred to a dietician during this admission. Her care was then referred for assessment to neurosurgery. Five weeks later, she had the odontoid screw removed. The patient’s ability to tolerate her normal diet subsequently improved. One month after the removal of the odontoid screw, she reported no symptoms on reassessment of swallow and had started to regain weight.
Discussion
Dysphagia after anterior cervical surgery is a relatively common occurrence ranging from 30% to 50% in the early postoperative period. This is felt to be a transient finding with the vast majority of cases resolving within three months2. Vasudevan et al reported gastrostomy tube placement due to patient failing swallow evaluation in 13 of 30 consecutive elderly patients with type II odontoid fractures treated with anterior odontoid screw fixation3. Patients during this period are at risk of aspiration, recurrent chest infections and malnutrition and hence, adverse health outcomes.
Videofluoroscopy or modified barium swallow has been considered the instrumental examination of choice in the study of swallowing, in addition to clinical history and bedside assessment. It plays a relevant role in diagnosis and monitoring of rehabilitation treatment for dysphagia, either by means of ascertaining the efficacy of dietary modifications, such as restricted-consistency diet, and/or of the compensatory postural manoeuvres. It has the advantage of the possibility to see the recorded images again immediately, even while the examination is still being performed4. FEES was also very important in the management of this case.
Dysphagia evaluation and management are usually a multidisciplinary team approach and are based on careful history, differentiation of an oropharyngeal dysphagia from oesophageal dysphagia and identifying the underlying cause1. Regarding behavioural management and therapy, speech-language therapists play a central role in the management of these patients; no single strategy is appropriate for all elderly patients with dysphagia5. Our patient required neurosurgical intervention and had a successful outcome after the odontoid screw removal. At follow up, the patient’s dysphagia had resolved and an improvement in weight with dietary advice was noted.
Conflict of Interest
The authors declare no conflicts of interest
Correspondence
Christopher N. Osuafor
Geriatric and General Medicine Department, Beaumont Hospital, Dublin, Ireland.
Email: [email protected]
References
1. Aslam M, Vaezi MF. Dysphagia in the elderly. Gastroenterol Hepatol (N Y). 2013 Dec;9(12):784-95.
2. Rihn JA, Kane J, Albert TJ, Vaccaro AR, Hilibrand AS. What is the incidence and severity of dysphagia after anterior cervical surgery? Clin Orthop Relat Res. 2011 Mar;469(3):658-65.
3. Vasudevan K, Grossberg JA, Spader HS, Torabi R, Oyelese AA. Age increases the risk of immediate postoperative dysphagia and pneumonia after odontoid screw fixation. Clin Neurol Neurosurg. 2014 Nov;126:185-9.
4. Rugiu MG. Role of videofluoroscopy in evaluation of neurologic dysphagia. Acta Otorhinolaryngol Ital. 2007 Dec;27(6):306-16.
5. Sura L, Madhavan A, Carnaby G, Crary MA. Dysphagia in the elderly: management and nutritional considerations. Clin Interv Aging. 2012;7:287-98.
(P657)