Peripherally Inserted Central Catheters (PICCs) and Potential Cost Savings and Shortened Bed Stays In an Acute Hospital Setting.
C O’Brien, J Mc Marrow, E O’Dwyer, P Govender, WC Torreggiani
Department of Radiology, Tallaght Hospital and Trinity College, Dublin 24
Abstract
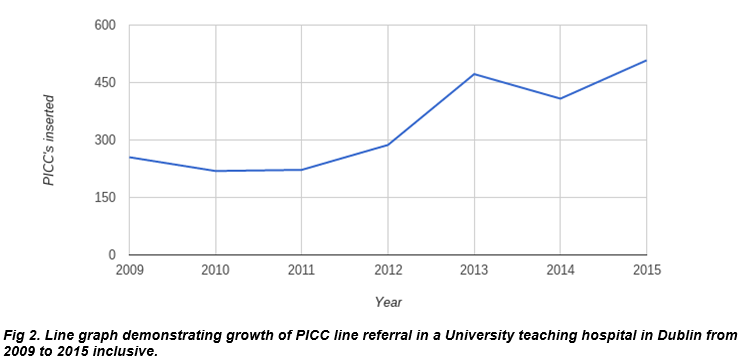
Peripheral inserted central catheters (PICCs) have increasingly become the mainstay of patients requiring prolonged treatment with antibiotics, transfusions, oncologic IV therapy and total parental nutrition. They may also be used in delivering a number of other medications to patients. In recent years, bed occupancy rates have become hugely pressurized in many hospitals and any potential solutions to free up beds is welcome. Recent introductions of doctor or nurse led intravenous (IV) outpatient based treatment teams has been having a direct effect on early discharge of patients and in some cases avoiding admission completely. The ability to deliver outpatient intravenous treatment is facilitated by the placement of PICCs allowing safe and targeted treatment of patients over a prolonged period of time. We carried out a retrospective study of 2,404 patients referred for PICCs from 2009 to 2015 in a university teaching hospital. There was an exponential increase in the number of PICCs requested from 2011 to 2015 with a 64% increase from 2012 to 2013. The clear increase in demand for PICCs in our institution is directly linked to the advent of outpatient intravenous antibiotic services. In this paper, we assess the impact that the use of PICCs combined with intravenous outpatient treatment may have on cost and hospital bed demand. We advocate that a more widespread implementation of this service throughout Ireland may result in significant cost savings as well as decreasing the number of patients on hospital trollies.
Introduction
In the past year we have seen the hospital bed crisis in Ireland escalate to new heights with a reported >600 patients on trolleys awaiting admission to a ward. National newspaper headlines have included: HSE - ‘more than €100million needed to tackle trolley crisis’1, “A&E overcrowding may get worse, HSE admits”2 and “Hospital crisis is killing our patients, says A&E boss”3. This issue is again dominating the media this month and the issues being discussed have not changed. There has been a shift towards delivering IV treatment in an outpatient setting when appropriate and safe for patients, outpatient parenteral antimicrobial therapy (OPAT) and ambulatory parenteral therapies have facilitated this movement. This facility decreases the number of patients occupying hospital beds for the delivery of intravenous treatment. A number of patients are deemed suitable for IV therapy in an outpatient setting after a complete medical assessment.
Recently there has been an increasing shift toward outpatient doctor and nurse led IV treatment schemes for some of this cohort of patients e.g. OPAT. The patients medically worked up, deemed fit for discharge and enrolled in an outpatient IV treatment scheme with regular follow-up in a physician led outpatient clinic. Prior to discharge in our centre these patients are referred to interventional radiology for a peripherally inserted central venous catheters to establish safe and reliable intravenous access.
PICCs have become a mainstay in the treatment of patients requiring prolonged IV antibiotics, chemotherapy and parental nutrition. The first central venous line was performed in 1929 by a German surgical intern – Werner Forssmann, under local anesthetic he cannulated his own right atrium via his right cephalic vein4. In 1952 Sven-Iver Seldinger developed the technique of placing catheters into lumens and body cavities that revolutionized medicine and is the principle for placing PICCs and central venous catheters (CVCs) used today4. PICCs are traditionally placed by Interventional Radiology in a peripheral vein at the inner aspect of the elbow (antecubital fossa) and travel along the venous network of the arm into the axillary vein, subclavian vein and terminating in the superior vena cava4. With the advent of a new doctor or nurse led outpatient IV treatment program PICCs are in greater demand.
We carried out a retrospective study to examine the increasing demand for PICCs in a university teaching hospital. We demonstrated a twofold increase in the number of referrals for PICCs over a 7 year period (2009-2015); this is mostly attributable to the new outpatient IV treatment strategy. With the current crisis for hospital beds in Ireland we hypothesize that increasing the number of medically stable patients enrolled in these outpatient IV treatment programs could help decrease the number of inpatient admissions and reduce the length of hospital stays. PICCs are a cost effective method of achieving stable IV access when compared to peripheral IV cannulas.
Methods
Radiologically-inserted peripherally inserted central venous catheters procedures are performed in the Interventional Radiology (IR) suite using ultrasound and fluoroscopic guidance under aseptic technique. The preferred vein for PICC line insertion is the basilic followed by the cephalic then brachial vein which is identified with ultrasound. A Chlorhexidine gluconate two percent w/v and isopropyl alcohol 70% v/v solution is used to clean the skin overlying the preferred vein. Local anaesthetic was infiltrated in skin, subcutaneous tissue and around the vein. A 21 gauge introducer needle is advanced into the vein under ultrasound guidance. A 0.018 inch guidewire is advanced through the introducer needle into vein and manipulated into the right atrium. The introducer needle is exchanged for a 7 French peel away sheath over the guidewire. The guidewire is used to measure the length up to the cavo-atrial junction and the PICC line is subsequently shortened to the same length. The PICC line is advanced through the peel-away sheath over the guidewire up to the cavo-atrial junction. It is secured in place with a stat-lock device and a biopatch dressing is placed around the PICC line at the dermatotomy. A Clear dressing (IV 300) is placed over the PICC line.
There are many practical benefits of radiologically-inserted PICC line, particularly with increased need for long-term venous access and increasing central vein thrombosis. Venous access is easier with ultrasound guidance and fluoroscopy allows for the correct length of PICC to be placed to optimise flow through the PICC. Limitations to PICC line placement like venous spasm or stenoses can be identified at time of PICC placement and alternate sites for PICC line placement can be used. Line sepsis is a major concern so radiologically-inserted PICC lines are placed in a sterile environment in an angiography suite. We carried out a retrospective study of all PICC insertions in our IR suite from January 2009 to December 2015. We calculated the number of PICC insertions per year and documented the referring physician. The patient age, location and date of procedure were also documented. Discussion with the clinical services revealed the timing and referral pathway for outpatient IV treatment implementation.
Results
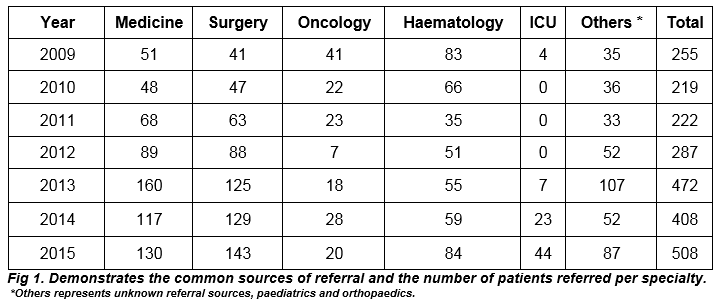
We carried out a retrospective study of 2,404 patients referred for PICC insertion from 2009 to 2015 in a university teaching hospital in Dublin (Fig 1). The mean age at referral was ~49.5 years with an age range of 6 weeks to 96 years. We analyzed the referral sources to our department and demonstrated that the largest source of referrals were from the inpatient population. The Haematology and Oncology services referred outpatients from their respective day wards. The most common indication was for prolonged IV antibiotic therapy followed by oncologic IV therapy and total parenteral nutrition. Patients referred from the intensive care required increased vascular access to facilitate increasing infusion and access demands.
The audit demonstrated an increase in the number of PICCs requested and inserted from 2011 to 2015 with a 64% increase from 2012 to 2013 as demonstrated by the line graph (Fig 2). The increased demand is attributed to the introduction of OPAT and ambulatory parenteral treatment to our institution. The increase in medical referrals is particularly attributable to the outpatient led IV treatment programs. The increase in demand for PICCs in the latter years of the study has had a minor impact on waiting times from referral to procedure. A same day service is not always feasible however, on review of the data the average waiting time from referral to completion of procedure is 48 hours.
The technical success rate of the PICC insertion in our institution was 99%. The one percent failure rate is secondary to patient factors such as significant venous stenosis and need for central vascular access.
Discussion
OPAT (Outpatient Parenteral Antimicrobial Therapy) is operational in many institutions around the country, in some cases patients require private medical insurance for enrolment. L Glackin carried out a retrospective study over three years in a tertiary referral children’s hospital that demonstrated an institutional, organizational and patient benefit to outpatient IV antibiotic treatment5. The Infectious disease society of Ireland (IDSI) OPAT working group have demonstrated significant patient benefits, financial benefits and organizational benefits of OPAT since its advent in Ireland.
PICCs are a safe method of vascular access for patients who require long term IV treatment in the community, with appropriate training and management in infection control PICCs can be managed in the community by specialist OPAT and outpatient IV trained nurses6. There are several known complications associated with PICCs including: phlebitis, central thrombosis, catheter fracture or embolization and infection however, these complications are infrequent. In a study of 322 PICCs over 2,506 days complication rates were described as: Infection- 0.6%, phlebitis – 9.7%, central vein thrombosis 0.3%, catheter embolization 0 % and catheter fracture - 9.6%3. PICCs have proven to be cost effective and associated with fewer complications compared to tunnelled central venous catheters (CVC) or implanted vascular ports (Port-A-Cath)1. Complications arising from a CVC or Port-A-Cath include: pneumothorax, haemothorax, hydrothorax and tracheal puncture. The reported cost to treat a haemothorax secondary to central line insertion was estimated to be $8,300; the treatment of the PICC induced complications are significantly less4.
PICCs offer a safe and cost effective alternative to peripheral IV access requiring frequent replacement and discomfort for patients; they are a cost effective method to aid the delivery of IV treatment in an outpatient setting. In the case report below we provide an example of the benefits described. We present the case of a 67 year old female who attended the emergency department with nausea and vomiting. The patient has a background medical history of chronic renal disease and hypertension. On admission her temperature of 38.60, she was hypotensive with a BP of 83/34 and had a tachycardia of 122 beats per minute. The patient was referred to the medical on-call service and admitted under their care. Clinical, hematological and biochemical evaluation diagnosed a cytomegalovirus (CMV) viremia. Her viral load was 217,700 at the time of diagnosis. The patient was commenced on IV ganciclovir.
Seven days into her treatment she had improved clinically, she was afebrile and her observations returned to normal. The medical service decided she was fit discharge despite requiring 14 days of ongoing IV treatment. She was enrolled in the ambulatory IV scheme. On day 7 of her admission she attended IR for PICC insertion, the procedure was uncomplicated. She received two weeks of outpatient IV therapy, was reviewed weekly in the medical outpatient clinic with bi-weekly blood tests. She made a full recovery at home and the PICC was removed with the cessation of IV treatment. This case illustrates the potential patient and hospital benefits outpatient therapy with PICC insertion can provide: The patient is treated at home with less exposure to hospital acquired infection and the demand for hospital beds is less with an associated cost saving benefit to outpatient treatment.
The IDSI have documented statistics proving that OPAT is a safe and viable option to facilitate prompt and safe discharge of patients for IV treatment in the community. The increased demand for PICC insertion in our Interventional Department secondary to OPAT and ambulatory outpatient treatment referrals demonstrates a cohesive multidisciplinary service and a willingness to facilitate outpatient IV treatment. The hospital bed crisis in Ireland this winter reached an all-time high and is likely to recur in 2018, enrolment in OPAT post PICC insertion is a viable option to alleviate some of the pressure that Irish hospitals will face in the future months.
Conflict of interest:
There is no conflict of interest.
Correspondence:
Ciara O Brien, Department of Radiology, Tallaght Hospital and Trinity College, Dublin 24
Email: [email protected]
References
(1) Martin Wall and Carl O’Brien, HSE needs ‘more than €100m’ to tackle trolley crisis.
The Irish times, news, social affairs 2015, Mar 2.
(2) Martin Wall, Harry McGee, Aine McMahon, A&E overcrowding may get worse, HSE admits
Consultants warn patients will die without steps to relieve crowded hospital units.The Irish Times, news, health 2015, Jan 7.
(3) Eilish O’Regan, Hospital crisis is killing our patients, says A&E boss Hospitals across the country continued to buckle. Independant.ie, news, health – 2015, Jan 7.
(4) Michael P Young, MD. Complications of central venous catheters and their prevention. Up To Date, 04/10/16.
(5) Glackin L, Flanagan F, Healy F, Slattery DM. Outpatient parenteral antimicrobial therapy: A report of three years experience. Ir Med 2014 AprJ
(6) E. G. Muldoon, G. M. Allison, D. Gallagher, D. R. Snydman, and C. Bergin. Out-patient Parenteral Antimicrobial Therapy in Ireland: Practice Standards. Infectious Diseases Society of Ireland (IDSI) OPAT Working Group. Eur J Clin Microbiol Infect Dis. PMC 2014 Apr 2.
(7) Ms Meinir Elen Hughes, PICC related thrombosis: Pathophysiology, incidence, morbidity and the effect of ultrasound-guided placement technique on occurrence in cancer patients. JAVE 2011, VOL 16 No 1.
(8) John Davis. PICC line insertions cost effectiveness and outcomes associated with independent PICC service. JAVA 2014 Vol 9 No 2.
(9) Stephen C Loughran and Marcello Borzatta Peripherally inserted central catheters: A report of 2506 catheter days. JPEN 1995 Vol 19 No 2.
P670