The Utility of Dopamine Transporter Scans for Diagnosing Parkinsonian Disorders.
GF Crotty1, OA O’Corragain1, C Bogue2, J Crotty3, S S O’Sullivan1,4
1 Department of Neurology, Cork University Hospital, Cork, Ireland.
2 Department of Radiology, Cork University Hospital, Cork, Ireland.
3 Department of Radiology, University Hospital Limerick, Limerick, Ireland
4 Department of Neurology, Bon Secours Hospital, Cork, Ireland
Abstract
Introduction
Dopamine transporter scans are increasingly being used in the diagnosis of clinically undefined Parkinsonism.
Aims
To assess the indications for imaging usage and its impact on future clinical management.
Methods
Retrospective review of scans ordered and their corresponding results over a five-year period. A chart review was carried out on a cohort of scans to assess changes in clinical management.
Results
One hundred and eighty scans (69% of total) were reported as showing evidence of dopaminergic deficit. A chart review in 81 patients showed a change in clinical management in 53 patients (65%). Scans were ordered inappropriately in 34 patients (13%).
Discussion
123I-FP-CIT SPECT scans are being more frequently ordered and if used correctly can alter clinical management. Increased education on indications for use is required to reduce waste of resources and risk to patients.
Introduction
Parkinson disease (PD) is the second most common neurodegenerative disease and is characterised by the presence of bradykinesia plus one of rigidity, tremor, or postural instability1. Misdiagnosis rates from 10 to 50% have been found using clinical exam alone, when compared to the gold standard pathological diagnosis2-4. The most common PD mimics include tremor disorders, drug-induced Parkinsonism, vascular Parkinsonism and Parkinson plus conditions. The prognosis and management of each disorder differs significantly from PD, and from each other. Therefore, the ability to distinguish between different parkinsonian entities is of clinical importance, allowing for optimal treatment and avoiding unnecessary therapeutic trials or other tests.
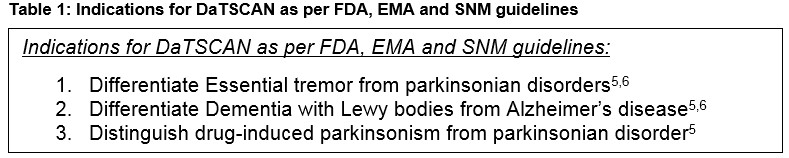
In-vivo functional imaging of dopamine transporters (DAT) can improve diagnostic accuracy in atypical cases of Parkinsonism. DaTSCAN, which is the trade name for striatal presynaptic dopamine transporter imaging using 123I-FP-CIT [(123)I-N-omega-fluoropropyl-2beta-carbomethoxy-3beta-nortropane] Single Photon Emission Computed Tomography [SPECT], has been licensed by the European Medicines Agency (EMA), The Society of Nuclear Medicine (SNM) and the US Food and Drug Administration (FDA) for certain indications (figure 1)5,6. Reductions in 123I-FP-CIT SPECT striatal uptake is demonstrated to have 95% sensitivity and 95% specificity with a high positive predictive value for identifying parkinsonian syndromes (PS)6. 123I-FP-CIT SPECT initial imaging results have been remarkably consistent with the clinical diagnoses made at three years follow-up4,7. Almost 100% concordance has been found between neuroradiologists on interpreting this imaging4,8. The PS which include PD, Multiple system Atrophy (MSA), Progressive supranuclear palsy (PSP) and Corticobasal degeneration (CBD) show nigrostriatal degeneration on DAT neuroimaging. Other conditions, such as essential or (ET), drug-induced Parkinsonism (DIP), vascular parkinsonism (VP), psychogenic parkinsonism, normal aging, normal pressure hydrocephalus and dystonic tremor may demonstrate features of parkinsonism, but do not have nigrostriatal degeneration on neuroimaging6. In the appropriate clinical setting (such as where the differential diagnoses being queried include a neurodegenerative Parkinsonism versus another mimic disorder), 123I-FP-CIT SPECT can be a very useful investigation. However, as each scan costs approximately €1,200 per patient, this is a resource that should not be used routinely.
Our primary aim was to evaluate the current use of 123I-FP-CIT SPECT in our health service as a diagnostic biomarker for parkinsonian syndromes. We reported on the indications for ordering 123I-FP-CIT SPECT along with assessing trends of referral by different specialties. We investigated for correlations between dopaminergic deficit on imaging and demographics or symptomatology. We identified inappropriate referrals and assessed the impact of these scans on subsequent clinical management.
Methods
Study design: A retrospective review of 123I-FP-CIT SPECT request forms and their corresponding results over a five-year period from 2008-2013 in two tertiary care hospitals, Cork University Hospital [CUH], Cork, Ireland and University Hospital Limerick [UHL], Limerick, Ireland. Patients in two tertiary care hospitals who underwent 123I-FP-CIT SPECT over this five-year period were included in the study. No additional exclusion or inclusion criteria were applied. Scans were carried out as per each institution’s protocol and in accordance with international guidelines. Patients were instructed to discontinue all potential confounding medications prior to scan. All scans were read by experienced radiologists who were aware of clinical history and differential diagnoses as documented on referral. Demographics including gender, age at scan, symptoms, medications and scan report details including indication for DaTSCAN, referring specialty and institution were manually gathered. Inappropriate referrals were defined as referral indications not approved by FDA, SNM or EMA guidelines and included differentiating PD from other PS, dystonia, vascular parkinsonism, dementia and unknown along with assessing progression (see table 1 for recommended indications for DaTSCAN). We reviewed all available handwritten charts in our two hospitals in order to evaluate the utility of scans for future clinical management.
Study Ethics was received from both the Clinical Research Ethics Committee of the Cork Teaching Hospitals and the Research Ethics Committee of UHL prior to the initiation of the study. Data was inputted into SPSS version 20. Two groups were formed for statistical analysis: those with and without dopaminergic deficits. Descriptive statistics, frequencies along with Pearson’s chi-squared test were used.
Results
Patient demographics and referral sources
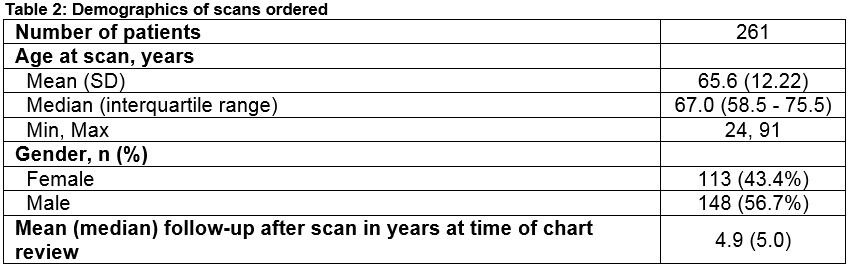
Two hundred and sixty-one patients underwent 123I-FP-CIT SPECT over a five-year period. One hundred and forty-eight (56.7%) were male and median age was 67 years (table 2). The number of scans ordered increased every year with the most scans completed in the final full calendar year. Scans were predominantly ordered by neurologists (54.4%), geriatricians (34.5%) and psychiatrists (6.1%). Thirteen scans were referred from other specialties including general medicine (n=6), rheumatology (n=2), respiratory (n=1), nephrology (n=1), gastroenterology (n=1) and emergency department (n=1). Fifty-five percent (55%) of scans were outside referrals, ordered by physicians working outside of our two hospitals.
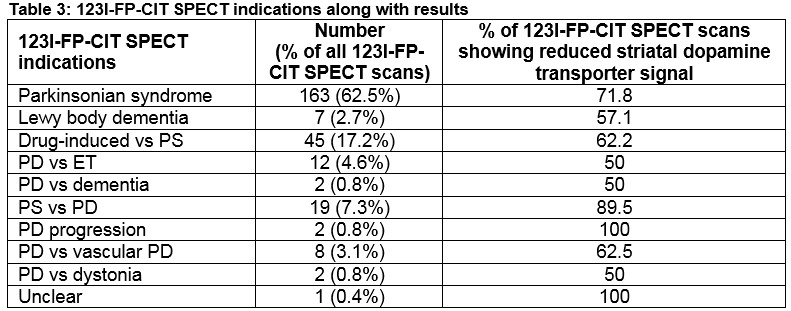
Referral reason
The most common reason for ordering a scan was for assessment of a parkinsonian syndrome (PS), accounting for 62.5% of referrals. Other frequent referral reasons were differentiating drug-induced Parkinsonism (DIP) from PS at 17.2% and PS vs. PD at 7.3%. Inappropriate referrals were seen in 13% of cases (table 3).
Symptomatology
We were interested in the documentation of Parkinsonism, in particular the symptoms needed for The United Kingdom Parkinson’s Disease Society Brain Bank Clinical Diagnostic (UKPDSBB) criteria1. One hundred and thirty-three patients (51%) had a tremor, 88 patients (33.7%) had rigidity, 69 patients (26.4%) had bradykinesia and 5 patients (1.9%) had postural instability documented on their request forms for imaging.
123I-FP-CIT SPECT results and subgroup analysis
One hundred and eighty patients (69%) had positive scans with dopaminergic deficit qualitatively assessed. Seventy-seven (42.7%) of these scans showed correct laterality between symptom sidedness and dopaminergic deficit on imaging. Thirty-two scans (17.9%) showed bilateral dopaminergic deficits in the presence of unilateral symptoms. Twenty-one scans (11.8%) showed dopaminergic deficit on the incorrect side to unilateral symptoms. In the remaining fifty scans (27.5%), the symptom sidedness was not documented on the referral forms. When comparing the demographics and symptomatology of those with evidence of dopaminergic deficit against those with a normal scan, no statistically significant difference was found regarding age, gender, indication for scan or symptoms.
Change of management
This was assessed by review of handwritten medical notes available in our two hospitals. Eighty-one charts were available for review. Forty-three (53%) of these scans were ordered by neurologists; 25 (30.9%) ordered by geriatricians; 7 (8.6%) ordered by psychiatrists and 6 (7.4%) ordered by general medical physicians. Documentation of further management was noted in 53 of these charts (65.4%). Twenty-four patients (29.6%) had a change of diagnosis from ET or DIP and PS. Seventeen patients (21%) were started on new medications including levodopa or anticholinergics, or had an increase in medication doses after confirmation of diagnosis. Eleven patients (13.5%) had either discontinued treatment or didn’t start planned medication.
In regards to specialties, changes in management were noted in 65.9% of neurology (27 patients), 94.7% of geriatrics (18 patients), 50% of psychiatry (2 patients), and 100% of general medicine (6 patients) referrals.
Discussion
Over the five-year period the number of scans ordered almost quadrupled, from 21 scans in the first year to 79 in the final year. We think this reflects the increased awareness of the utility of 123I-FP-CIT SPECT in diagnosing parkinsonian syndromes. Many of our patients (62.5%) were referred for this scan in cases of PS, although it was often unclear from the referral forms what other diagnoses were being considered in addition to PS. The second most common indication was for DIP (17.2%). DIP is important to identify as withdrawal of the offending drug can reverse the symptoms of parkinsonism9. 123I-FP-CIT SPECT scans are ideal for these patients as neuroleptics predominantly affect the postsynaptic dopamine receptors with only a negligible affinity for the dopamine transporter (DAT)10-11. Interestingly, 26 patients prescribed neuroleptics were found to have evidence of dopaminergic deficit on neuroimaging. This has been reported before with antidopaminergic drugs felt to unmask prematurely presymptomatic PD12.
Inappropriate referrals for 123I-FP-CIT SPECT are important to identify and prevent as they are a waste of resources and cause an unnecessary risk to patients without benefit6,13. We found inappropriate referrals in 34 cases (13% of total) resulting in an estimated cost of €48,000 euros to the health service. Documented reasons for ordering the scan included differentiating PS from PD; PD from dystonia; PD from dementia with lewy bodies or assessing progression in PD. Although ongoing research is investigating variant mapping techniques of 123I-FP-CIT SPECT and other biomarkers for these reasons6, they are currently not clinical indications for the scan and are not licensed by the EMA, SNM and FDA guidelines (table 1). Positive scans (i.e. evidence of qualitative dopaminergic deficit) were seen in 69% of cases. We noted a slight trend to a higher proportion of positive scans in the under 60 age group versus the over 60 age group, at 76% versus 66.1% (p = 0.118), which has been reported previously4. Although not studied in our study, there is an age-related decline of radiotracer uptake in normal patients of 3.3 to 10% per decade14, making the interpretation of results in an older age group more difficult. Eighty-one scans (31%) were normal with no evidence of dopaminergic deficit. Possible diagnoses for normal scans include ET, dystonia, dementia not related to Lewy body disease, vascular parkinsonism, DIP and psychogenic parkinsonism.
As 55% of patients were referred from outside institutions, we were limited in our chart review. However, we were able to assess change of management in patients under the care of neurologists, geriatricians, psychiatrists and general medical physicians. A change in management after 123I-FP-CIT SPECT was clearly documented in 65.4% of our chart review subgroup. This was consistent with a recent multicentre, open, non-randomized study which showed change in planned management in 72% of their patients after DaTSCAN8. Another retrospective review, reported a change in management in 63% of cases11. Interestingly in three of our patients, the scans results were not accepted by the ordering physician suggesting some uncertainty in the scan’s validity.
The overdiagnosis of PD at initial presentation occurs in 10 to 47% of patients in both community and hospital settings15,16. This misdiagnosis of PD is more likely with non-specialists compared to Movement disorder experts17. In our study, only three scans were requested by a recently appointed Movement disorder specialist. Prior research had scans ordered solely by neurologists18. However, patients with parkinsonism can present to any specialty and the feasibility and cost-effectiveness of restricting the ordering of these scans to only neurologists is debatable19.
Given the retrospective nature of the study, the large percentage of outside referrals to our centers for these scans and the reliance on handwritten scan request forms and chart reviews for data collection there were some limitations to our study. In particular, we were only able to assess change of management in one-third of scans due to either unclear documentation or inability to access the handwritten medical records.
Accurate clinical diagnosis in patients with Parkinsonism can often be challenging, especially early in the disease when signs are minimal; when atypical features are present or when there are other comorbidities. Dopamine transporter imaging can assist with diagnosis provided it is used for the correct indications. In our study we showed an increased awareness and utility of dopamine transporter scans in diagnosing parkinsonian syndromes in our health service. We also identified a significant number of inappropriate referrals which will be important to address in the future through education or strict indications on scan request forms in order to reduce the waste of resources and prevent unnecessary radiation exposure to patients.
Correspondence
Grace Crotty, MBBChBAO MRCPI, Department of Neurology, Brigham and Women’s hospital, 75 Francis Street, Boston, MA, USA 02115.
Email: [email protected]
Financial disclosure/conflicts of interest: The authors of this manuscript have NO affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
References:
1. Gibb WRG, Lees AJ. The relevance of the Lewy body to the pathogenesis of idiopathic Parkinson's disease. J Neurol Neurosurg Psychiatry 1988;51:745-52.
2. Hughes AJ, Daniel SE, Lees AJ. Improved accuracy of clinical diagnosis of Lewy body Parkinson's disease. Neurology. 2001;23,57(8):1497-9.
3. Hughes AJ, Daniel SE, Ben-Shlomo Y, Lees AJ. The accuracy of diagnosis of parkinsonian syndromes in a specialist movement disorder service. Brain. 2002;125:861-70.
4. Marshall VL, Reininger CB, Marquardt M, Patterson J, Hadley DM, Oertel WH, Benamer HT, Kemp P, Burn D, Tolosa E, Kulisevsky J, Cunha L, Costa D, Booij J, Tatsch K, Chaudhuri KR, Ulm G, Pogarell O, Höffken H, Gerstner A, Grosset DG. Parkinson's disease is overdiagnosed clinically at baseline in diagnostically uncertain cases: a 3-year European multicenter study with repeat [123I]FP-CIT SPECT. Mov Disord. 2009; 24(4):500-8.
5. Djang D, Janssen M, Bohnen N, Booij J, Henderson T, Herholz K, Minoshima S, Rowe C, Sabri O, Seibyl J, Van Berckel B, Wanner M. SNM Practice Guideline for Dopamine Transporter Imaging with 123I-Ioflupane SPECT 1.0. J Nucl Med. 2012 Jan;53(1):154-63.
6. Bajaj N, Hauser RA, Grachev ID. Clinical utility of dopamine transporter single photon emission CT (DaT-SPECT) with (123I) ioflupane in diagnosis of parkinsonian syndromes. J Neurol Neurosurg Psychiatry. 2013;84(11):1288-95.
7. Bajaj NP, Gontu V, Birchall J, Patterson J, Grosset DG, Lees AJ. Accuracy of clinical diagnosis in tremulous parkinsonian patients: a blinded video study. J Neurol Neurosurg Psychiatry. 2010;81:1223–8.
8. Catafau A, Tolosa E. Impact of dopamine transporter SPECT using 123I-Ioflupane on diagnosis and management of patients with clinically uncertain parkinsonian syndromes. Mov Disord. 2004;19(10):1175-82.
9. Thanvi B, Treadwell S. Drug induced parkinsonism: a common cause of parkinsonism in older people. Postgrad Med J. 2009;85(1004):322-6.
10. Reader TA, Ase AR, Huang N, Hébert C, van Gelder NM. Neuroleptics and dopamine transporters. Neurochem Res. 1998;23:73–80.
11. Sadasivan S, Friedman JH. Experience with DaTscan at a tertiary referral center. Parkinsonism Relat Disord. 2015;21(1):42-45.
12. Tolosa E, Wenning G, Poewe W. The diagnosis of Parkinson's disease. Lancet Neurol. 2006;5(1):75-86.
13. Grosset DG, Tatsch K, Oertel WH, Tolosa E, Bajaj N, Kupsch A, O'Brien JT, Seibyl J, Walker Z, Sherwin P, Chen C, Grachev ID. Safety Analysis of 10 Clinical Trials and for 13 Years After First Approval of Ioflupane 123I Injection (DaTscan). J Nucl Med. 2014;55(8):1281-7.
14. Eerola J, Tienari PJ, Kaakkola S, Nikkinen P, Launes J. How useful is [123I]beta-CIT SPECT in clinical practice? J Neurol Neurosurg Psychiatry. 2005;76(9):1211-16.
15. Rajput AH, Rozdilsky B, Rajput A. Accuracy of clinical diagnosis in parkinsonism—a prospective study. Can J Neurol Sci. 1991 Aug; 18(3): 275-8.
16. Schrag A, Ben-Shlomo Y, Quinn N. How valid is the clinical diagnosis of Parkinson’s disease in the community? J Neurol Neurosurg Psychiatry. 2002 Nov; 73(5): 529- 534.
17. Jennings DL, Seibyl JP, Oakes D, Eberly S, Murphy J, Marek K. [123I] b-CIT and single-photon emission computed tomographic imaging vs clinical evaluation in Parkinsonian syndrome: unmasking an early diagnosis. Arch Neurol. 2004;61:1224–1229.
18. Kagi G, Bhatia KP, Tolosa E. The role of DAT-SPECT in movement disorders. J Neurol Neurosurg Psychiatry. 2010; 81(1):5-12.
19. Manoharan P, Jamieson S, Bury RF. Initial clinical experience with [123I] ioflupane scintigraphy in movement disorders. Clinical radiology. 2007;62(5):463-71.
(P751)
