Staff Attitudes towards Patient Safety Culture and Working Conditions in an Irish Tertiary Neonatal Unit
Dwyer L1, Smith A1, McDermott R2, Breatnach C1, El-Khuffash A1, Corcoran JD1
1.Department of Neonatology, The Rotunda Hospital, Dublin
2.Department of Research, The Rotunda Hospital, Dublin
Abstract
Introduction
There is little published research evaluating attitudes towards patient safety culture and working conditions in neonatal units. This study aimed to explore this within a Level III Irish neonatal unit setting.
Methods
This was a quantitative, cross-sectional study performed in the Rotunda Hospital, Dublin. A 30-item safety attitudes questionnaire (SAQ) was utilized to analyze staff perceptions in areas including job satisfaction, working conditions and stress recognition.
Results
The ‘Stress Recognition’ domain received the highest score (75.3) followed by ‘Job Satisfaction’ domain with a mean score of 74.4. The lowest mean scale score in the neonatal unit was for ‘Perceptions of Management’, with a mean score of 50.7. Collaboration and Communication scores were high across all disciplines.
Conclusion
This SAQ has highlighted a number of important areas for quality improvement and staff satisfaction in our neonatal unit.
Introduction
Medical error is an adverse event defined as an injury resulting from a medical intervention and not caused by an underlying medical condition1. There is mounting evidence regarding the serious impact ‘iatrogenic’ harms may pose to patient wellbeing in complex healthcare systems. Ensuring patient safety is a vital component of any high quality healthcare service2. A European report entitled ‘Safety Improvement for Patients in Europe’ emphasized that patient safety must focus on identifying, analyzing and minimizing patient risk3.
Several studies have aimed to classify the type of medical errors found in different medical contexts4–6. European data demonstrate that medical errors and healthcare related adverse events occur in 8-12% of hospitalizations7. Healthcare associated infections (HAI) affect approximately one in 20 hospital inpatients annually in Europe, equating to over 4.1 million affected patients8. A recently published EU commission report found that adverse events related to HAIs directly cause 37,000 deaths/year, and contribute to a further 10,000 deaths/year with an annual cost to hospitals of more than €5.4 billion/year9.
In healthcare, a significant percentage of errors are due to poor communication and lack of effective teamwork10. Developing a culture of professional cooperation, teamwork and effective communication can improve staff job satisfaction. In turn, such an environment will enhance the quality of healthcare provision, advance patient safety, reduce error and decrease workload. Thus, hospital management must view the ability of their staff to function in an harmonious, cohesive team as an essential component in the establishment of safe hospital systems1,10,11.
In spite of the costs of medical errors in Ireland, there is little published research investigating interventions to improve safety climate or culture in hospital settings12,13. It is widely accepted that healthcare is a high hazard industry due to the inherent risk of morbidity and mortality14. While new approaches are being established, there are limited methods available to determine the effects of interventions on outcomes15. This study is aims to address this research gap. The primary objective is to assess the safety culture in a tertiary neonatal unit of a university teaching hospital16.
Methods
This was a quantitative, cross-sectional study. The data was collected between July 2016 and March 2017. The Rotunda Hospital is a stand-alone tertiary maternity and neonatal centre with an annual birth rate of 8,500. The Rotunda Hospital contains a 39-bedded level 3 neonatal unit providing neonatal intensive care, high dependency and special care facilities for all the infants born at the Rotunda hospital and for high risk or sick infants born in the Royal College of Surgeons Ireland network hospitals. There are 65 whole time equivalent nursing staff, 6 neonatal consultants and 17 non-consultant hospital doctors. There are three Advanced Neonatal nurse Practitioners (ANPs).
The most commonly used and rigorously validated tool to measure safety culture is the Safety Attitudes Questionnaire (SAQ)17. Higher scores on the SAQ are linked with lower rates of nurse turnover, postoperative sepsis, infection and inpatient mortality17. The SAQ has been utilized across the US, UK and New Zealand18.
The SAQ is a 60-item survey which elicits healthcare professionals perceptions in six areas; the teamwork climate, the safety climate, the perceptions of management, job satisfaction, working conditions and stress recognition, with a response scale ranging from 1 (disagree strongly) to 5 (agree strongly) using a 5-point Likert scale. The scores were then transformed to a numerical 100-point scale to aid in analysis of the results (1=0, 2=25, 3=50, 4=75 and 5=100). Each domain score equals the mean score of its component survey items19,20. A further 30 items investigate additional aspects of safety, which vary according to the particular unit type being surveyed. The SAQ also captures relevant respondent demographics. Respondents were grouped with different job positions as follows: (1) doctors - includes all medicine and critical care physicians across all levels of training; (2) nurses - includes critical care nurses, ANPs, licensed vocational nurses, nurse managers, charge nurses and midwives; and (3) ancillary personnel - includes pharmacists, nursing aides and assistants, ward clerks, radiographers, dieticians and porters. Surveys that were blank or had uniform responses (e.g., all of the responses were ‘neutral’ or ‘agree strongly’) were excluded from this analysis because they did not provide any diagnostic information. Approval by the Hospital ethics committee was sought and approval was granted. The participants were informed about the aims of the study. Responding to the questionnaire was voluntary and anonymous.
Data were analyzed using SPSS version 20. The scores of the two negatively-worded survey items were reversed. A composite scale score was calculated by summing the scores of the items with the scale. Descriptive statistics were used for all survey items and domains. Internal consistency was measured via Cronbach's alpha in this survey instrument to gauge its reliability. Alpha coefficient ranges in value from 0 to 1 were used to describe the reliability of factors extracted from the Likert scale.
Results
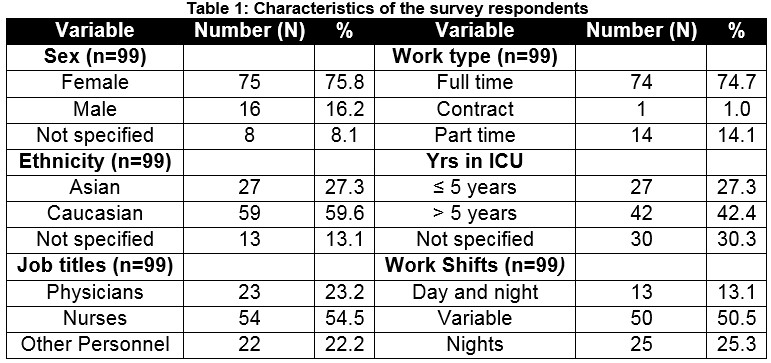
Ninety-nine members of staff participated in this survey. Table 1 illustrates the demographics of the survey respondents.
The SAQ item responses are outlined in Table 2. The respondents' mean and standard deviation ratings of the SAQ items are illustrated.
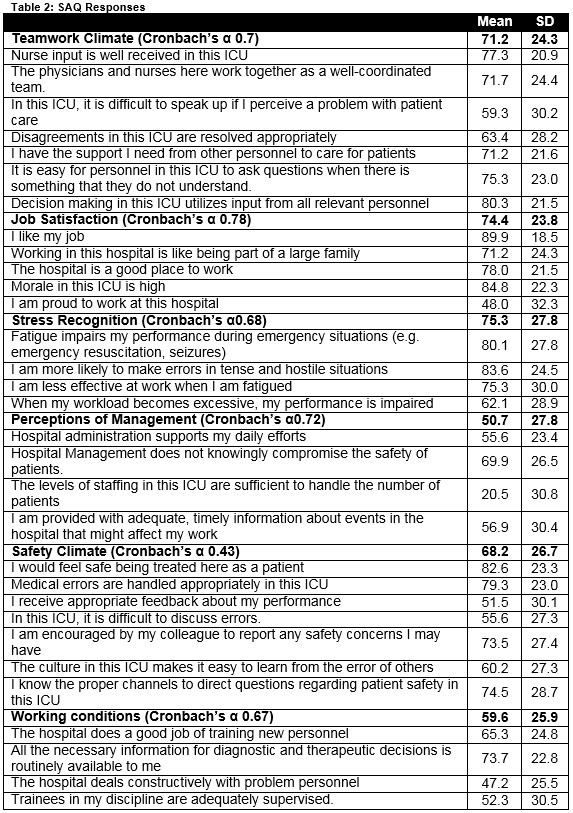
Table 3 reports the analysis of the ‘Collaboration and Communication’ section of the SAQ. Teamwork ratings from each healthcare group were found to be similar across caregiver type, with the largest differences in perceptions of teamwork between Doctors and Nurses in the neonatal unit and the laboratory. Doctors rated teamwork with the lab as 3.87 out of 5.00 (77%). This score was reciprocated by staff nurses, who scored communication and collaboration with the lab at 3.84 out of 5.00 (77%). The teamwork ratings by both doctors and nurses with other personnel were high.
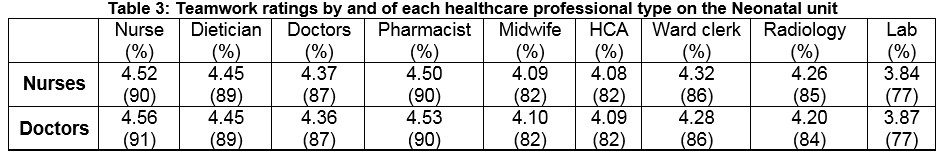
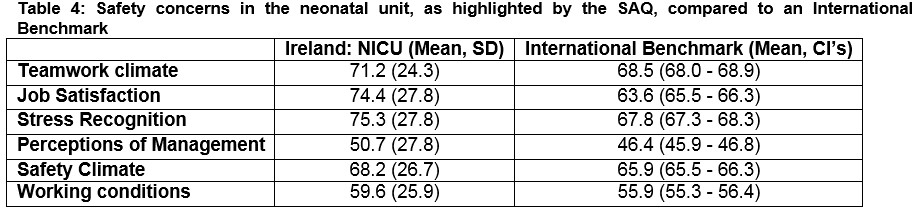
Table 4 illustrates the comparison of the results of our survey with international benchmarks. The results of our SAQ are higher across all 6 areas of assessment when compared with international data.
Discussion
This study assessed the safety culture within a tertiary neonatal unit. While this SAQ has been utilized in a number of hospital environments this is the first time it has been applied to an Irish neonatal setting.
The majority of staff were female, Caucasian, full-time employees, with over five years’ experience in and ICU setting. Nursing staff comprised the majority of study participants at 54.5%. The ‘Stress Recognition’ domain received the highest mean score at 75.3, followed by ‘Job Satisfaction’ with a mean score of 74.4. The majority, 71.7%, of those surveyed felt that the physicians and nurses work together as a well co-ordinated team and 80.3% felt that decision making in the ICU utilizes input from all relevant personnel. Also, 89.9% responded that they like their job and 78% felt that the hospital was a good place to work. 82.6% responded that they would feel safe being treated in the Rotunda Hospital as a patient and 79.3% responded that medical errors are handled appropriately in the NICU. Collaboration and Communication scores were high across all disciplines at 76%, as demonstrated in Table 3. Importantly, the Rotunda neonatal unit scored higher for all domains when compared to international benchmarked data as per Table 5.
However there are several key areas for future improvement and the SAQ highlighted two particularly important points: perceived lack of support from hospital management and apprehensions regarding stress recognition and working conditions. For example, only 59.3% of those surveyed felt that it was difficult to speak up if they perceived a problem with patient care and 20.5% felt that the levels of staffing in the ICU are sufficient to handle the number of patients. There were 52.3% of the respondents that felt that trainees in their discipline are adequately supervised and less than half of respondents (47.2%), felt that the hospital deals constructively with problem personnel.
There are many challenges for hospital management to remedy such issues fully. There are significant difficulties on a national scale with suitable staff recruitment and retention. However, a number of methods could be implemented to create a more supportive work environment with regards to staffs concerns about safety. A no-blame culture to medical error and must be promoted and open, multidisciplinary discourse facilitated on how to improve medical structures and processes23. Completion and regular discussion of clinical incident forms should be encouraged. Frequent contact between medical and nursing management and front line staff in both formal and informal settings would help foster better working relationships. Staff should receive regular feedback and performance evaluations in order to enable continuing professional development23. Raising awareness of educational opportunities and relevant events such as study days, conferences and multidisciplinary meetings will aid in allowing staff to access up to date information in their field and connect with other healthcare providers. Staff induction and on-going training will be an important area to develop. Effective management is vital for ensuring good morale, collegiality and teamwork. It is important that teamwork climate scores remain high as low scores have been associated with difficulties in retaining caregivers21. Moreover, both domains of teamwork and perceptions of management are responsive to interventions. Improved communication in hierarchy and leadership walk rounds can improve teamwork and perceptions of management respectively24,25.It is important that the continuation of the research into the safety culture in Ireland involves feedback to both staff and management in an effort to improve outcomes. It is a legal requirement for safety teams to be established in an Irish context, and as such, identify and manage risks.
To our knowledge, this is the first study to investigate safety culture within an Irish neonatal setting. As such the findings may also be applicable to other Irish neonatal units. This study will aid in developing a safety network team to address the full spectrum of safety issues arising in our neonatal unit. Future studies should validate whether safety culture correlates with clinical and operational outcomes in the NICU setting.
Conflict of Interest
The authors declare no conflict of interest.
Corresponding Author
Liam Dwyer, The Rotunda Hospital, Parnell Square, Dublin
E: [email protected]
T: (01) 817 1700
References
1. Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Vol. 21, Annales francaises d’anesthesie et de reanimation. 2000. 453-454 p.
2. Committee on Quality of Health Care in America I of M. Crossing the Quality Chasm: A New Health System for the 21st Century. In: Crossing the Quality Chasm: A New Health System for the 21st Century. 2001. p. 61–88.
3. Improvement S, Patients FOR, Europe IN. Interim Report SIMPATIE Project. 2008;(May 2006):1–55.
4. West DR, Pace WD, Dickinson LM, Harris DM, Main DS, Westfall JM, Fernald DH, Staton EW. Relationship Between Patient Harm and Reported Medical Errors in Primary Care: A Report from the ASIPS Collaborative. Adv Patient Saf New Dir Altern Approaches. 2008;1–10.
5. Van Vorst RF, Araya-Guerra R, Felzien M, Fernald D, Elder N, Duclos C, Westfall JM. Rural community members’ perceptions of harm from medical mistakes: a High Plains Research Network (HPRN) Study. J Am Board Fam Med [Internet]. 2007;20(2):135–43. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17341749
6. Gehring K, Schwappach DLB, Battaglia M, Buff R, Huber F, Sauter P, Wieser M. Frequency of and harm associated with primary care safety incidents. Am J Manag Care. 2012;18(9):E323–37.
7. Gabrani A, Hoxha A, Simaku A, Gabrani J. Application of the Safety Attitudes Questionnaire (SAQ) in Albanian hospitals: a cross-sectional study. BMJ Open [Internet]. 2015;5(4):e006528–e006528. Available from: http://bmjopen.bmj.com/cgi/doi/10.1136/bmjopen-2014-006528
8. World Health Organization. Health care-associated infections Fact sheet. World Heal Organ [Internet]. 2015;4. Available from: http://www.who.int/gpsc/country_work/gpsc_ccisc_fact_sheet_en.pdf
9. European Commission. Info graph “Patient Safety in the EU: 2014”. http://ec.europa.eu/health/patient_safety/docs/ps2014_infograph_en. pdf.
10. Lo LCPSI. Teamwork and Communication in Healthcare a Literature Review. Can Patient Saf Inst [Internet]. 2011;68. Available from: www.patientsafetyinstitute.ca
11. Singer SJ, Vogus TJ. Reducing Hospital Errors: Interventions that Build Safety Culture. Annu Rev Public Health [Internet]. 2013;34(1):373–96. Available from: http://www.annualreviews.org/doi/10.1146/annurev-publhealth-031912-114439
12. Verbakel NJ, Langelaan M, Verheij TJM, Wagner C, Zwart DLM. Improving Patient Safety Culture in Primary Care: A Systematic Review. J Patient Saf [Internet]. 2014;0(0):1–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24647271
13. Relihan E, Glynn S, Daly D, Silke B, Ryder S. Measuring and benchmarking safety culture: application of the safety attitudes questionnaire to an acute medical admissions unit. Ir J Med Sci. 2009;178(4):433–9.
14. Colla JB, Bracken AC, Kinney LM, Weeks WB. Measuring patient safety climate: a review of surveys. Qual Saf Health Care [Internet]. 2005;14(5):364–6. Available from: http://qshc.bmj.com/content/14/5/364.abstract%5Cnhttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1744072&tool=pmcentrez&rendertype=abstract
15. Makary MA, Sexton JB, Freischlag JA, Millman EA, Pryor D, Holzmueller C, Pronovost PJ. Patient Safety in Surgery. Ann Surg [Internet]. 2006;243(5):628–35. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00000658-200605000-00008
16. Sexton JB, Thomas EJ, Helmreich RL. Error, stress, and teamwork in medicine and aviation: cross sectional surveys. BMJ. 2000;320(7237):745–9.
17. Pronovost PJ, Miller MR, Wachter RM. Tracking progress in patient safety: an elusive target. JAMA. 2006;296(6):696–9.
18. Sexton JB, Helmreich RL, Neilands TB, Rowan K, Vella K, Boyden J, Roberts PR, Thomas EJ. The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res [Internet]. 2006;6(1):44. Available from: http://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-6-44
19. Abu-el-noor NI, Abduallah M, Abu-el-noor MK, Radwan AS, Ali A. Journal of Paediatric Nursing Safety Culture in Neonatal Intensive Care Units in the Gaza Strip , Palestine : A Need for Policy Change. J Pediatr Nurs [Internet]. 2017;33:76–82. Available from: http://dx.doi.org/10.1016/j.pedn.2016.12.016
20. Huang DT, Clermont G, Kong LAN, Weissfeld LA, Sexton JB, Rowan KM, Angus DC. Intensive care unit safety culture and outcomes : a US multicenter study †. 2010;22(3):151–61.
21. Sexton JB, Holzmueller CG, Pronovost PJ, Thomas EJ, McFerran S, Nunes J, Thompson DA, Knight AP, Penning DH, Fox HE. Variation in caregiver perceptions of teamwork climate in labor and delivery units. J Perinatol [Internet]. 2006;26(8):463–70. Available from: http://www.nature.com/doifinder/10.1038/sj.jp.7211556
22. Sexton JB, Helmreich RL, Neilands TB, Rowan K, Vella K, Boyden J, Roberts PR, Thomas EJ. The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res [Internet]. 2006;6:44. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16584553
23. Hughes RG. Patient safety and quality: an evidence-based handbook for nurses. Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2008. 1-1403 p.
24. Profit J, Etchegaray J, Petersen LA, Sexton JB, Hysong SJ, Mei M, Thomas EJ. Neonatal intensive care unit safety culture varies widely. Arch Dis Child - Fetal Neonatal Ed [Internet]. 2012;97(2):F120–6. Available from: http://fn.bmj.com/lookup/doi/10.1136/archdischild-2011-300635
25. McCulloch P, Mishra A, Handa A, Dale T, Hirst G, Catchpole K. The effects of aviation-style non-technical skills training on technical performance and outcome in the operating theatre. Qual Saf Heal Care [Internet]. 2009;18(2):109–15. Available from: http://qualitysafety.bmj.com/lookup/doi/10.1136/qshc.2008.032045
P786
