A Borderline Ovarian Tumour in a Patient with Classic Bladder Exstrophy; a Case Report.
K Beauchamp, G Ryan, B Gibney, T Walsh, D Brennan
Mater Misericordiae University Hospital Dublin.
Abstract
A 37-year-old Romanian lady presented with a large pelvic mass, urosepsis and deteriorating renal function. She had undergone separation from her conjoined twin. Imaging revealed grossly abnormal anatomy and a suspicious pelvic mass. Examination was consistent with classic bladder exstrophy. Postoperative histology showed borderline ovarian tumour (BTO).
Introduction
Bladder exstrophy is a rare congenital anomaly involving a defect in the abdominal wall with variations involving the external genitalia, pelvis and urinary tract. The incidence varies between 1:30,000 to 1:50,0001. It is believed to be caused by an abnormal cloacal membrane formation during embryological development1. BTO comprise 15-20% of all ovarian malignancies2. We present a complex case of BTO in the setting of bladder exstrophy and the complexities involved in managing a patient with aberrant anatomy.
Case Report
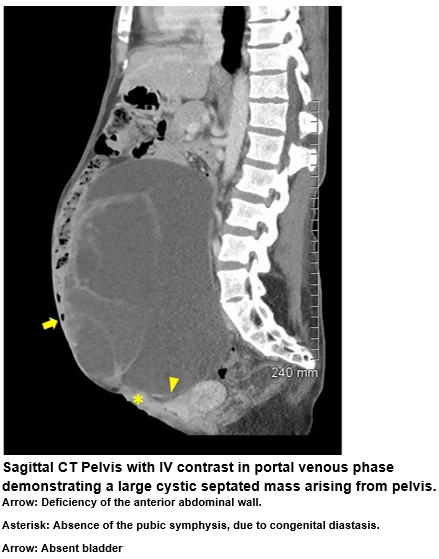
Ms X, a 37-year-old Romanian lady presented with urosepsis and renal failure secondary to a large pelvic mass. A poor historian, her only past medical history was surgical separation from her conjoined twin as a baby. Initially Ms X was managed with intravenous antibiotics. CT demonstrated a 23x19x13cm complex left adnexal mass, with multiple septations and mural nodularity. There was mass effect on the uterus, small volume of free fluid within the pelvis and retroperitoneal lymphadenopathy. The omentum had deposits suspicious for metastases. There was mass effect on the distal left ureter causing hydroureter and hydronephrosis with marked hypertrophy of the left kidney. The right kidney was markedly atrophied. No bladder was identified. The abdominal wall was deficient and there was diastasis of the pubic symphysis. MRI confirmed these findings except the lymphadenopathy was not identified.
CT urogram showed moderate left sided hydronephrosis. There was poor opacification of the left ureter along its retroperitoneal course. EUA identified a vaginal opening on the inferior abdominal wall and a normal cervix. No urethra was identified. Ms X was noted to be incontinent of urine but no obvious source of from where the urine was leaking. A large immobile pelvic mass was palpated abdominally. Surgery was planned due to worsening renal function. An antegrade left ureteric catheter was placed under fluoroscopic guidance preoperatively. A midline incision was performed which revealed extensive adhesions and a large complex left adnexal mass. Extensive left ureterolysis was performed which identified a wet conduit whereby the left ureter had been anastomosed to the sigmoid colon as a result of an absent bladder. This was presumably performed as part of the surgical separation of the conjoined twins. There was no evidence of metastatic disease. Left salpingo-oophorectomy, appendectomy and omental biopsies were performed. Ms X recovered in the high dependency unit. Postoperative histology showed a borderline mucinous tumour of the ovary of endocervical type. Omental biopsies and appendix were normal. Ms X returned to Romania well shortly after.
Discussion
Bladder exstrophy is a rare condition encompassing the exstrophy-epispadias complex.1 Classical bladder exstrophy affects the lower urinary tract, genitalia and musculoskeletal system1,3,4. Risk factors include maternal smoking, younger and grand multiparous mothers, in-vitro fertilisation, family history, and male gender3,4,5. Bladder exstrophy is usually diagnosed prenatally or immediately after birth. 3 Findings include an open bladder on the lower abdominal wall with mucosa exposed through a fascial defect. The distance between the umbilicus and anus is shortened. The vagina and anus are both anteriorly displaced along with a bifid clitoris with divergent labia superiorly. Abdominal recti diverge distally and attach to widely separated pubic bones3.
Investigations include bloods and imaging of the urinary tract looking for hydronephrosis, renal agenesis, and ectopic pelvic kidney. Bilateral vesicoureteral reflux is seen in almost all cases. Voiding cystourethrography should be performed to assess bladder capacity prior to reconstructive continence surgery6. Initial management is conservative with prophylactic antibiotics, and protection of the bladder7. Surgical management can be with a staged procedure or a total reconstruction8,9,10. Long term monitoring of renal and bladder function is important. The above case illustrates the complexity when a relatively common condition such as a borderline ovarian tumour presents in a patient with grossly abnormal anatomy. It also highlights the difficulties entailed through language barriers and when patients have poor knowledge of their past medical history.
Conflict of Interest
The authors confirm that there are no conflicts of interest.
Correspondence
Dr Katie Beauchamp, Gynaecology Dept, Mater Misericordiae University Hospital Dublin 7.
Email: [email protected]
References
1. Bladder Exstrophy and Epispadias – www.urology-textbook.com. Urology-textbook.com 2017.
2. Borderline ovarian tumours | Ovarian cancer | Cancer Research UK. Cancerresearchuk.org 2017.
3. Jayachandran D, Bythell M, Platt MW, Rankin J. Register based study of bladder exstrophy-epispadias complex: prevalence, associated anomalies, prenatal diagnosis and survival. J Urol. 2011 Nov. 186(5):2056-60. [Medline].
4. Epidemiology of bladder exstrophy and epispadias; a communication from the International Clearinghouse for Birth Defects Monitoring Systems. Teratology. 1987 Oct;36(2):221-7.
5. Wood HM, Babineau D, Gearhart JP. In vitro fertilization and the cloacal/bladder exstrophy-epispadias complex: A continuing association. J Pediatr Urol. 2007 Aug. 3(4):305-10. [Medline].
6. Mensah J.E, Asante E.K, Mensah Appeadu, Glover Addey H. Continent cutaneous diversion for bladder exstrophy in adults. African Journal of Urology. 2013 June 19 (2) 94-98.
7. Clinical manifestations and initial management of infants with bladder exstrophy Uptodate.com. 2017.
8. Shnorhavorian M, Grady RW, Andersen A, Joyner BD, Mitchell ME. Long-term followup of complete primary repair of exstrophy: the Seattle experience. J Urol. 2008 Oct. 180(4 Suppl):1615-9; discussion 1619-20. [Medline].
9. Bhatnagar V. Bladder exstrophy: An overview of the surgical management. J Indian Assoc Pediatr Surg. 2011 Jul. 16(3):81-7. [Medline].
10. Baird AD, Nelson CP, Gearhart JP. Modern staged repair of bladder exstrophy: A contemporary series. J Pediatr Urol. 2007 Aug. 3(4):311-315. [Medline]
(P695)