A Combination of Surgery And Methotrexate for Successful Treatment of a Caesarean Scar Ectopic Pregnancy.
WG Tadesse, G Von Bunau
Department of Gynaecology, the Adelaide and Meath National Children's Hospital, Dublin, Republic of Ireland
Abstract
Caesarean scar ectopic pregnancy (CSEP) is one of the rarest forms of ectopic pregnancies. With rising caesarean delivery (CD) rates worldwide, there is an increase in the incidence of CSEP. Patients usually present with painless vaginal bleeding and often misdiagnosed as spontaneous miscarriage. The use of ultrasonography with colour flow Doppler helps in the differential diagnosis. Different treatment options are described in the literature, although there is insufficient evidence regarding the best approach. We report the diagnosis and management of a case of CSEP in a woman with four previous CD who presented with vaginal bleeding and lower abdominal cramps at six weeks of gestation. She was treated with laparoscopic and ultrasound guided aspiration of the gestational sac and local injection of methotrexate supplemented by intramuscular methotrexate injection.
Introduction
CSEP is one of the rarest forms of ectopic pregnancies1-5. It is characterised by a gestation separated from the endometrial cavity and surrounded by the myometrium and the fibrous tissue of the scar. It usually presents with painless vaginal bleeding and often misdiagnosed as spontaneous miscarriage1. The major risk of CSEP is the early uterine rupture with life-threatening maternal haemorrhage leading to hysterectomy and loss of reproductive potential. The use of ultrasonography with colour flow Doppler is a useful adjunct in the workup of CSEP. An early diagnosis can offer treatment options capable of preserving the uterus2,5. We describe the diagnosis and management of a case of CSEP who presented to our emergency department with vaginal bleeding and lower abdominal cramps at six weeks of gestation.
Case Report
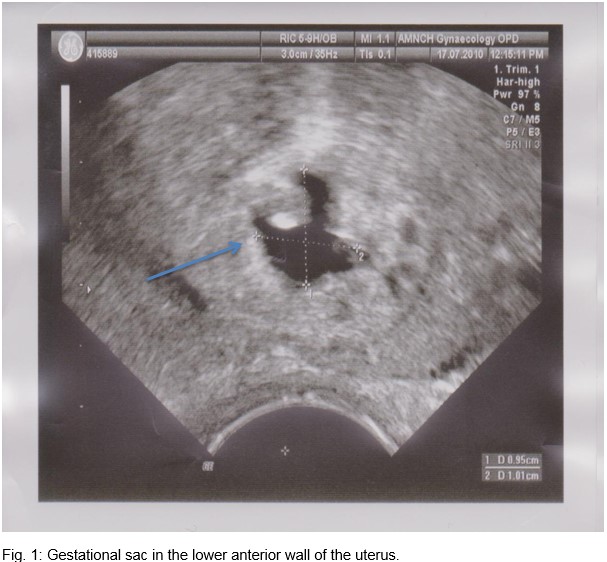
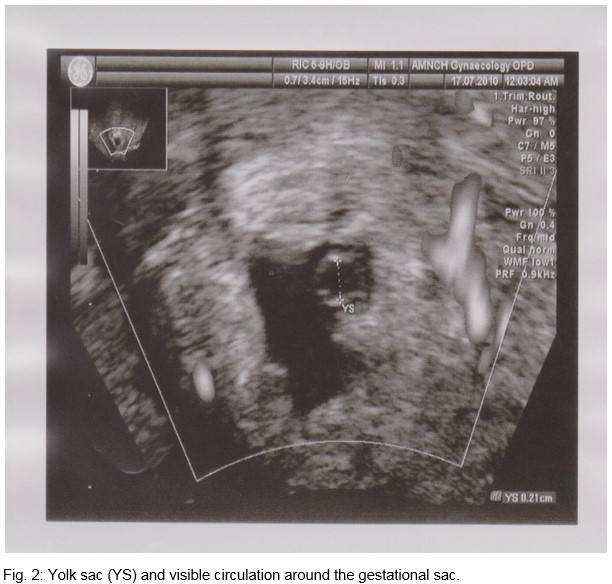
A 39-year-old Gravida 5 Para 4 woman presented to the emergency department with vaginal bleeding and mild lower abdominal pain of an hour duration. She was six weeks amenorrheic. All her previous deliveries were by caesarean, and her last delivery was four months ago. At presentation, she was haemodynamically stable with a haemoglobin of 12.4 g/dl. The cervix was closed, and there was no adnexal mass or tenderness. Transvaginal sonography (TVS) showed a 9.6mm irregular echolucent area in the anterior lower uterine wall, which appeared to be a gestational sac with a yolk sac (figure 1). There was positive colour flow around this echolucent area (figure 2). The uterus measured 10 x 5.6 cm. Both adnexae appeared normal. There was a moderate amount of free fluid in the Pouch of Douglas. Serum beta-hCG was 9404 IU/L.
Based on the findings on TVS, we considered a diagnosis of CSEP with possible intra-abdominal bleeding. We performed a diagnostic laparoscopy, which revealed a dense omental adhesion to the previous caesarean scar obscuring the view in the pelvis. The adhesion was dissected off the uterus. The uterus was intact, and the SCEP could not be seen laparoscopically. Therefore, intraoperative TVS was used to guide laparoscopic needle aspiration of the gestational sac content and to inject methotrexate (50mg) into the sac. The patient received an additional dose of methotrexate intramuscularly 48 hours later and discharged home on day three. Serum beta-hCG levels were monitored weekly, which became normal 30 days after the initial treatment.
Discussion
The commonest presenting symptom of SCEP is painless vaginal bleeding that can be substantial2. The cervical os is usually closed. There are proposed ultrasound diagnostic criteria, allowing a differential diagnosis from cervical ectopic pregnancy and miscarriage. These include a gestational sac located between the bladder wall and the anterior isthmic portion of the uterus, no trophoblastic tissue visible in the uterine cavity and cervical canal, and blood flow surrounding the sac2,6.
Treatment depends on several criteria including haemodynamic status, severity of vaginal bleeding, presence of fetal cardiac activity, gestational age, and beta-hCG level2. A number of case reports described surgical and non-surgical management options, although there is very little evidence as to which is the best approach5. These options include, hysterectomy4, dilatation and curettage and excision of trophoblastic tissue using laparotomy or laparoscopy5,7, aspiration of the amniotic fluid plus local and/or systemic methotrexate administration1,4, bilateral hypogastric artery ligation with dilatation and evacuation under laparoscopic guidance8, and selective uterine artery embolisation with curettage and/or methotrexate injection2.
With the rising rates of caesarean deliveries, an increase in the incidence of SCEP is expected1,4,9,10. Therefore, clinicians should be aware of this rare but potentially serious complication of pregnancy. In our case, the features on TVS were characteristic to make the diagnosis of SCEP and successfully managed with a combination of surgery and methotrexate. We monitored the response to treatment using serial serum beta-hCG levels.
Consent
Consent was obtained from the patient for publication of this case report
Conflict of interest
None
Corresponding author
WG Tadesse, Department of Obstetrics and Gynaecology, The Rotunda Hospital, Parnell Square, Dublin 1
Email: [email protected]
References
1. G Tan, YS Chong, A. Biswas. Caesarean scar pregnancy: A diagnosis to consider carefully in patients with risk factors. Ann Acad Med Singapore 2005; 34: 216-9.
2. L. Tulpin, O. Morel, C. Malartic, E. Barranger. Conservative management of a caesarean scar ectopic pregnancy: a case report. Cases Journal 2009, 2: 7794.
3. KM Seow, LW Huang, YH Lin, M Yan-Sheng Lin, YL Tsai, JL Hwang. Caesarean scar pregnancy: issues in management. Ultrasound in Obs & Gyn. 2004; 23(3): 247 – 253.
4. R Maymon, R Halperin, S Mendlovic, D Schneider, Z Vaknin, A Herman, M Pansky. Ectopic pregnancies in caesarean section scars: the 8 year experience of one medical centre. Human reproduction 2004; 19(2): 278 -284.
5. A Yalinkaya, O Yalinakay, G Olmez, M Yayla. Ectopic pregnancy in a previous caesarean section scar: a case report. The intern J of Gynecol and Obst 2004; 3 (1): 1528-8439.
6. C.H Mini, V Rabiyabi. Caesarean scar ectopic pregnancy: case report. Calicut Med J. 2008; 6(4): e7.
7. EL Lee, CJ Wang, A. Chao, CF Yen, YK Soong. Laparoscopic management of an ectopic pregnancy in a previous caesarean section scar. Case report. Human Reproduction, 1999; 14 (5): 1234 -1236.
8. FT Kung, TL Huang, CW Chen, YF Cheng. Image in reproductive medicine: Caesarean scar ectopic pregnancy. Fertil Steril 2006, 85: 1508 – 1509.
9. AK Mahapatro, K Shankar, T Varma. Caesarean Scar Ectopic Pregnancy: Report of Two Cases. J Clin Diagn Res. 2016; 10(5): QD05-6. doi: 10.7860/JCRD/2016/18075.7848
10. Deepika, T Gupta, S Washi. A Rare Case Report of Caesarean Scar Ectopic Pregnancy. J Clin Diagn Res. 2017; 11(8): QD10- QD11. doi: 10.7860/JCDR/2017/24611.10523.
(P774)
