A Cross-Sectional Study of Antibiotic Prescribing for Childhood Upper Respiratory Tract Infections in Irish General Practice
Maguire F 1, *, Murphy ME 2, *, Rourke M 3, *, Morgan F 3, Brady G 3, Byrne E 3, O’Callaghan ME 3, *
1 School of Medicine, Trinity College Dublin, The University of Dublin, Ireland
2 HRB Centre for Primary Care Research, Royal College of Surgeons Ireland, Dublin 2, Ireland
3 Trinity College Dublin/Health Service Executive (TCD/HSE) GP training scheme, Floor 6, The Russell Centre, Tallaght Cross West, Tallaght, Dublin 24
* = Co-authors
Abstract
Introduction
This study aimed to analyse antibiotic prescribing in cases of upper respiratory tract infection (URTI) in children under 6 years attending Irish daytime and out-of-hours General Practice (GP) services. There have been large scale changes in entitlements for free GP care for this group in recent years.
Methods
A cross-sectional study of children under 6 years with URTI presentations was performed, over a two-week period for three years from 2015 to 2017. Factors associated with antibiotic prescription and preferred antibiotic compliance were examined using multivariate logistic regression.
Results
1,007 Under-6 patients presented with an URTI in our sample over the study period. Following introduction of free GP care, patients were 50% less likely to receive an antibiotic prescription. Overall antibiotic prescribing fell from 70% to 50% in daytime services and from 72% to 60% in the out-of-hours setting. Patients presenting to out-of-hours services were more likely to receive an antibiotic (OR: 1.42) and less likely to receive a deferred antibiotic (OR: 0.53). One quarter to one third of all prescriptions were for deferred antibiotics. Year-on-year trends showed a 13% decrease in prescriptions and 13% increase in preferred antibiotic use.
Conclusion
The introduction of free GP care led to significant reductions in antibiotic prescribing, which may be due to changes in health seeking behaviour by parents or other reasons. Antibiotic prescribing was more commonplace in the out-of-hours setting, and rates remains high by international standards. This study underlines the importance of ongoing work around GP antimicrobial stewardship, particularly in the out-of-hours setting.
Introduction
Antimicrobial resistance has been labelled a major threat to global public health by the World Health Organisation 1. In Europe 80% of antibiotics are prescribed in the primary care setting, with similar trends seen in Ireland 2. General Practices with lower rates of antibiotic prescription for upper respiratory tract infections (URTI) have not been shown to have higher rates of serious bacterial complications 3. Examining prescribing behaviour in GP services could be useful in reducing potentially inappropriate antibiotic use.
Influences on prescribing patterns in any healthcare setting are multi-factorial, but include setting, patient (or parental) factors and financial pressures [4-11].
Studies on GP antibiotic prescribing patterns in out-of-hours settings in Ireland compared to daytime settings are lacking. However, it has been demonstrated that Irish GPs are more likely to prescribe an antibiotic for urinary tract infections when approaching the weekend 4. A Dutch study has shown that children were more than twice as likely to receive an antibiotic prescription during out-of-hours consultation as compared to a daytime consultation 5.
Patient or parental factors relating to increased antibiotic prescribing include social background 6, lack of education about common viral illnesses 7, previous experience 8, perceived severity of illness 9 and economic considerations 10. Additionally, doctors may misinterpret parental concern or information-seeking as pressure for an antibiotic prescription 11.
In Ireland, just over half the population are not eligible for state-funded care and thus must pay out-of-pocket for visits to their GP 12. In July 2015, the “Under-6 contract” was introduced in an effort to address this inequality for young children 13. This contract granted Doctor Visit Cards (DVCs) to all children under the age of six years, regardless of parental financial means. These patients thus joined the 30% of the under-6 population who already had free access to GP services via their General Medical Services (GMS) card 14. Holders of DVC or GMS cards can attend daytime practices and the out-of-hours services free-of-charge. Reports suggest a 25% increase in visits when children receive free access to GP services 15,16.
We aimed to quantify antibiotic prescription rates and compliance with preferred antibiotic guidelines for URTI presentations and to analyse any factors associated with antibiotic prescription in an Under-6 sample attending Irish daytime and out-of-hours GP services. The time period examined offers an opportunity to examine for changes which may be linked to eligibility for access to services free-of-charge.
Methods
We conducted a cross-sectional study using 2 weeks of anonymised consultation data from January of each for the years 2015, 2016 and 2017. Data was obtained from four providers of daytime and two providers of out-of-hours General Practice services across the Greater Dublin Area.
URTIs were classified according to the ICD-10 criteria i.e. infectious process affecting the upper respiratory tract (nose, paranasal sinuses, pharynx, larynx, or trachea). A review of electronic medical records was completed for patients under 6 years of age presenting with an URTI over the third and fourth calendar weeks of the three included years. Consultation notes were reviewed individually to determine inclusion in this study. This was conducted for all children attending daytime services and a randomized sample (including approximately 50%) of out-of-hours presentations. Data were collected on patient age, gender, medical cover status, type of antibiotic prescription (immediate or deferred) and compliance with Ireland’s national preferred antibiotic guidelines 3.
Trends over time were examined using univariate Poisson regression. Year of sampling was included as the independent variable and trend is reported as incident rate ratios (IRR), which are presented as percentage change per year. Antibiotic prescription, type of prescription and compliance with preferred antibiotic guidelines were considered as dependent variables. Factors associated with prescription were assessed using multivariate logistic regression. Independent variables included in the model were age (over 1 years of age), medical cover (GMS or DVC Cover versus Private Patients), Post 2015 (so as to compare before- and after- introduction of free GP care) and setting (out-of-hours versus daytime settings). Associations are reported as odds ratios (OR) with 95% confidence intervals estimated (95% CI). Analysis was conducted using Microsoft Excel 2007 and Stata 14 IC (Stata Corp, LLC, College Station, TX).
This study was approved by the TCD/HSE GP Training scheme internal ethics committee. Approval was also granted by the relevant out-of-hours service steering committees.
Results
Population Characteristics
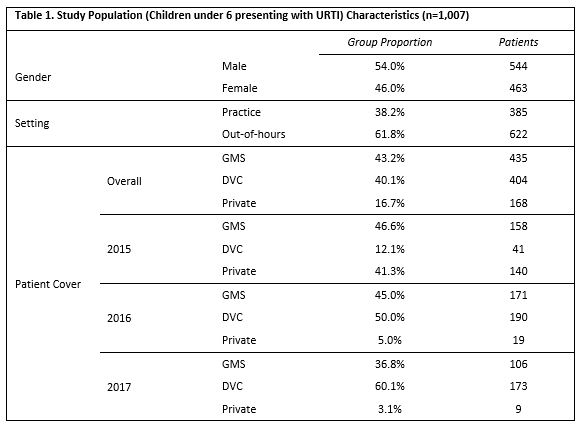
Patients under 6 years of age presenting to a GP with an URTI were included (n = 1,007). The mean age of patients was 2.8 years (SD= 1.6) with females accounting for 46.0% (n = 463). Further details on practice mix and medical cover of patients are provided in Table 1. The large reduction in private patients post-2015 reflects the introduction of the free GP care for all Under-6s.
Antibiotic Prescribing Rates
For the children under 6 who presented with an URTI to daytime services in the 2-week period of 2015, 69.6% were prescribed an antibiotic (Table 2). This fell in 2016 and 2017 to 46.2% and 49.5% respectively. For patients attending the out-of-hours service with an URTI, an antibiotic was prescribed in 72.3% of cases in 2015. In 2016 and 2017, this figure fell to 57.7% and 60.6% respectively.
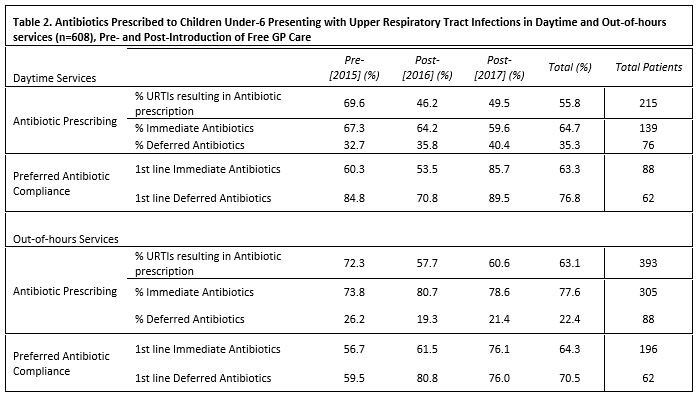
Almost two thirds (64.7%) of antibiotics from daytime services during the study were for immediate use, with 35.3% intended for deferred use. For all antibiotics prescribed in the out-of-hours setting, 77.6% were for immediate use and 22.4% were for deferred use.
Overall daytime compliance with preferred antibiotic guidelines was higher for deferred antibiotics (76.8%), compared to that for immediate antibiotics (63.3%). Compliance with antimicrobial guidelines in the out-of-hours services was 64.3% for immediate antibiotics and 70.5% for deferred antibiotics.
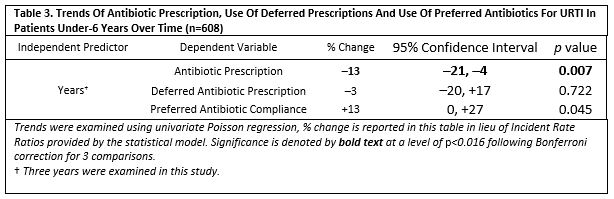
Overall preferred antibiotic guideline compliance increased by 13% (p<0.05) and antibiotic prescriptions decreased by 13% (p<0.01) year-on-year (Table 3). The use of immediate or deferred antibiotics did not change significantly over the three years examined.
Factors Associated with Antibiotic Prescribing
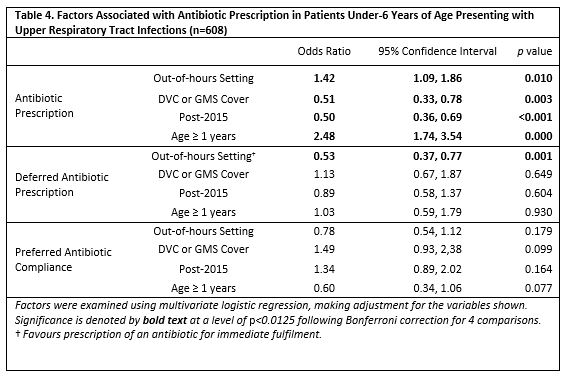
All patients presenting in the two years following the introduction of the free GP care (2016, 2017) were 50% less likely to receive an antibiotic prescription (p<0.001). Patients with DVC or GMS cover were 49% less likely than private patients to receive an antibiotic for an URTI (p=0.03), with no further significant associations.
The out-of-hours setting represented a 42% increased likelihood of antibiotic prescription (p=0.01) (see Table 4). Patients over 1 year old were two and a half times more likely to be prescribed an antibiotic (p<0.001). Patients presenting to the out-of-hours setting were more likely to receive an immediate antibiotic prescription (p=0.001). In this analysis no other factors were significantly associated with deferred prescription type, nor with preferred antibiotic use (Table 4).
Discussion
This cross-sectional study, repeated over three years in the Irish GP setting, showed predictable changes in GP care entitlements of children under-6 following introduction of free GP care. Free GP care was associated with lower antibiotic prescribing rates, with the odds of DVC or GMS patients being prescribed an antibiotic being half that of private patients. As more children gained access to free visits over the study, this in turn led to a clear reduction in antibiotic prescribing rates in both settings. While these prescribing trends are likely multifactorial, we postulate that increased attendance as a result of gaining access to free GP care 4, 5 has led to increased presentation of undifferentiated or more minor illness, thereby facilitating lower prescribing rates. Parental pressure to prescribe may also have been lessened now that care is free at point of use. In any event, GPs are improving standards of antimicrobial stewardship despite increased workload.
Patients attending an out-of-hours setting were more likely to be prescribed an antibiotic, which was expected 17,18. Notably, the only factor clearly associated with immediate antibiotic prescription use was the out-of-hours setting. This may be linked to increased workload pressures, lack of opportunity for follow-up, GPs not knowing the patients and the fact that those who present out-of-hours may be sicker than their daytime counterparts.
Use of deferred antibiotics was a popular strategy amongst GPs in both settings, and compliance with antimicrobial guidelines was generally higher for deferred antibiotics. Compliance with antimicrobial guidelines for preferred first-line agents fluctuated somewhat over the study but comprised a majority of antibiotics at all times. Overall compliance was two-thirds for immediate antibiotics and three-quarters for deferred antibiotics.
Patients over one year-of-age in our sample were more likely to receive an antibiotic prescription. Parents with younger infants may be presenting more readily for review but are less likely to receive antibiotic treatment. Viral bronchiolitis is also a common illness for younger infants. However, this is a novel finding and warrants further exploration.
While overall rates of antibiotic prescribing for URTIs fell over the study, antibiotic prescribing rates remain relatively high 6, with 49.5% of daytime and 60.6% of out-of-hours URTI presentations receiving an antibiotic prescription in the most recent year examined (2017).
This study was strengthened by sampling a large population over a number of different practices in both the daytime and out-of-hours settings. The study was unique in being able to quantify antibiotic prescribing before and after the introduction of free GP care for all children under 6 years. A weakness of our study was that URTI presentation data was only collected for a 14-day period in January for each year, and this may not accurately reflect general antibiotic prescribing trends. However, Ireland is known to be above average in terms of overall antibiotic prescribing in the OECD 7. It was also not possible to determine severity of illness or rationalise individual prescribing decisions from chart review. A number of findings on univariate logistic regression are attenuated by wide confidence intervals.
Antibiotic use fell over the course of the study and overall use of preferred antibiotics seems to be rising. Much progress has been made to date in developing specific public health awareness programmes (e.g. ‘Under The Weather’ campaign 8) and preferred Irish primary care antibiotic guidelines to assist in appropriate use of antibiotics. The most successful interventions to reduce antibiotic prescribing rates in children with URTIs are indeed those which targets both parents and clinicians 7. Continued educational interventions around antimicrobial stewardship, for both patients and GPs, will be critical in years to come if antibiotic consumption, and consequent antimicrobial resistance 7, is to be reduced. The effect of same will likely be attenuated in the out-of-hours setting. Factors affecting prescribing rates here are less likely to be influenced by GP prescribing habits and potentially more dependent on patient factors. Future work in this area should assess factors driving differences in prescribing patterns between settings. It is reasonable to consider that both patient and practice characteristics have differing but related contributions to the data described within this study.
Conflicts of Interest
The authors have no conflicts of interest to declare
Corresponding Author
Dr. Martin Rourke,
Trinity College Dublin/Health Service Executive (TCD/HSE) GP training scheme,
Floor 6,
The Russell Centre,
Tallaght Cross West,
Tallaght,
Dublin 24.
Email: [email protected]
References
1. Laxminarayan R, Matsoso P, Pant S, Brower C, Røttingen JA, Klugman K, Davies S. Access to effective antimicrobials: a worldwide challenge. Lancet 2016;387(10014):168-175.
2. Centre, NDS. A Strategy for the Control of Antimicrobial Resistance in Ireland. 2001.
3. Gulliford, MC, Moore, MV, Little, P, Hay A, Fox R, Prevost T, Juszczyk D, Charlton J, Ashworth M, Safety of reduced antibiotic prescribing for self limiting respiratory tract infections in primary care: cohort study using electronic health records. BMJ 2016;354:i3410.
4. Tandan, M, Duane, S, Vellinga, A. Do general practitioners prescribe more antimicrobials when the weekend comes? Springerplus 2015;4:725.
5. Elshout, G, Kool, M, Van der Wouden, JC, Moll HA, Koes BW, Berger MY. Antibiotic prescription in febrile children: a cohort study during out-of-hours primary care. J Am Board Fam Med 2012;25(6):810-818.
6. Vaz LE, Kleinman KP, Lakoma MD, Dutta-Linn MM, Nahill C, Hellinger J, Finkelstein JA. Prevalence of Parental Misconceptions About Antibiotic Use. Journal of Pediatrics 2015 Aug;136(2):221-31. doi: 10.1542/peds.2015-0883.
7. Cantarero-Arevalo L, Hallas MP, Kaae S. Parental knowledge of antibiotic use in children with respiratory infections: a systematic review. International Journal of Pharmacy Practice 2017, 25, pp. 31–49.
8. Bosley H, Henshall C, Appleton JV, Jackson D. A systematic review to explore influences on parental attitudes towards antibiotic prescribing in children. Journal of Clinical Nursing 2017 Sep 14. doi: 10.1111/jocn.14073.
9. Cabral C, Ingram J, Lucas PJ, Redmond NM, Kai J, Hay AD, Horwood J. Influence of clinical communication on parents’ antibiotic expectations for children with respiratory tract infections. Annals of Family Medicine, March/April 2016 vol. 14 no. 2 141-147.
10. Pichichero ME. Understanding antibiotic overuse for respiratory tract infections in children. Pediatrics 1999;104(6):1384-1388.
11. Cabral C, Horwood J, Hay AD, Lucas PJ. How communication affects prescription decisions in consultations for acute illness in children: a systematic review and meta-ethnography. Bio Med Central Family Practice 2014; 15: 63.
12. Department of Health (DOH). Health in Ireland, Key Trends 2016- Section 4: Primary Care and Community Services. 2017. Available at: http://health.gov.ie/wp-content/uploads/2016/12/Health-in-Ireland-Key-Trends-2016.pdf (accessed 30th November 2017)
13. Health Service Executive (HSE). GP Visit Card for children under 6. HSE Website. 2015. Available at: https://www.hse.ie/eng/services/list/1/schemes/mc/gpvc/under6.html (accessed 12th November 2017).
14. Health Service Executive (HSE). Medical Workforce Planning: Future Demand for General Practitioners 2015-2025. National Doctor Training and Planning, HR Directorate, Health Service Executive, Dr. Steevens’ Hospital, Dublin 8, Ireland. Available at: https://www.hse.ie/eng/staff/leadership_education_development/met/plan/reports/medical_workforce_planning_future_demand_for_general_practitioners_2015-2025.pdf (accessed 30th November 2017)
15. Nolan, A, Layte, R. The impact of transitions in insurance coverage on GP visiting among children in Ireland. Soc Sci Med 2017;180:94-100.
16. O'Callaghan, ME, Zgaga L, O’Ciardha D, O’Dowd T, (2018). "Free Children's Visits and General Practice Attendance." Ann Fam Med 16(3): 246-249.
17. Antimicrobial Guidelines; 2017. http://www.hse.ie/eng/services/list/2/gp/Antibiotic-Prescribing/. Accessed 20th November 2017.
18. Debets VE, Verheij TJ, van der Velden AW. Antibiotic prescribing during office hours and out-of-hours: a comparison of quality and quantity in primary care in the Netherlands. British Journal of General Practice. 2017 Mar;67(656):e178-e186. doi: 10.3399/bjgp17X689641.
P835
