A Dedicated Perineal Clinic – An Audit in Support
E. Corry1, E. O’Connor1, M. Eogan2, M. Fitzpatrick3, S. O’Sullivan4, M. Imcha1
1. University Maternity Hospital Limerick, Ennis Road, Limerick
2. The Rotunda Hospital, Parnell Square, Dublin 1
3. The National Maternity Hospital, Holles Street, Dublin 2
4. Cork University Maternity Hospital, Wilton, Cork
Abstract
Aims
To assess the quality of care in both the initial management of obstetric anal sphincter injury (OASI) and subsequent follow up postnatally in a tertiary maternity hospital without direct access to a perineal clinic.
Methods
Medical records were reviewed over a one-year period in University Maternity Hospital Limerick (UMHL) to determine the characteristics of patients sustaining OASI, how and where the repair was undertaken, the complications recorded and their follow up in the postpartum period. This pathway of care was compared with care currently available in three dedicated perineal clinics nationally.
Results
There were 44 patients with OASI recorded over a one-year period in UMHL. The majority were diagnosed in primiparous women having an operative vaginal delivery (OVD). Only 23 of 44 women had a documented review postnatally.
Conclusion
Audit of OASI is paramount to providing the best standard of care for affected women. It also aids clinician training and will be important in the establishment of a dedicated perineal clinic in UMHL.
Introduction
The rate of Obstetric Anal Sphincter Injury (OASI) has increased significantly in the last decade, having risen in England from 1.8% to 5.9% from 2000 to 2012.1 The impact of OASI on mode of delivery has been demonstrated both nationally and internationally, with one study suggesting 25-30% patients opt for elective caesarean section (CS) in the subsequent pregnancy.2, 3 Review at a dedicated perineal clinic provides a critical component in the assessment and management of OASI and discussion around future mode of delivery.4 There are currently three perineal clinics in the Republic of Ireland that review and assess recovery post-OASI and advise on future mode of delivery following OASI.5
We undertook an audit of management of OASI and subsequent postpartum follow up in UMHL, a large tertiary maternity hospital with more than 4,500 deliveries per year. The genesis of the study was a significant rise in the rate of recorded OASI the previous year. The aim of the study was to assess the quality of care and complications associated with OASI in our unit as well as to assess follow up care in a large maternity unit without a perineal clinic, where postpartum assessment is based on clinical history and examination only. Following this audit, the pathway of care in each of the three existing perineal clinics was reviewed to determine the resources required and the appropriate standard of care for the establishment of a perineal clinic in our institution.
Methods
We performed an audit of OASI in our unit over a 1-year period from July 2015 to July 2016. The medical records of all OASI recorded in the hospital electronic database were reviewed. To determine the quality of care delivered to women post-OASI in UMHL all aspects of the surgical repair and corresponding care were assessed. The obstetric characteristics of those who had OASI were recorded. The quality of care for the management of OASI was then reviewed, including markers such as the technique, location and material used for OASI repair, any post-repair complications and subsequent follow up of the patients. To determine a model of care appropriate for the establishment of a dedicated perineal clinic in our institution, we reviewed the three existing perineal clinics nationally, examining the different pathways within each clinic and the resources available for each unit for the assessment and care of patients' post-OASI.
Results
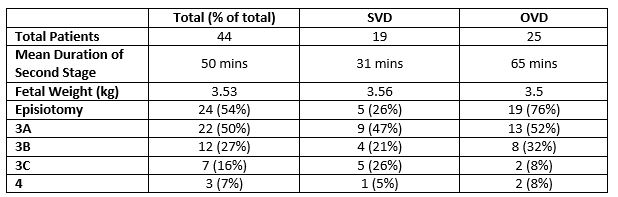
Over the 1-year period of the audit there were 44 recorded patients who sustained OASI during delivery. Of these, 33 were in primiparous women and 11 in multiparous women (one of whom had a VBAC with no previous vaginal deliveries). Twenty-five women (57%) were delivered by operative vaginal delivery (OVD), with 20 patients delivered by ventouse, 4 patients delivered by forceps and 1 patient requiring a “double instrumental” delivery (i.e. ventouse and forceps). Nineteen (76%) patients requiring an instrumental delivery had an episiotomy; of the nineteen (43%) patients who had a spontaneous vaginal delivery (SVD), five women (26%) also had an episiotomy. Of the OVD group, the primary indication for delivery was suspected fetal distress in sixteen women (64%). Nine women (36%) had an OVD for prolonged second stage of labour and twenty (80%) women in this group were delivered by ventouse. These characteristics are outlined in Table 1.
Table 1
The technique and material used for repair are outlined in Table 2. The primary location for the repair was the operating theatre, however a significant proportion (34%) were repaired in the labour ward. Of the group who had OASI repaired in the labour ward, 73% (11/15) had a 3A tear and 27% (4/15) had a 3B tear. Thirteen women (13/15, 87%) of this group had the repair performed by a consultant. Of those who had OASI repair in the LW one patient had an immediate post-repair complication (breakdown and re-suturing of the repair) and one patient had ongoing flatal incontinence at the 6-week review. All 44 patients received antibiotic prophylaxis.
Table 2
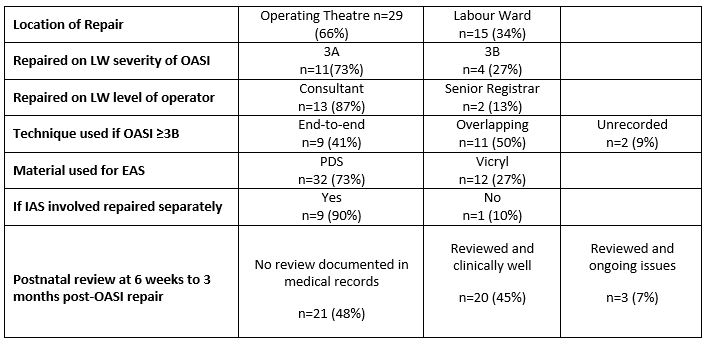
Only one patient had an immediate post-repair complication (breakdown and re-suturing of the repair). Postpartum review occurred between six weeks and three months after OASI repair. The documented ongoing complication rate was low, with three patients having (documented) ongoing issues. One patient had stitch protrusion from the repair site. Two patients had persistent flatal incontinence, and one of these patients had reduced anal tone on digital examination. A large proportion of patients (48%) had no documentation in the medical records of assessment between six weeks and three months postpartum.
Discussion
The primary aim of this audit was to assess the quality of care delivered to women experiencing OASI, as well as review the current evidence available in this area. When examining causation, the majority of our patients with OASI had an OVD with a significant proportion also having a second recognised risk factor as the mean duration of the second stage of labour in this group was >60 mins.6 Significantly, 24% of the population who sustained an OASI following an OVD did not have a right mediolateral episiotomy performed during the delivery. While it must be recognised that each delivery requires individual assessment for the need for episiotomy, the evidence does reflect the potential benefits of correctly angled episiotomies in reducing the incidence of OASI.7, 8
The almost equal numbers of repair technique for 3B (or greater) tears (Table 2) is perhaps reflective of the evidence that there are no significant long-term differences in outcomes between the end-to-end vs overlapping techniques of repair.9, 10 The national clinical guideline for the management of OASI suggests that repair is best undertaken in the operating theatre.11 While a larger than expected number of patients in our population had the repair undertaken on the labour ward, the clinician assessing the appropriate location of repair was a consultant in almost all cases. None of these cases were more than a grade 3B tear. A limitation of this audit is that it does not reflect the dynamic nature of the labour ward, which may have had a critical impact on issues such as the location and timing of repair of OASI.
When looking at wound management, 100% adherence to antibiotic prophylaxis following repair in this population is reassuring given the current evidence for risk reduction for infection with appropriate antibiotic therapy.12 The most striking finding from this audit was the lack of documented follow up post-OASI repair, with 48% of patients having no documented follow up assessment in their maternity record. Some of this may be explained by a proportion of patients conducting their post-partum follow up with their consultant outside of the hospital setting. However, it still poses a significant barrier to audit of complications and assessing perineal care in the hospital.
All patients post OASI in our institute have an inpatient physiotherapy review prior to discharge and a further appointment, six weeks after discharge with further follow-up arranged if required. Obstetric review is provided by the consultant under whose care the patient was booked antenatally. Review is usually performed at that consultant’s antenatal clinic as many of the gynaecology clinics are in peripheral centres.
The absence of a dedicated perineal clinic in a location within the hospital amenable to mothers with young infants and a single consultant reviewing this cohort of patients creates potential barriers to ongoing follow up and audit of care. This challenge in ensuring a consistent pathway of care with a unified multidisciplinary approach is faced internationally.13 The clear benefits of a dedicated perineal clinic are multiple, allowing consistency in assessment and follow up of OASI, reduction in morbidity from OASI, facilitating appropriate investigations where indicated, and enable advice to be given for future mode of delivery. Audit of the detection, management and outcomes of OASI in the unit contribute both to internal monitoring of standards and ongoing research in the area.4, 14, 15 Variation in rates of OASI between hospitals can be significant and highlights the need for close surveillance to ensure detection and the need to retain rates of OASI as a marker of quality of care delivered to obstetric patients.16 A perineal clinic provides the opportunity for review (where appropriate) of rising incidence of OASI within a hospital, and to provide a defined standard of care. An increasing incidence of OASI may also be due to over diagnosis; a perineal clinic provides the opportunity for re-training where appropriate.17
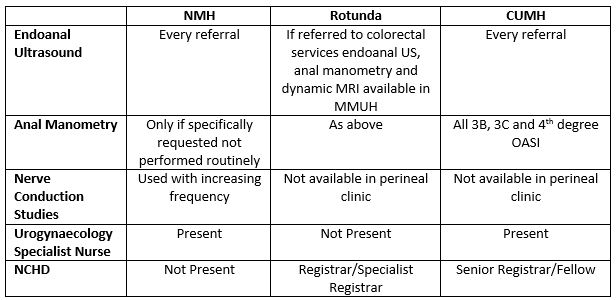
When highlighting the potential benefits of the establishment of a perineal clinic in UMHL, it is important to consider the existing models nationally. While each of the existing perineal clinics has a different care pathway, all provide an essential focal point of care for patients following a traumatic event, and lead to safe, effective, timely, efficient, equitable and person-centred care - the six dimensions of healthcare quality18.
There are slightly different resources available to each of the three clinics, this is demonstrated in Table 3. OASI alone is not the sole indication for referral, highlighting their overall contribution to postnatal care. While the investigations performed in each clinic may vary, an integral component of the clinics is the presence of a clinician with expertise in OASI, which is critical for the provision of high quality care. These clinics form a template for the establishment of a perineal clinic in the mid-western region.
Table 3
The continued audit of OASI provides both reassurance of the standard of care delivered and opportunities for early detection of potential contributory factors to OASI where intervention in the form of training may be beneficial. The absence of a dedicated perineal clinic is an impediment to postnatal follow-up and auditing of postnatal complications. The existing perineal clinics nationally provide evidence for the establishment of a dedicated perineal clinic within a maternity unit to ensure the best standard of care for affected women.
Conflict of Interest:
The authors of this article do not perceive any conflict of interest with the article.
Corresponding Author:
Emily O'Connor
University Maternity Hospital Limerick,
Ennis Road,
Limerick
Email: [email protected]
References
1. Gurol-Urganci I, Cromwell DA, Edozien LC, Mahmood TA, Adams EJ, Richmond DH, Templeton A, Van der Muelen JH. Third- and fourth-degree perineal tears among primiparous women in England between 2000 and 2012: time trends and risk factors. BJOG : an international journal of obstetrics and gynaecology. 2013;120(12):1516-25.
2. Edozien LC, Gurol-Urganci I, Cromwell DA, Adams EJ, Richmond DH, Mahmood TA, Van der Muelen JH. Impact of third- and fourth-degree perineal tears at first birth on subsequent pregnancy outcomes: a cohort study. BJOG : an international journal of obstetrics and gynaecology. 2014;121(13):1695-703.
3. Fitzpatrick M, Cassidy M, Barassaud ML, Hehir MP, Hanly AM, O'Connell PR, O'Herlihy C. Does anal sphincter injury preclude subsequent vaginal delivery? European journal of obstetrics, gynecology, and reproductive biology. 2016;198:30-4.
4. Fitzpatrick M, Cassidy M, O'Connell PR, O'Herlihy C. Experience with an obstetric perineal clinic. European journal of obstetrics, gynecology, and reproductive biology. 2002;100(2):199-203.
5. Gynaecologists IoOa. Irish Guidelines for Management of Obstetric Anal Shincter Injury,Guideline No. 8. 2011.
6. Donnelly V, Fynes M, Campbell D, Johnson H, O'Connell PR, O'Herlihy C. Obstetric events leading to anal sphincter damage. Obstetrics and gynecology. 1998;92(6):955-61.
7. Eogan M, Daly L, O'Connell PR, O'Herlihy C. Does the angle of episiotomy affect the incidence of anal sphincter injury? BJOG : an international journal of obstetrics and gynaecology. 2006;113(2):190-4.
8. Kapoor DS, Thakar R, Sultan AH. Obstetric anal sphincter injuries: review of anatomical factors and modifiable second stage interventions. International urogynecology journal. 2015;26(12):1725-34.
9. Fernando RJ, Sultan AH, Kettle C, Thakar R. Methods of repair for obstetric anal sphincter injury. The Cochrane database of systematic reviews. 2013(12):Cd002866.
10. Fitzpatrick M, Behan M, O'Connell PR, O'Herlihy C. A randomized clinical trial comparing primary overlap with approximation repair of third-degree obstetric tears. American journal of obstetrics and gynecology. 2000;183(5):1220-4.
11. and IoOaG, Directorate of Clinical Strategy and Programmes, Executive HS. Guideline Number 8 : Management of Anal Sphincter Injury. Clinical Practice Guideline. 2014.
12. Buppasiri P, Lumbiganon P, Thinkhamrop J, Thinkhamrop B. Antibiotic prophylaxis for third- and fourth-degree perineal tear during vaginal birth. The Cochrane database of systematic reviews. 2010(11):Cd005125.
13. Priddis HS, Schmied V, Kettle C, Sneddon A, Dahlen HG. "A patchwork of services"--caring for women who sustain severe perineal trauma in New South Wales--from the perspective of women and midwives. BMC pregnancy and childbirth. 2014;14:236.
14. Fowler G, Williams A, Murphy G, Taylor K, Wood C, Adams E. How to set up a perineal clinic. The Obstetrician & Gynaecologist. 2009;11(2):129-32.
15. Pretlove S, Thompson PJ, Toozs-Hobson PM, Radley S. The first 18 months of a new perineal trauma clinic. Journal of obstetrics and gynaecology : the journal of the Institute of Obstetrics and Gynaecology. 2004;24(4):399-402.
16. Baghurst PA. The case for retaining severe perineal tears as an indicator of the quality of obstetric care. The Australian & New Zealand journal of obstetrics & gynaecology. 2013;53(1):3-8.
17. Sioutis D, Thakar R, Sultan AH. Overdiagnosis and rising rate of obstetric anal sphincter injuries (OASIS): time for reappraisal. Ultrasound in Obstetrics & Gynecology. 2017;50(5):642-7.
18. Institute of Medicine Committee on Quality of Health Care in A. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC): National Academies Press (US)
Copyright 2001 by the National Academy of Sciences. All rights reserved.; 2001.
P913
