A Response to: “A Cluster of Paediatric Invasive Group A Streptococcal and Chicken Pox Infections”
Cassidy A, McBrien J
General Paediatrics Department, Children’s University Hospital, Temple Street, Dublin 1
Dear Sir,
We read with interest the recent article “A Cluster of Paediatric Invasive Group A Streptococcal and Chicken Pox Infections”, Ó Maoldomhnaigh et al published in your March 2018, Volume 111, No 3 edition. Hospitalisation with chickenpox is a notifiable disease to the Health Protection Surveillance Centre (HPSC).
We have identified another cluster of children with complications secondary to Varicella Zoster Virus (VZV) infection. Thirteen children were admitted to the Children’s University Hospital, Temple Street (CUHTS) between January and July 2017 (the year following Dr Ó Maoldomhnaigh’s research) as a result of complications of chickenpox infection. Five of these children were male. The ages ranged from 27 weeks to 7 years (mean=2.1 years, median=1.5 years). All of these children were previously well, with no history of immunodeficiency.
The complications are outlined in the table below (patients may have had multiple):
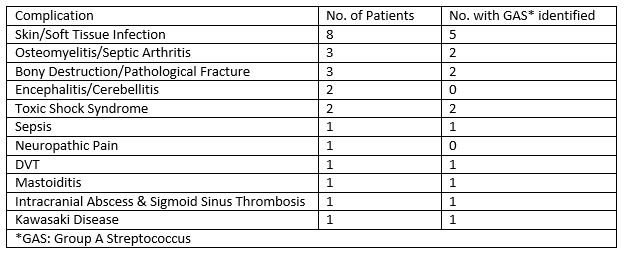
The length of time from VZV infection to onset of complication ranged from no history of chickenpox (but VZV identified on CSF PCRs) to 17 days after the rash had crusted over (mean=6 days, median=4.5 days). Six children (46%) had Group A Streptococcus identified as a causative organism for their complication.
The length of hospital stay ranged from 1 day to 27 days (mean=9.3, median=6) with one patient requiring readmission for a further day. One child was admitted to PICU for 9 days. Three children required PICC line insertion. Four patients required >6 weeks of antibiotics (2 oral, 2 IV). Two patients required surgery (orthopaedic, ENT and neurosurgery), while a total of 5 patients required Surgical Team input (orthopaedic, ENT and neurosurgery). All patients had commenced the routine vaccination schedule but none had received the VZV vaccine. All of these children have required varying levels of outpatient follow up and treatment.
Ó Maoldomhnaigh et al reported 10 children with invasive Group A streptococcal infection, 7 of whom had active VZV infection who presented to CUHTS in 2016. A year later in the same hospital we are reporting 13 children who required hospitalization as a result of a complication of VZV infection, 6 of whom had invasive group A streptococcal infection. In Ireland, VZV vaccine is not part of the universal childhood immunization. While the majority of VZV cases are mild and self-limiting, there is significant patient morbidity and healthcare costs associated with severe or complicated varicella infections. Permanent disability occurs particularly with intracranial and orthopaedic complications. There is an added economic impact for parents taking time off work to be with their sick child. We agree with the authors of the IMJ article that universal VZV vaccination needs to be reconsidered.
Conflicts of Interest
The authors have no conflicts of interest to declare
Corresponding Author
Dr Aoife Cassidy,
General Paediatric Department,
Our Lady’s Children’s’ Hospital,
Crumlin,
Dublin 12
Email: [email protected]
P847
