A Review of the Parenteral Nutrition Supply Service in an Irish Neonatal Unit
Smith A1, Glynn AC 2, Shankar A 3, McDermott C 1& McCallion N 1,3
1. Department of Neonatology, The Rotunda Hospital, Dublin
2. Clinical Nutrition and Dietetics service, The Rotunda Hospital, Dublin
3. Department of Paediatrics, Royal College of Surgeons in Ireland, Dublin 2
Abstract
Background
Neonatal Intensive Care (NICU) patients have individual nutritional requirements often requiring Patient Specific Parenteral Nutrition (PSPN). From October 2015, the national PSPN compounding service availability changed from 7 days per week service to 5 days per week (i.e. no weekend and limited bank holiday ordering available). The aim of this study was to examine the introduction of a 5 day only PSPN supply on neonatal patient parenteral nutrition availability in a tertiary NICU.
Methods
We performed a prospective assessment of the provision of a 5 day rather than 7 day ordering of PSPN over a one month period (June 2017).
Results
Fifteen neonatal patients received a cumulative 89 days of PN during June 2017. 10 (66%) patients received PSPN during this time period. There was same day availability of PSPN in 62 of 89 days of PN (69%).
Conclusion
Thorough education and training will help prescribers to make appropriate PSPN ordering decisions. Improvements to available stock bags may reduce the amount of PSPN that is required but a 7 day PSPN ordering service would improve efficient provision of clinically indicated PSPN to premature infants in NICU in Ireland.
Introduction
Major advancements have been made in provision of neonatal care and neonatal outcomes in recent years, most especially a significant increase in survival without major neonatal morbidity for infants born between 25 and 28 weeks gestation1,2. The ability to provide adequate nutrition during the vulnerable early postnatal period has been pivotal in achieving such improved outcomes3, 4. A study by Ehrenkranz et al found that ‘Compared with more critically ill infants, less critically ill infants received significantly more total nutritional support during each of the first three weeks of life, had significantly faster growth velocities, less moderate to severe bronchopulmonary dysplasia, less late-onset sepsis, less death and shorter hospital stays’5. The developing brains of premature infants are exquisitely sensitive to then nutritional milieu to which they are exposed. Very and extremely low birth weight infants are at high risk of malnutrition and postnatal growth restriction which can lead to inadequate brain development and poor neurodevelopmental outcomes in later life5-7. A 2017 study assessing adults who were born very preterm or with very low birth weight identified PN as one significant modifiable factor which was ‘strongly related to adult IQ’8. Therefore, optimizing the nutrition provided to neonates who cannot achieve their full nutritional requirements enterally, due to gastrointestinal immaturity or malfunction, is central to enhancing their long term neurodevelopmental potential9.
In the Rotunda Hospital, the general indications for prescribing and ordering PN are as follows; infants born <1,500g and <32 weeks gestation, infants receiving nil or minimal enteral feeding for 2-3 days and infants advancing enteral feeds by <30ml/kg/day (both PSPN and Stock PN are available in the Appendices). PSPN is often required because of electrolyte imbalance e.g. hyponatraemia requiring increased sodium, glucose imbalance e.g. hyperglycaemia required reduced glucose infusion rate, non-standard macronutrient requirement e.g. increased amino acids requirements for extremely low birth weight infants, trace element requirement and for the provision of acetate e.g. to help correct metabolic acidosis.
Very premature and low birth weight infants can be very clinically unstable at times with widely fluctuating fluid and electrolyte requirements that are subject to significant individual variation and so are difficult to predict. Therefore, it should be determined daily if PN is required to provide ideal macronutrients, micronutrients, electrolytes and trace elements in order to meet the individual requirements of premature babies in particular10. In October 2015, daily, 7-day per week, ordering of PSPN based on 24-hourly blood results and fluid balances was reduced to a 5-day per week PN compounding service (with no weekend or bank holiday ordering service). Where PSPN was required, it was pre-ordered for weekend and holiday days during the working week, using estimated potential infant requirements. Where infants are delivered at the weekend or on bank or public holidays, stock standard bags of PN were used to try to meet patient requirements. Stock PN has the advantage of being pre-prepared and once indicated can be immediately administered to ensure nutrient delivery is not delayed. However stock PN may not meet the amino acid, glucose, electrolyte or micronutrient requirements of the low birth weight infant and thus it is generally used on a short term basis. A retrospective audit of the first 14 months of the initial phase of this service, during which 815 PSPN bags were ordered, identified issues with delays or availability of ordered PSPN in 15 cases. As these results could have been influenced by a staff learning curve during the introduction of new 5-day prescribing practices, a prospective study was designed. This study aimed to prospectively examine the direct impact on PSPN availability and clinical service of a 5-day PSPN ordering service.
Methods
We performed a prospective assessment of PN availability and requirements for modification of fluid, nutritional and electrolytes arising from pre-ordering PSPN and the provision of a 5 rather than 7-day ordering of PSPN to the neonatal unit over the month of June 2017. This was a prospective assessment of PSPN supply to the Rotunda Hospital neonatal unit from June 1st to June 30th 2017. The Rotunda is a tertiary referral centre for neonatal patients with a birth rate of approximately 9,000 babies per annum. All infants in receipt of PN during this time frame were eligible for inclusion. Data was collected by one neonatal physician and a neonatal dietitian. Data points collected included total number of days on PN, type of PN (stock PN or PSPN), the necessity for additional intravenous (IV) infusions and glycaemic or electrolyte modifications, IV cannulation and phlebotomy, PSPN same day availability and delays in PN delivery.
Results
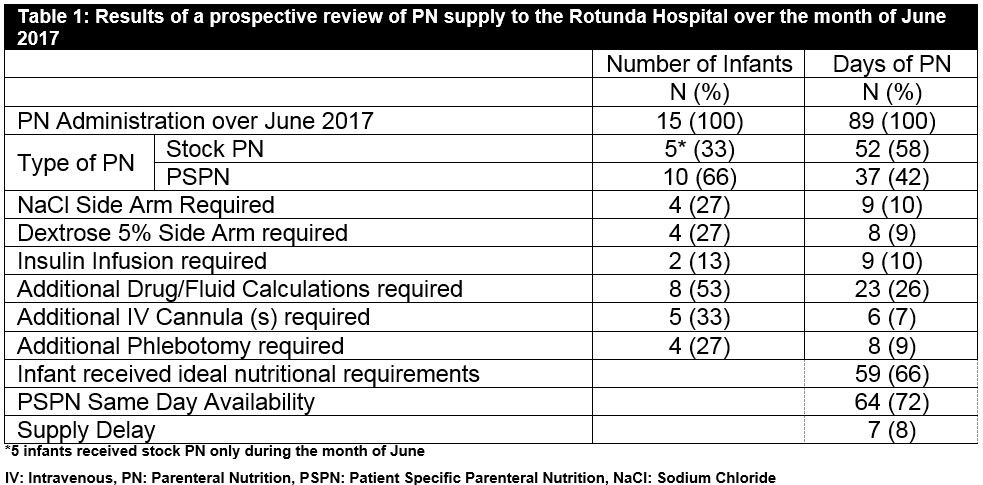
The results of our prospective review of PN supply are displayed in Table 1. Fifteen neonatal patients received a total of 89 days PN in the Rotunda Hospital during the month of June 2017. Five infants (33%) received stock PN only and 10 (66%) patients received PSPN during this time period. Of the cumulative 89 days of PN administered, 52 (58%) days were stock PN and 37 (42%) were PSPN. There was same day availability of PSPN in 62/89 (69%) days of PN. When PN does not meet the real-time fluid, glycaemic or electrolyte requirement of these complex intensive care patients, additional intravenous fluid infusions and electrolyte infusions, known as “side arms”, are required. There was concern that increased use of non-individualised stock PN or TPN ordered well in advance of use would lead to increased use of “side-arm” infusions in order to meet each infant’s nutritional, electrolyte and fluid requirements. Over the month of June, side arms of sodium chloride (NaCl) were required in four (27%) patients, or on 9 (10%) of the 89 days of overall PN use. Anecdotally, side arms of other supplemental electrolytes such as potassium and calcium infusions have been required to help correct hypokalaemia and hypocalcaemia when PSPN was not available in our unit; however this was not found during our one-month prospective study. Additional Dextrose 5% was also required in four (27%) neonates or a total of 8 (9%) of the 89 days of PN provision.
Premature neonates frequently have labile blood sugar levels and insulin is often necessitated to regulate this. The glucose concentration may be modified in PSPN to the infants particular needs, however where PSPN is not available insulin may be required to control blood sugar levels while in receipt of the standard glucose concentration stock PN. Over the month of June, two (13%) infants required insulin for a total of 9 (10%) PN days. Same day delivery of PSPN was available for most days when insulin was required bar one 24 hour period where it was not available. With the necessity to provide side arms and insulin infusions to specific infants, additional fluid and drug calculations were required when nursing staff prepared the fluids and set the infusion pumps. Eight (53%) neonates required additional calculations for side arms and insulin to be administered over 23 (26%) of the 85 days of PN provision. In order to administer side arms additional intravenous (IV) cannulas may be required. Additional IV cannulas were necessary in 5 (33%) infants during June in order to administer their requisite side arm IV infusions over 6 (7%) of the total PN days. Additional phlebotomy, directly related to monitoring electrolytes while in receipt of side arm infusions, was required in four (26%) infants over 8 (9%) PN days.
The same day supply of PSPN was available to the Rotunda on 62 (69%) days of PN during June. A delay in the PSPN supply was noted on 7 (8%) days. A delay was defined as delivery of PSPN after 7pm in the evening. While a delay in the delivery of PSPN was not overtly detrimental to neonatal nutrition it does affect staff workload and efficient administration of PSPN. Table 1:
Discussion
The provision of optimum nutrition to developing premature infants is essential. Ensuring nutritional integrity is vital for both establishing adequate neonatal growth and protection from future morbidity and neurodevelopmental impairment11. The lack of an ideal national 7 day service PSPN service (covering weekends and bank holidays) raises many issues. This five day only system necessities ordering a three to four day supply of PN each Friday to cover patients over weekends and/or bank holidays. At specific times, e.g. Christmas and other holiday periods, prescribing happens several days in advance of administration based on a best estimate of patient requirements. Due to the often rapid changes in a neonate’s specific nutritional, fluid and electrolyte requirements, particularly in the smallest and most immature babies, it is not uncommon that pre-ordered PN bags may no longer be suitable for the patients’ needs by delivery and must either be discarded or clinical management manipulated. This study did not attempt to quantify the costs associated with PN bags which were no longer suitable for individual patient use on the prescribed day, or of additional staff time or resources required to meet patient nutritional and electrolyte requirements in real time.
Our prospective, one month review provides a snapshot into the effect of 5 rather than 7 days PSPN ordering in the NICU. It quantifies for the first time the use of side arms of various fluids and electrolytes to meet patient needs, the use of insulin where glycaemic input cannot be modified and the additional intravenous access requirements. Extra IV cannulation may be required, and removal of temporary central IV access (such as umbilical venous catheters) may be delayed. Extra phlebotomy and blood glucose monitoring may be required. Every side arm of fluids introduces a potential risk of medication or administration error of fluids and medications, despite best safety practices; however no adverse events were noted during this study. Indeed, neonates are a high risk patient population recognised as prone to medication prescribing and administration error12. Compensatory measures due to a 5 day PSPN service also lead to an increased workload for staff and accrue a financial burden for the hospital.
Limitations of this study are that it was conducted over a one month period, where a longer study might have shown variability in the results obtained. A larger, multicentre study conducted over a longer time frame would provide valuable data on this topic. However, the short epoch studied allowed a rapid analysis of data, ensuring relevance to current clinical practice.
The provision of PSPN is a national issue affecting all Irish neonatal units. Over 70,000 infants are delivered annually in Ireland. Six hundred and twenty-two infants were born in Ireland weighing less than 1,500g at birth in 2015, a cohort for whom early and tailored nutrition is vital13. Premature infants are a vulnerable population whose future neurodevelopmental outcome and overall prognosis is directly influenced by early nutrition. Providing optimum nutrition is multifactorial and may be influenced by many issues including the infant’s current clinical status. Thorough education and training will help prescribers to make sensible PSPN ordering decisions. Improvements to available stock bags may reduce the amount of PSPN that is required and progressing enteral feeds at faster rates can reduce PN requirements overall. However, increased system responsiveness to allow prescribing based on the real-time, current clinical condition of very low birth weight infants through the use of a 7-day PSPN service would be key to ensuring that all premature infants born in Ireland are afforded the best possible start in life.
Corresponding Author:
Aisling Smith, The Rotunda Hospital, Parnell Square, Dublin
Email: [email protected]
T: +353 877838119
Conflict of Interest
The authors have no conflicts of interest to declare.
References
1. Soll RF. Progress in the Care of Extremely Preterm Infants. JAMA. 2015;314(10):1007-8.
2. Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, Laptook AR, Sanchez PJ, Van Meurs KP, Wyckoff M, Das A, Hale EC, Ball MB, Newman NS, Schibler K, Poindexter BB, Kennedy KA, Cotten CM, Watterberg KL, D'Angio CT, DeMauro SB, Truog WE, Devaskar U, Higgins RD. Trends in Care Practices, Morbidity, and Mortality of Extremely Preterm Neonates, 1993-2012. Jama. 2015;314(10):1039-51.
3. Adamkin DH, Radmacher PG. Current trends and future challenges in neonatal parenteral nutrition. Journal of neonatal-perinatal medicine. 2014;7(3):157-64.
4. Harding JE, Cormack BE, Alexander T, Alsweiler JM, Bloomfield FH. Advances in nutrition of the newborn infant. Lancet (London, England). 2017;389(10079):1660-8.
5. Ehrenkranz RA, Das A, Wrage LA, Poindexter BB, Higgins RD, Stoll BJ, Oh W. Early nutrition mediates the influence of severity of illness on extremely LBW infants. Pediatric research. 2011;69(6):522-9.
6. Embleton NE, Pang N, Cooke RJ. Postnatal malnutrition and growth retardation: an inevitable consequence of current recommendations in preterm infants? Pediatrics. 2001;107(2):270-3.
7. Stephens BE, Walden RV, Gargus RA, Tucker R, McKinley L, Mance M, Nye J, Vohr BR. First-week protein and energy intakes are associated with 18-month developmental outcomes in extremely low birth weight infants. Pediatrics. 2009;123(5):1337-43.
8. Breeman LD, Jaekel J, Baumann N, Bartmann P, Wolke D. Neonatal predictors of cognitive ability in adults born very preterm: a prospective cohort study. Developmental medicine and child neurology. 2017;59(5):477-83.
9. Belfort MB, Ehrenkranz RA. Neurodevelopmental outcomes and nutritional strategies in very low birth weight infants. Seminars in fetal & neonatal medicine. 2017;22(1):42-8.
10. HSE. Guideline on the Use of Parenteral Nutrition in Neonatal and Paediatric Units. 2016.
11. Hay WW. Optimizing nutrition of the preterm infant. Zhongguo dang dai er ke za zhi = Chinese journal of contemporary pediatrics. 2017;19(1):1-21.
12. Pawluk S, Jaam M, Hazi F, Al Hail MS, El Kassem W, Khalifa H, Thomas B, Abdul Rouf P. A description of medication errors reported by pharmacists in a neonatal intensive care unit. International journal of clinical pharmacy. 2017;39(1):88-94.
13. Centre NPE. Very Low Birth Weight Infants in the Republic of Ireland. 2015.
(P778)
