A Survey of Colorectal Cancer Surveillance Practices In Ireland, And Implementation of A Survivorship Care Plan Pilot Programme
M. Greally1,2, F. Keane1, D.G. Power3, G.D. Leonard1
1. Medical Oncology Department, University Hospital Galway, Galway.
2. Gastrointestinal Oncology Service, Department of Medicine, Memorial Sloan Kettering Cancer Center, New York, United States.
3. Medical Oncology Department, Cork and Mercy University Department, Cork.
Abstract
Aims
The number of colorectal cancer (CRC) survivors in Ireland is rising. We aimed to survey current surveillance practices and pilot the use of survivorship care plans (SCPs) in the clinic.
Methods
An online survey was issued to medical oncologists (MOs) in designated cancer centres (DCC) and satellite centres. The SCP was piloted in CRC patients and a follow-up questionnaire assessing their views was issued.
Results
Responses from 8 DCC and satellite centres were obtained (n=13). Routine surveillance is practiced by 77% (n=10) and 69% (n=9) believe that the MO clinic is inappropriate for follow-up. Most think that the SCP is useful and that ANP-led surveillance clinics should be introduced. Of 16 patients who replied to the survey, most felt that the SCP was beneficial. Sixty-two percent (n=10) were agreeable to GP follow-up using the SCP.
Conclusion
Surveillance practices in Ireland are heterogeneous. The SCP may be useful for streamlining follow-up practices nationally.
Introduction
Colorectal cancer (CRC) is the second most common cancer in men and women in Ireland1. The number of CRC survivors is increasing, due to rising incidence1, earlier detection and improved treatment. As survival can be increased with metastasectomy there is a role for surveillance of early stage disease.2-4 There are approximately 150,000 cancer survivors in Ireland, equivalent to 3% of the population, and at the end of 2014, 17,136 people were living with a history of CRC.5 These numbers are projected to rise, with implications for health service planning. Given the current shortage of medical oncologists (MOs) and advanced nurse practitioners (ANPs) in Ireland when compared to the Organisation for Economic Co-operation and Development (OECD) averages, integration of high quality survivorship care into our clinical practice will be challenging.6
The impact of a CRC diagnosis on health and quality-of-life (QoL) is not insignificant, particularly as interventions have become more complex over time. Although many survivors maintain a good QoL without significant cancer related symptoms, many are at risk of multiple survivorship issues and late side effects.7,8 It is recognised by American Society of Clinical Oncology (ASCO) and National Comprehensive Cancer Network (NCCN), that survivorship is a distinct phase along the cancer care continuum9,10.
The 2005 Institute of Medicine report in the United States (US) described four components of survivorship care: cancer prevention, surveillance for recurrence, interventions for long-term and late effects from cancer and its treatment and coordination between specialists and primary care to ensure the survivors needs are met.11 Currently, CRC survivors in Ireland may encounter fragmented care, often with a disconnect between specialist and primary care services. In addition, surveillance practices in Ireland are heterogenous and there is variability in the guidelines from expert groups. Survivorship care plans (SCPs) have emerged as a potential tool for aiding survivorship and follow-up care. They include a treatment summary and follow-up care plan for patients as they transition out of acute cancer care. While broadly endorsed by professional and advocacy organisations their adoption remains limited and only 20% of oncologists routinely provide SCPs in the US.12
The recently published National Cancer Strategy (NCS) has recognized the need to enhance survivorship care in Ireland.13 A key objective set out in the strategy is to offer patients a treatment summary and SCP, with a target of achieving this goal in 95% of patients by 2020. It was also recommended that the National Cancer Control Programme (NCCP) in conjunction with the cancer centres, develop shared care protocols for patients following treatment to span the hospital and primary care settings. Streamlining of surveillance care in concert with use of SCPs may be an effective strategy for follow-up of patients with CRC and allow health-care professionals (HCP) other than MOs to play a more significant role.
In this study, we aimed to assess current surveillance practices in Ireland and perform a pilot implementation of SCPs into our CRC clinic to assess its usefulness as a tool for streamlining follow-up practices.
Methods
The NCCP has 8 designated cancer centres (DCC) which encompass associated satellite centres. We issued an electronic survey to a gastro-intestinal (GI) malignancy focused medical oncologist (MO) in each of the 8 centres and satellite centres. The survey addressed surveillance practices, use of guidelines and future strategies for follow-up.
Secondly, we piloted use of the SCP in our GI focused MO clinic. We identified patients who had completed treatment for CRC (surgery, chemotherapy +/- radiotherapy) and provided a standardised ASCO treatment summary and SCP for CRC (Appendix 1).
With patient consent, we provided education on the treatment summary and SCP and recommended it be kept with their health records. The SCP was sent to the GP, filed in the patient’s medical chart and onto the oncology information technology system. At an interval of 3 months following receipt of the SCP, patients were sent a questionnaire regarding their views on the contribution of the SCP to their follow-up care.
Results
Part 1
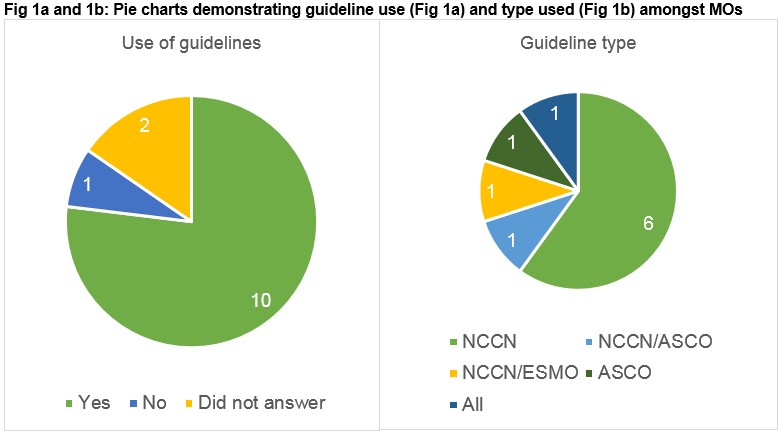
We obtained thirteen replies to our electronic survey, representing all DCCs and a selection of satellite centres. Routine surveillance of CRC is practiced by 77% (n=10) of MOs while 23% (n=3) do not perform follow-up. Of the MOs who do practice follow-up, 90% (n=9) do so for 5 years. Guidelines for follow-up are utilised by 77% (n=10) of respondents (Fig 1a). Of MOs who use guidelines, 60% (n=6) solely use NCCN guidelines while others used a combination of ASCO, ESMO and NCCN (Fig 1b). Sixty-two percent (n=8) reported their intention to adopt NCCP guidelines when published.
When asked about the appropriate channel for surveillance, 75% (n=9) do not believe that the MO clinic is the optimal mechanism for follow-up and survivorship care. Furthermore, 53.8% (n=7) believe that patients should be discharged from the MOC to an alternative mode of follow-up. Ninety-two percent (n=11) of respondents feel that implementation of a SCP could be utilised as a tool for follow up by GPs and ANPs. Most respondents (69.2%, n=9) believe that in-hospital surveillance clinics run by ANPs would be an appropriate method of follow-up using the SCP as an adjunct.
Part 2
Twenty-eight patients in follow-up were provided with a SCP at the MO clinic and subsequently were sent a follow-up postal questionnaire. We received 16 (57%) responses.
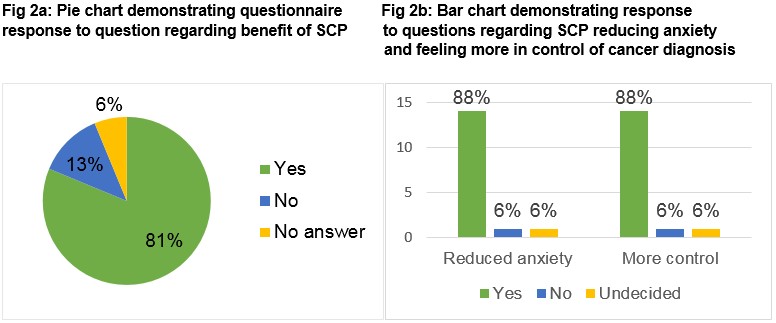
Most patients, 81% (n=13) felt that the SCP was beneficial, 13% (n=2) disagreed and 6% (n=1) did not answer. When asked if the SCP reduced worry and/or anxiety regarding their history of bowel cancer, 81% (n=13) answered “Yes”, 13% (n=2) answered “No” and 6% (n=1) did not answer (Fig 2a). Thirdly, we asked if the SCP helped them feel more in control of their follow-up and 88% (n=14) agreed that it did, 6% (n=1) disagreed and 6% (n=1) did not reply (Fig 2b).
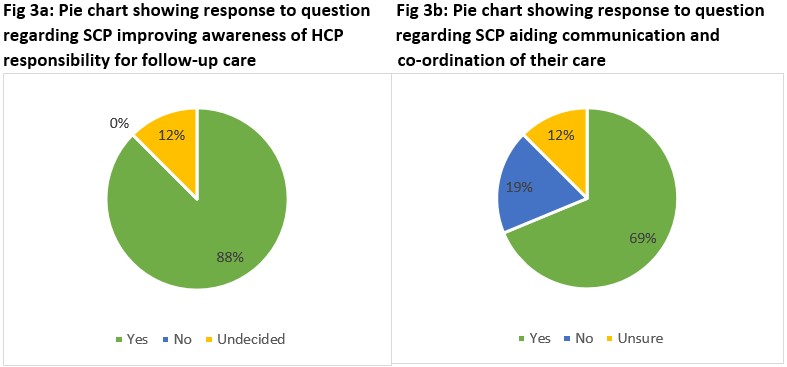
When asked if the SCP improved awareness of the HCPs responsible for follow-up, 88% (n=14) believed that it did and 12% (n=2) were undecided (Fig 3a). We asked if patients felt it aided communication and coordination of their care between the hospital services and their GP and 69% (n=11) answered “Yes”, 19% (n=3) answered “No” and 12% (n=2) were unsure (Fig 3b).
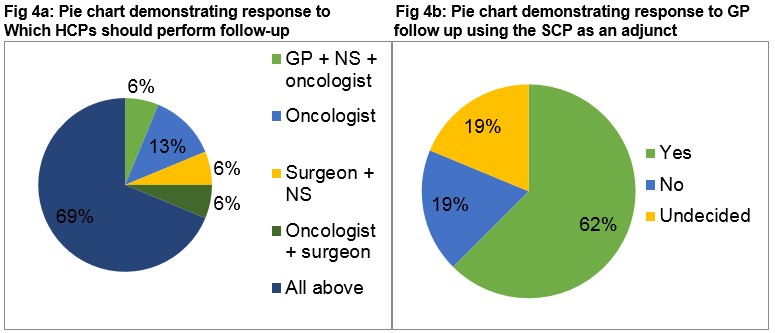
Sixty-nine percent (n=11) of patients would like to be followed by their oncologist, surgeon, nurse specialist and GP, 13% (n=2) by their oncologist alone and 1 patient each would like to be followed by an oncologist, surgeon and nurse specialist, an oncologist and a surgeon or a surgeon and nurse specialist respectively (Fig 4a). Lastly, we asked if GP follow-up in conjunction with the SCP, and access to hospital services if required, would be acceptable. The majority, 62% (n=10) answered “Yes”, 19% (n=3) disagreed and 19% (n=3) were undecided (Fig 4b)
Discussion
Cancer survivorship care has been recognised as a priority by the NCCP and the recently published NCS set out several targets aimed at enhancing survivorship care in Ireland. This is the first study to examine current patterns of surveillance in CRC and the potential role of the SCP. Our results demonstrate that current surveillance practices are heterogeneous. Most felt that surveillance in the MO clinic is suboptimal and that SCPs may be helpful in streamlining surveillance and if ANP follow-up clinics are established. This data advocates for the homogenization of guidelines for follow-up of patients with CRC.
As the number of survivors rise, demand for cancer services are growing. Health service planning must take account of the need to incorporate quality, efficient and structured survivorship care for our patients. Non-hospital-based follow-up should be explored which in turn may facilitate redirection of hospital resources. However, inherent challenges do exist. Comprehensive knowledge of late toxicities and survivorship issues (e.g. fatigue, altered bowel function, stoma care, neuropathy, genetic risk, psychosocial issues and increased risk of chronic disease) is required.14 There is also evidence that lifestyle interventions are important. Physical activity and reduced intake of dietary simple sugars and total carbohydrates in the diet (Delete) have been associated with a reduced risk of disease recurrence.15,16 Furthermore, it has been prospectively demonstrated that higher Vitamin D levels following surgery for stage I-III CRC are associated with improved survival.17 Delivering survivorship care which addresses the above issues will require an expansion in healthcare resources in this area.
It is currently unclear who is best placed to provide surveillance and survivorship care. An Australian randomised trial addressed generalist versus specialist care in CRC survivors and 203 patients CRC were assigned to follow-up by their GP or surgeon. There was no difference between groups in time to detection or survival, QoL or patient satisfaction.18
When survivorship care is undertaken by a GP, patients may benefit from more rounded preventive care and care for comorbid conditions than patients who are seen by oncologists alone.19 However, they may be less focused on long-term complications of treatment and surveillance recommendations. Two studies have suggested that there is potential for primary care to contribute more to ongoing care of patients both with breast cancer and CRC.20,21 However, in a recent survey of Irish GPs most felt they did not have enough information regarding long-term issues after cancer treatment.22
While the evidence base for SCPs remains limited,23,24 leading oncology organisations continue to support their use. In addition, there is consensus that evidence-based guidelines for survivorship care are required.24,25 Overall in our study patients reacted favorably to incorporation of the SCP into their follow-up. Most patients felt they should be followed by several HCPs although a small majority were agreeable to be followed by their GP with the use of the SCP. Patient education could improve understanding of the recommended follow-up and the roles of differing HCPs. This may in turn empower patients to take a more active role in their care. Patients are often reluctant to be discharged from MO follow-up and a cultural shift may be required in this regard. It is imperative that patients and GPs have trust in their ability to access specialist care when required. In an era of heightened public awareness of the ‘cancer journey’ and exposure to personal stories on social media, survivorship will have an increasingly prominent place in the dialogue of patients recovering from a cancer diagnosis. Therefore, this is an opportune time to educate survivors, GPs and hospital specialists about the needs of this population and the NCS seeks to address these issues.
The time and resource intensive nature of completing a SCP, and which HCP is best placed to do so, may represent barriers to implementation. The planned national electronic medical record may help overcome this. As a first step, a ‘shared-care model’ could be considered whereby patients and their GPs are provided with a SCP at on completion of treatment. Survivorship workshops could be undertaken to provide GPs with education on CRC follow-up and survivorship issues, thereby facilitating them to play a greater role in the follow-up of these patients.
In conclusion, CRC follow-up and survivorship care in Ireland is heterogenous and patients often feel lost in transition following the acute phase of their care. It is recognised that a busy MO clinic is a suboptimal environment for appropriately addressing patient’s survivorship needs. Our study identified that both patients and MOs feel the SCP may be beneficial as an instrument for supporting co-ordinated care between hospital specialists and GPs and over time may facilitate care to occur in a more suitable setting potentially involving ANPs and GPs. Future efforts by our team will seek to provide a national consensus on follow up guidelines and pilot a ‘shared-care model’ of survivorship.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Corresponding Author
Megan Greally,
Gastrointestinal Oncology,
Department of Medicine,
Memorial Sloan Kettering Cancer Center,
1275 York Avenue,
New York.
Phone: +1 917-705-3949
Email: [email protected]
References
1. National Cancer Registry (2013) Colorectal cancer incidence, mortality, treatment and survival in Ireland 1994-2010. NCR, Cork, Ireland
2. Tomlinson JS, Jarnagin WR, DeMatteo RP, Fong Y, Komprat P, Gonen M, Kemeny N, Brennan MF, Blumgart LH, D’Angelica M. Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol 2007; 25(29):4575-4580
3. Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, Rougier P, Bechstein WO, Primrose JN, Walpole ET, Finch-Jones M, Jaeck D, Mirza D, Parks RW, Collette L, Praet M, Bethe U, Van Cutsem E, Scheithauer W, Gruenberger T. EORTC Gastro-Intestinal Tract Cancer Group; Cancer Research UK; Arbeitsgruppe Lebermetastasen und–tumoren in der Chirurgischen Arbeitsgemeinschaft Onkologie (ALM-CAO); Australasian Gastro-Intestinal Trials Group (AGITG); Fédération Francophone de Cancérologie Digestive (FFCD). Perioperative FOLFOX4 chemotherapy and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC 40983): long-term results of a randomised, controlled, phase 3 trial. Lancet Oncol 2013;14(12):1208-1215
4. Meyerhardt JA, Mangu PB, Flynn PJ, Korde L, Loprinzi CL, Minsky BD, Petrelli NJ, Ryan K, Schrag DH, Wong SL, Benson AB 3rd. American Society of Clinical Oncology. Follow-up care, surveillance protocol, and secondary prevention measures for survivors of colorectal cancer: American Society of Clinical Oncology clinical practice guideline endorsement. J Clin Oncol. 2013;31(35):4465-4470
5. National Cancer Registry (2016) Cancer in Ireland 1994-2014: Annual Report of the National Cancer Registry. NCR, Cork, Ireland
6. OECD (2013), Cancer Care: Assuring Quality to Improve Survival, OECD Health Policy Studies, OECD Publishing. http://dx.doi.org/10.1787/9789264181052-en
7. Harrison SE, Watson EK, Ward AM, Khan NF, Turner D, Adams E, Forman D, Roche MF, Rose PW. Primary health and supportive care needs of long-term cancer survivors: a questionnaire survey. J Clin Oncol 2011; 29:2091-2098
8. Zucca Ac, Boyes AW, Linden W, Girgis A. All’s well that ends well? Quality of life and physical symptom clusters in long-term cancer survivors across cancer types. J Pain Symptom Manage 2012; 43:720-731
9. McCabe MS, Bhatia S, Oeffinger KC, Reaman GH, Tyne C, Wollins DS, Hudson MM. American Society of Clinical Oncology statement: achieving high-quality cancer survivorship care. J Clin Oncol 2013; 31:631-640
10. Ligibel JA, Denlinger CS. New NCCN guidelines for survivorship care. J Natl Compr Canc Netw 2013; 11:640-644
11. Hewitt M, Greenfield S, Stovall E (Eds). From Cancer Patient to Cancer Survivor: Lost in Transition. Committee on Cancer Survivorship: Improving Care and Quality of Life, Institute of Medicine and National Research Council. Accessed May 13, 2017.
12. Forsythe LP, Parry C, Alfano CM, Kent EE, Leach CR, Haggstrom DA, Ganz PA, Aziz N, Rowland JH. Use of Survivorship Care Plans in the United States: Associations with Survivorship Care. J Natl Cancer Institute 2013; 105(20):1579-1587
13. The National Cancer Strategy 2017-2026. Available from: http://health.gov.ie/blog/publications/national-cancer-strategy-2017-2026/
14. Cupit-Link MC, Kirkland JL, Ness KK, Armstrong GT, Tchkonia T, LeBrasseur NK, Armenian SH, Ruddy KJ, Hashmi SK. Biology or premature ageing in survivors of cancer. ESMO Open 2017;2:e000250. doi:10.1136/esmoopen-2017-000250
15. Meyerhardt JA, Heseltine D, Niedzwiecki D, Hollis D, Saltz LB, Mayer RJ, Thomas J, Nelson H, Whittom R, Hantel A, Schilsky RL, Fuchs CS. Impact of physical activity on cancer recurrence and survival in patients with stage III colon cancer: findings from CALGB 89803. J Clin Oncol. 2006; 24(22):3535-41
16. Meyerhardt JA, Sato K, Niedzwiecki D, Hollis D, Saltz LB, Mayer RJ, Thomas J, Nelson H, Whittom R, Hantel A, Schilsky RL, Fuchs CS. Dietary glycemic load and cancer recurrence and survival in patients with stage III colon cancer: findings from CALGB 89803. J Natl Cancer Inst. 2012; 104(22):1702-11
17. Zgaga L, Theodoratou E, Farrington SM, Din FV, Ooi LY, Glodzik D, Johnston S, Tenesa A, Campbell H, Dunlop MG. Plasma vitamin D concentration influences survival outcome after a diagnosis of colorectal cancer. J Clin Oncol. 2014;32(23):2430-9.
18. Wattchow DA, Weller DP, Esterman A, Pilotto LS, McGorm K, Hammett Z, Platell C, Silagy C. General practice vs surgical-based follow-up for patients with colon cancer: randomised controlled trial. Br J Cancer. 2006; 94(8):1116
19. Khan NF, Mant D, Rose PW. Quality of care for chronic diseases in a British cohort of long-term cancer survivors. Ann Fam Med 2010; 8(5):418–424.
20. Naidoo J, Hayes E, Teo MY, Horgan A, Calvert P, O’Connor M. An Irish breast cancer survivorship study: are we meeting our patient’s needs? Ir Med J 2013;106(9):262, 264-6.
21. Browne S, Dowie A, Mitchell L, Ziebland S, Campbell N, Macleod U. Patients’ needs following colorectal cancer diagnosis: where does primary care fit in? Br J Gen Pract 2011; 61(592): e692-e699
22. O’Shea M, Collins C. Cancer Survivorship in General Practice – Barriers Encountered by General Practitioners in Ireland. Universal Journal of Public Health 2018; 6(2):73-78. doi: 10.13189/ujph.2018.060206.
23. Jacobsen PB, DeRosa AP, Henderson TO, Mayer DK, Moskowitz CS, Paskett ED, Rowland JH. Systematic Review of the Impact of Cancer Survivorship Care Plans on Health Outcomes and Health Care Delivery. J Clin Oncol 2018 [epub ahead of print]. doi: 10.1200/JCO.2018.77.7482.
24. Mayer DK, Birken SA, Check DK, Chen RC. Summing it up: an integrative review of studies of cancer survivorship care plans (2006-2013). Cancer 2015; 121(7):978-96.
25. Brennan ME, Gormally JF, Butow P, Boyle FM, Spillane AJ. Survivorship care plans in cancer: a systematic review of care plan outcomes. Br J Cancer 2014; 111: 1899-1908.
P870
