An audit of empiric antibiotic choice in the inpatient management of community-acquired pneumonia
F Delaney, A Jackson
Mercy University Hospital, Grenville Place, Cork City, County Cork, Ireland
Abstract
Adherence to antimicrobial guidelines for empiric antibiotic prescribing in community-acquired pneumonia (CAP) has been reported to be worryingly low. We conducted a review of empiric antibiotic prescribing for sixty consecutive adult patients admitted to the Mercy University Hospital with a diagnosis of CAP. When analysed against local antimicrobial guidelines, guideline concordant empiric antibiotics were given in only 48% of cases, lower than the average rate in comparable studies. Concordance was 100% in cases where the CURB-65 pneumonia severity assessment score, on which the guidelines are based, was documented in the medical notes. The use of excessively broad spectrum and inappropriate antibiotics is a notable problem. This study supports the theory that lack of knowledge regarding pneumonia severity assessment tools and unfamiliarity with therapeutic guidelines are key barriers to guideline adherence, which remains a significant problem despite increased focus on antimicrobial stewardship programs in Ireland.
Introduction
In hospitalised patients, community-acquired pneumonia (CAP) can be defined as symptoms and signs consistent with acute lower respiratory tract infection, associated with new radiographic shadowing for which there is no other explanation, where this illness is the primary reason for hospital admission1. It is an illness which combines a high incidence with significant morbidity and mortality, and is therefore associated with a considerable healthcare and economic burden. The annual incidence rate in adults is 1.2-14/1000 varying with age, with a hospital admission rate of roughly 40%2. Mortality in those hospitalised ranges from 10-40% depending on severity and need for ICU admission3, 4.
The selection of an initial antimicrobial regimen for empiric therapy is based on consideration of the most likely underlying pathogens and knowledge of local susceptibility and epidemiologic patterns5. Guidelines should therefore be as local and specific to a particular country/region as possible. Over the last 20 years, guidelines for the management of CAP and other infectious illnesses have been developed by many regional committees aiming to accomplish a more uniform approach toward empiric antibiotic treatment.
Broad-spectrum guideline-concordant empiric therapy maximises the likelihood of starting the patient on the appropriate antibiotic treatment in a timely manner, and has comparable clinical efficacy to pathogen-directed approach6. Inappropriate initial therapy in hospitalised CAP patients is associated with longer hospital stays, increased financial costs and higher mortality rates7, 8. Furthermore, inappropriate antibiotic choice accelerates the emergence of resistance5, and guideline concordance can be more important than the actual antibiotic used9. However, adherence to guidelines on the empiric antibiotic treatment of CAP has often been found to be worryingly low when studied10-13, with the use of antibiotics excessively broad in spectrum especially concerning. The British Thoracic Society CAP audit in 200912 reported an adherence rate of 50-70% depending on CAP severity, with intravenous and combination therapy overused in patients who did not have a high severity of illness.
Mercy University Hospital is a general acute care hospital in Cork city centre. It provides approximately 350 beds and offers a wide range of specialities with in-patient, day patient, out-patient and emergency services. The antimicrobial guidelines used in the Mercy University Hospital (MUH) classify the empiric antibiotic regimen for CAP based on severity as determined by the CURB-65 score. This is one of a number of prognostic scoring systems which have been developed to aid in the management of CAP and guide the appropriate setting and level of treatment14. In Ireland no specific review of guideline concordance in the administration of empiric antibiotics in patients hospitalised with CAP has been performed. An audit15 in 2006 into CAP inpatient management in an Irish setting reported that the majority of patients were not stratified based on established criteria or scoring systems, with a significant number given an excessively broad-spectrum or inappropriate empiric antibiotic regimen. The healthcare and economic burden of inappropriate empiric antibiotic prescribing, in combination with the poor rates of guideline adherence reported in other countries and the flourishing issue of antibiotic resistance, warrant review of empiric antibiotic administration for CAP in an Irish hospital setting.
Methods
Adult patients admitted to MUH in the two month period between the 19th of October and the 19th of December 2015 with a principal diagnosis of CAP, who had a clearly suggestive infiltrate on initial chest radiograph, were eligible for inclusion. Exclusion criteria were as follows: diagnosis of cystic fibrosis, bronchiectasis, tuberculosis or HIV, known lung carcinoma, or chemotherapy in the past year.The patient cohort was indentified using a multi-step process. An electronic search of the Integrated Patient Management System (iPIMS) database in the MUH identified all patients admitted under a medical speciality each day over the two months. The radiology database Impax was then used to determine which of the admitted patients underwent a chest radiograph on admission. The consultant validated reports of these radiographs were reviewed and those with an infiltrate clearly suggestive of infection noted. These patients then made up the initial study cohort and their medical notes were examined.
A true community-acquired pneumonia was confirmed by excluding those who met the criteria for healthcare-associated pneumonia as defined in the guidelines. This left a final group of patients eligible for the audit. A case report form, developed based on review of the literature and expert consultant advice, was then completed for each using the medical notes, drug Kardex and radiology report.The data collected was used to determine if the empiric antibiotic regimen given to each subject was concordant with the local guidelines. The medical notes were re-referred to if necessary. The raw data collected was then entered manually into Microsoft Excel. Subjects were grouped based on CURB-65 score from 0 to 4. Descriptive statistics were used to represent the following: patient demographics, CURB-65 scores and documentation, imaging findings, empiric antibiotic regimen and guideline adherence.
Results
Demographics
There were 60 adult patients admitted to the MUH in the two month period with a diagnosis of CAP. The mean [range] age of the study subjects was 71.85 [27-101]. 32 (53%) were female.
Presentation and Prognostic Scoring
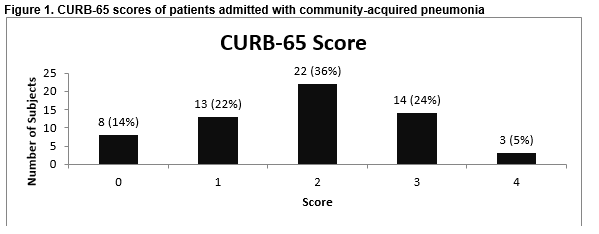
Forty-one (68%) presented with symptoms consistent with a lower respiratory tract infection, while 50 (83%) had raised inflammatory markers on initial blood testing. CURB-65 scores are shown in Figure 2. The CURB-65 score was documented in the medical notes in 7 of the 60 cases (12%).
Guideline Adherence
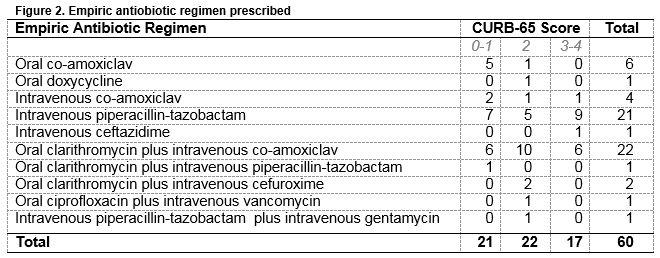
Empiric antibiotic regimen was concordant with local guidelines in 29 (48%) of the 60 cases. Concordance was highest in those with a CURB-65 score of 2 (59%) and lowest with a score of 3-4 (35%) with scores of 0-1 (43%) in between. Guideline adherence was 100% in those 12% of cases with the CURB-65 score documented in the medical notes. Of the 31 cases where empiric antibiotic choice was inappropriate, 23 were given piperacillin-tazobactam, either alone or in combination with another antimicrobial. Sixteen received intravenous antibiotics when oral were indicated (CURB-65 = 0-1) and 1 received oral when intravenous was indicated (CURB-65 = 2).
Discussion
CAP is certainly a common reason for hospital admission in Ireland and can present with a wide spectrum of illness. Initial accurate assessment of disease severity and prognosis is imperative in determining the appropriate site of care and guiding treatment. CAP prognostic scoring systems such as the CURB-65 score are well-validated in assisting with this process. Significantly however, as in previous studies15-17, the frequency of recording of these scores in clinical documentation is extremely low (12%), despite its association9 with improved guideline adherence for empiric antibiotic choice, emphasised here (100% concordance when documented).
Over one-third had a CURB-65 score of 0-1 which indicated that they may have been suitable for outpatient treatment in the absence of a significant co-morbidity. This may reflect excessive use of inpatient care for CAP which contributes to unnecessary interventions and further risks for patients as well as increased healthcare costs. Although the decision to admit patients with a CURB-65 of 0 and 1 may have been based on other factors not allowed for here, poor compliance with national guidelines when considering hospital admission for CAP is a recurring issue17, 18.
Our 48% guideline adherence rate is lower than similar studies9,12. Piperacillin-tazobactam was used in empiric therapy for CAP in 38% of cases, despite its absence from the local CAP antimicrobial guidelines regardless of the setting or patient. This suggests a significant lack of knowledge surrounding these guidelines, and reflects the trend towards the use of excessively broad-spectrum antibiotics (particularly piperacillin-tazobactam), in many healthcare settings. A likely contributor to this is the increased focus on achieving targets for prompt antibiotic administration in patients meeting sepsis criteria, with piperacillin-tazobactam a common default antibiotic when the source may be unclear. In addition, 76% of patients with a CURB-65 score of 0-1 received intravenous antibiotics.
This study supports the theory that lack of knowledge regarding pneumonia severity assessment tools, inadequate education on antibiotic therapy and unfamiliarity with therapeutic guidelines are key barriers to guideline adherence19. Educational interventions which are multifaceted and robust, in combination with antimicrobial stewardship programs, have been proposed as the best way to improve guideline adherence for empiric antibiotics20. Undergraduate education on antibiotic prescribing needs to be more directly relevant to clinical practice and hospital guidelines need to be readily-accessible and in a user-friendly format21, 22. Targeted educational interventions including audit and feedback have shown to improve both pneumonia severity tool documentation and adherence to CAP guidelines17.
Inappropriate empiric antibiotic prescribing in CAP remains a significant problem in an Irish setting, in spite of increased focus on antimicrobial stewardship. Controlling cost within the Irish healthcare system is an ever growing concern and inappropriate empiric antibiotic prescribing in CAP increases the length of hospital stay and financial costs. This, in combination with the poor rates of guideline adherence reported in this and other studies and the flourishing issue of antibiotic resistance, warrant ongoing review of empiric antibiotic administration in an Irish hospital setting.
Correspondence:
Dr. Francis Delaney, Mercy University Hospital, Grenville Place, Cork City, County Cork
Telephone: 353879178959
E-mail: [email protected]
Conflict of interest:
The authors confirm that there is no conflict of interest to be declared with regards to the above work.
References
1. Lim WS, Baudouin SV, George RC, Hill AT, Jamieson C, Le Jeune I, Macfarlane JT, Read RC, Roberts HJ, Levy ML, Wani M, Woodhead MA . BTS Guidelines for the management of community-acquired pneumonia in adults: update 2009. Thorax 2009;64:iii1-iii5
2. Torres A, Peetermans WE, Viegi G, Blasi F. Risk factors for community-acquired pneumonia in adults in Europe: a literature review. Thorax. 2013; 68(11):1057–65.
3. Nair GB, Niederman MS. Community-acquired pneumonia: an unfinished battle. Med Clin N Am. 2011;95(6):1143–61
4. Gattarello S, Borgatta B, Solé-Violán J, Vallés J, Vidaur L, Zaragoza R, Torres A, Rello J. Decrease in mortality in severe community-acquired pneumococcal pneumonia: impact of improving antibiotic strategies (2000-2013). Chest 2014 Jul;146(1):22-31
5. Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF, File TM Jr, Musher DM, Niederman MS, Torres A, Whitney CG, Infectious Diseases Society of America, American Thoracic Society. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007 Mar 1; 44 Suppl 2:S27-72
6. van der Eerden MM, Vlaspolder F, de Graaff CS, Groot T, Bronsveld W, Jansen HM, Boersma WG. Comparison between pathogen directed antibiotic treatment and empirical broad spectrum antibiotic treatment in patients with community acquired pneumonia: a prospective randomized study. Thorax. 2005; 60(8):672-8
7. Oster G, Berger A, Edelsberg J, Weber DJ. Initial treatment failure in non-ICU community-acquired pneumonia: risk factors and association with length of stay, total hospital charges, and mortality. J Med Econ. 2013;16(6):809–819
8. McCabe C, Kirchner C, Zhang H, Daley J, Fisman DN. Guideline-concordant therapy and reduced mortality and length of stay in adults with community-acquired pneumonia: playing by the rules. Arch Intern Med 2009 Sep 14;169(16):1525-31
9. Triantafyllidis C, Kapordelis V, Papaetis GS, Orphanidou D, Apostolidou M, Nikolopoulos I, Pefanis A. Guidelines adherence for patients with community acquired pneumonia in a Greek hospital. Eur Rev Med Pharmacol Sci. 2012 Jan; 16(1):1-9
10. Arnold FW, LaJoie AS, Brock GN, Peyrani P, Rello J, Menendez R, Lopardo G, Torres A, Rossi P, Ramirez JA. Improving outcomes in elderly patients with community-acquired pneumonia by adhering to national guidelines: Community-Acquired Pneumonia Organization International cohort study results. Arch Intern Med. 2009;169:1515–24
11. Dambrava PG, Torres A, Vallès X, Mensa J, Marcos MA, Penarroja G, Camps M, Estruch R, Sanchez M, Menendez R, Niedermann MS. Adherence to guidelines’ empirical antibiotic recommendations and community-acquired pneumonia outcome. Eur Respir J. 2008;32:892–901
12. Lim WS, Woodhead M. British Thoracic Society adult community acquired pneumonia audit 2009/10.Thorax. 2011;66:548–9
13. Switzer GE, Halm EA, Chang CC, Mittman BS, Walsh MB, Fine MJ. Physician awareness and self-reported use of local and national guidelines for community-acquired pneumonia. J Gen Intern Med.2003;18:816–23
14. Lim WS, van der Eerden MM, Laing R. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax 2003;58:377-82
15. Foley SC, Kelly EM, O'Neill SJ. Audit of the management of patients admitted with community acquired pneumonia. Ir Med J. 2006 May; 99(5):138-40
16. Brett J, Lam V, Bayasari M. Pneumonia severity scores and prescribing antibiotics for community-acquired pneumonia at an Australian hospital. J Pharm Pract Res. 2013;43(2):97–100
17. McIntosh KA, Maxwell DJ, Pulver LK, Horn F, Robertson MB, Kaye KI, Peterson GM, Dollman WB, Wai A, Tett SE. A quality improvement initiative to improve adherence to national guidelines for empiric management of community-acquired pneumonia in emergency departments. Int J Qual Health Care. 2011 Apr;23(2):142-50
18. Nadarajan P, Wilson L, Mohammed B, Connor M, Lane SJ. Compliance in the measurement of CURB-65 in patients with community-acquired pneumonia and potential implications for early discharge. Ir Med J. 2008 May; 101(5): 144-6
19. Barlow G, Nathwani D, Myers E, Sullivan F, Stevens N, Duffy R, Davey P. Identifying barriers to the rapid administration of appropriate antibiotics in community-acquired pneumonia. J Antimicrob Chemother. 2008 Feb; 61(2):442-51
20. Adler NR, Weber HM, Gunadasa I, Hughes AJ, Friedman ND. Adherence to Therapeutic Guidelines for Patients with Community-Acquired Pneumonia in Australian Hospitals. Clin Med Insights Circ Respir Pulm Med. 2014 Sep 14;8:17-2
21. De Souza V, MacFarlane A, Murphy AW, Hanahoe B, Barber A, Cormican M. A qualitative study of factors influencing antimicrobial prescribing by non-consultant hospital doctors. J Antimicrob Chemother. 2006 Oct; 58(4):840-3
22. Mol PG, Rutten WJ, Gans RO, Degener JE, Haaijer-Ruskamp FM. Adherence barriers to antimicrobial treatment guidelines in teaching hospital, the Netherlands. Emerg Infect Dis. 2004 Mar; 10(3):522-5
(P545)