Attitudes and Knowledge of Healthcare Professionals Regarding Organ Donation. A Survey of the Saolta University Health Care Group.
E Umana1, O Grant2, E Curran2, 3, P May3, A Mohamed2, J O’Donnell1
1. Department of Emergency Medicine, University Hospital Galway, Galway
2. Department of Anaesthesia, University Hospital Galway, Galway
3. Intensive Care Department, University Hospital Galway, Galway
Abstract
Organ donation saves lives and healthcare professionals (HCPs) play a vital role in that process. Therefore, the purpose of this study was to assess the attitudes and level of knowledge of HCPs regarding organ donation. An online anonymous self-administered questionnaire containing 40 questions on organ donation using google forms was created. The survey was distributed to HCPs working in the Saolta University Health Care Group. A hundred and thirty-nine responses were received giving a response rate of 11.8%. HCPs willingness to donate their organs was at 93% compared to 97% willing to receive a transplant. More HCPs understood or had knowledge of the term donation after brain death (64%) than donation after circulatory death (49%). HCPs working in intensive care knew more about the management of brain dead donors than other specialties (p<0.0001). Over 60% of HCPs when asked either disagreed or strongly disagreed with the adequacy of training in organ donation and transplant. Overall, HCPs surveyed had positive attitudes towards organ donation but there was a lack of knowledge particularly among non-intensive care professionals. This study highlights the need to increase awareness along with implementation of educational programmes among HCPs regarding organ donation and transplant.
Introduction
In 1964 the first organ (kidney) was transplanted in Ireland1. Since then organ transplantation has grown enormously and includes pancreas, liver, lung and heart transplants. In 2016, the Organ Donation and Transplant Ireland (ODTI) reported a total of 280 people received a life-saving organ transplant and currently, 55% of people with end-stage renal failure are treated with a transplant in Ireland1. Organ transplantation has become the most effective treatment for those patients with end-stage organ failure. Despite such advancements, there is a chronic imbalance between the supply and demand for organs both nationally and internationally1, 2.This organ shortage results in many potential recipients being on a waiting list for a prolonged period with resultant increase in mortality1, 3. According to 2015 statistics, Ireland was ranked 18th in terms of deceased organ donors per million population compared to other European countries with Croatia and Spain coming in first and second respectively4. Thus increasing donation rates is important in Ireland.
Increasing donation rates involves multiple factors which include increasing awareness and educating both the public and health care professionals (HCPs), development of guidelines, creating agencies and considering legislative changes. Donation rates were increased by Croatia and Spain by also embedding specialist key organ donation personnel within emergency, intensive care and operating theatre departments. HCPs play an important role in the organ donation process, including identification and referral of potential donors. They also are involved in management of potential donors, engaging donor families and acquiring consent. The attitudes and knowledge of HPCs towards organ donation is important as some studies have suggested that HCPs can positively influence families of potential donors3, 5. Currently, there are several studies assessing the attitudes and knowledge of HCPs from various regions of the world but none so far assessing HCPs in Ireland5-9. Therefore, the purpose of this study was to assess the attitudes and level of knowledge of HCPs regarding organ donation in the Saolta University Health Care Group comprising 6 hospitals in the west of Ireland.
Method
An online anonymous self-administered questionnaire using google forms was created based on the prior works of Hu et al and Bedi et al in surveying attitudes and knowledge of HCPs and medical students towards organ donation 9, 10. This study was conducted over a 4 week period in October 2017. The survey was sent to all hospitals within the Saolta University Health Care Group (University Hospital Galway, Sligo University Hospital, Mayo University Hospital, Roscommon Hospital, Letterkenny University Hospital and Portiuncula University Hospital). The participants of this study consisted of doctors working in acute specialties (emergency medicine, medicine, surgery, intensive care medicine and anaesthesia), intensive care nurses and nurses working in the emergency department (ED) of University Hospital Galway. The survey consisted of 40 questions divided into 3 categories: 7 questions on demographic details, 10 questions on attitudes of HCPs towards organ donation and 23 questions on knowledge of HCPs regarding organ donation. The survey was distributed via email and was sent on 2 subsequent occasions to encourage better response rates. Frequencies were used to describe demographics, attitudes, knowledge and associations were examined using chi-squared test. Results were considered significant at p<0.05.
Results
There were 139 responses received from 1176 HCPs emailed the survey, thus giving a response rate of 11.8%.
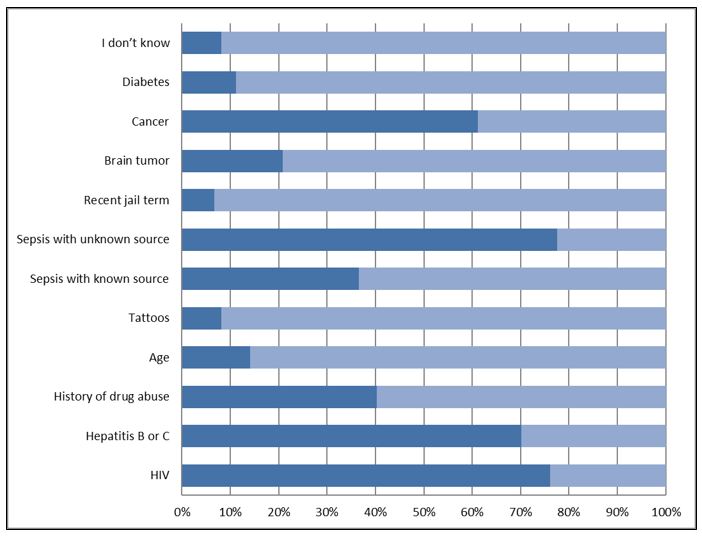
Table 1: Demographics characteristics
Demographics
Table 1 outlines the demographic characteristics of the participants in the study. There was a female preponderance of 63%. Over 50% of HCPs were above the age of 30. Eighty-six per cent were doctors (120), while only 14% (19) were nurses. Senior house officers and staff nurses made up the highest number among doctors and nurses respectively. Regarding years of experience, 55% of HCPs had less than 5 years in practice. The majority (73%) of respondents were from University Hospital Galway. Approximately 39% of HCPs did not document their religion.
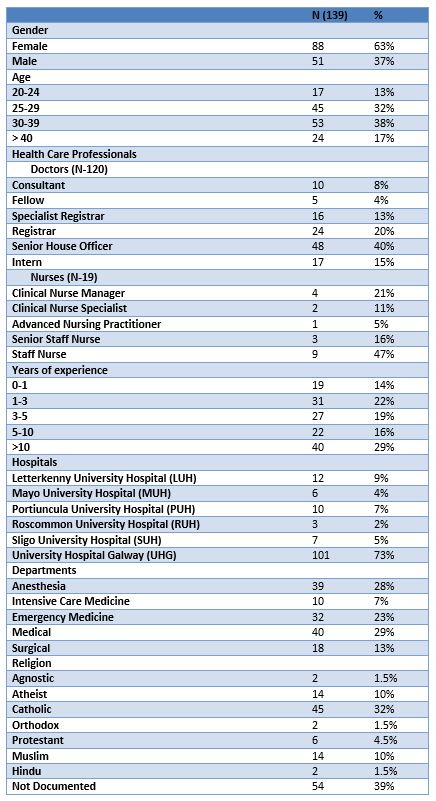
Figure 1: Which of the following can be donated after death in Ireland?
Attitudes
Eighty-six percent (119) of HCPs had considered donating their organs. Amongst HCPs who considered donation, 72 had discussed with their next of kin, 67 had ticked organ donor on their driver’s license, 59 had a donor card and 32 had done all the above. Over 93% of HCPs wish to donate their organs after death. HCPs not willing to donate their organs gave reasons such as: “religious belief”, “not decided yet”, “health condition” and “against taking out my organs”. If transplantation was necessary, 97% of HCPs were willing to receive organ donation from both living and deceased donors. Only 18% of HCPs had someone close to them who was involved in organ donation and transplant. The majority (81%) of HCPs were in support of changing the law, so that everyone is an organ donor unless they opt-out or their families decline. Half of the HCPs reported being involved in care of patients where organ donation was a possibility but did not occur. When asked for a reason as to why organ donation did not occur, most HCPs reported that it was not a practical option or it was not suggested.
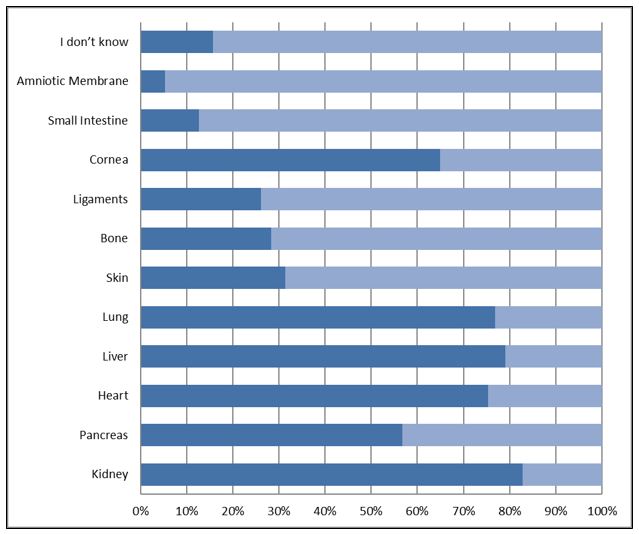
Figure 2: Do you think any of the following are contraindications to organ donation?
Knowledge
Over 75% of HCPs were conversant with the terms solid, tissue and living donation. Most (83%) HCPs were aware that majority of people who need a transplant don’t receive one, with 3% stating otherwise and 14% not sure. The kidney, liver, lungs and heart were identified by HCPs as the most commonly donated organs after death in Ireland (Figure 1). The kidney was correctly identified by most HCPs as the most common organ for living donation. The most common contraindications to organ donation selected by HCPs were infection with HIV, Hepatitis B or C, sepsis of unknown source and cancer (Figure 2). In terms of awareness of laws governing organ donation in Ireland, 10% were aware, 45% were not and 45% were unsure. Forty two percent of HCPs were aware that according to Irish law, a person who is brain dead is legally dead. More (58%) HCPs knew about guidelines for brainstem death (BSD) diagnosis than guidelines for organ donation and transplant (40%). The term BSD was understood by most (91%) HCPs who also felt that a consultant or doctor fully registered for 5 years could carry out BSD testing.
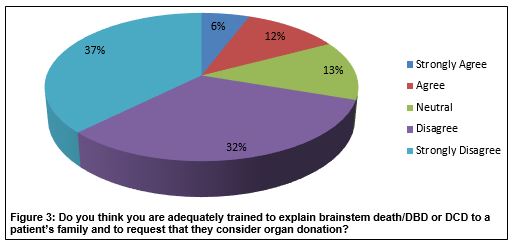
More HCPs understood or had knowledge of the term donation after brain death (64%) than donation after circulatory death (49%). Approximately 28% of HCPs were knowledgeable of triple therapy and how to manage brain dead donors. HCPS working in intensive care knew more about the management of brain-dead donors than other specialties (p<0.0001). “After diagnosis of brainstem death” (65%) was considered the best time to approach a family about organ donation by most HCPs compared to 24 hours after ED presentation (6%), 12 hours after ED presentation (3%), (4%) after coroner’s permission, while the remainder (22%) were unsure. The Majority of the HCPs when asked either disagreed or strongly disagreed with the adequacy of training in organ donation and transplant (Figure 3).
Discussion
There have been surveys of public awareness and attitudes towards organ donation in Ireland but none so far have targeted HCPs. Our study is the first to focus on attitudes and knowledge of HCPs in the Irish health service. High rates of responses were notably female (63%) among HCPs. This has been observed in other studies6, 7, 9 and has been attributed to the altruism of women. Women may be more inclined to discuss the sensitive issues surrounding mortality and organ donation. In terms of religion among HCPs, there was significant diversity noted. Religion has always been thought of as a barrier to organ donation, but such notions have been dispelled particularly in recent studies by Bener et al and Alsaied et al3, 11. In their study, religion had no impact on attitudes towards organ donation among HCPs surveyed3, 11.
The majority (86%) of HCPs would consider donating their organs and most have discussed organ donation with their next of kin, while only a third had either ticked organ donor on their driver’s license or had a donor card. Compared to the Irish public survey on organ donation carried out in March 2015, one third of the general population carried an organ donor card and half had discussed organ donation with family12. There was a 10% increase among the public for those carrying donor cards and those who discussed organ donation with family compared to previous surveys conducted in 2003 and 2009 respectively 12. This shows that both the public and HCPs are aware of organ donation and are willing to participate in the process by becoming organ donors.
There was a discrepancy in willingness to donate (93%) compared to those willing to receive (97%) organ transplants among HCPs in our survey. A 7% difference was also observed in the ODTI’s public survey in Ireland12, in favour of more people willing to receive organs (95%).There was no clear explanation as to why this discrepancy exists but the aim would be to match expectations of donation and transplant through education. Currently, organ donation in Ireland is based on a voluntary donation system (opt-in) as there is no legislation governing consent. In an attempt to increase donation rates in Ireland, there has been a push to introduce a soft opt-out system which was supported by majority (81%) of HCPs who are also aware of the organ shortage in the country. The impact of the opt-out system or presumed consent on donation rates is presented by some studies as a positive one when compared to countries with an opt-in system 13.
Less than half of HCPs were knowledgeable about laws or guidelines regarding organ donation and BSD. Even less knew about diagnosis or the management of patients who are BSD. These findings imply that there is a lack of knowledge among HCPs, particularly non-intensivists, and highlights the need for further education to increase awareness and knowledge. This also reflects the response from majority of HCPs in this study about being inadequately trained in matters of organ donation. Research has shown educating not only HCPs but also medical and nursing students can positively influence attitude and knowledge leading to willingness to donate their own organs as well as equip HCPs when having difficult conversations with family members and obtaining consent14-16.
Our study had several limitations. There was a low response rate which could mean that only participants interested in organ donation were likely to participate. There was also significant disparity in responses among hospitals in the Saolta group with University Hospital Galway having the most responses compared to the others. Due to this difference we were unable to compare attitudes and knowledge between hospitals in the Saolta group. Nurses were also under-represented in this study, with a response rate of only 7% out of 263 nurses surveyed.
The benefits of organ donation not only lie with the recipients but also hands the grieving family of the organ donor closure at their time of loss. Organ transplantation has been shown to improve quality of life and is a cost-effective form of management for patients with end organ failure17. In summary, HCPs surveyed had positive attitudes towards organ donation but there was lack of knowledge particularly among non-intensivists. The findings in this study highlight the need to increase awareness along with implementation of educational programmes among HCPs regarding organ donation and transplant.
Conflict of Interest
The authors declare no conflict of interest.
Corresponding Author
Dr Etimbuk Umana,
Department of Emergency Medicine,
University Hospital Galway,
Galway.
Email: [email protected]
References
1. Organ Donation and Transplant Ireland (ODTI): Annual Report. 2016. [Cited: 18 Feb. 2018]. Available from: https://www.hse.ie/eng/about/who/organdonation/publications/organ-donation-and-transplant-annual-report-2016.pdf.
2. Gómez M, Pérez B, Manyalich M. International Registry in Organ Donation and Transplantation—2013. Transplantation Proceedings. 2014;46(4):1044–8.
3. Bener A, El-Shoubaki H, Al-Maslamani Y. Do we need to maximize the knowledge and attitude level of physicians and nurses toward organ donation and transplant? Experimental and clinical transplantation. 2008;6(4):249-53.
4. European Kidney Patients Federation. European and EU countries organ donation and transplant. 2015. [Cited: 18 Feb. 2018]. Available from: http://www.ika.ie/pdf/ika_euro_and_eu_organ_donor_and_tx_stats-2015.pdf.
5. Cantwell M, Clifford C. English nursing and medical students’ attitudes towards organ donation. Journal of Advanced Nursing. 2000;32(4):961–8.
6. Bøgh L, Madsen M. Attitudes, knowledge, and proficiency in relation to organ donation: a questionnaire-based analysis in donor hospitals in northern Denmark. Transplantation Proceedings. 2005;37(8):3256-7.
7. Radunz S, Hertel S, Schmid KW, Heuer M, Stommel P, Frühauf NR, Saner FH, Paul A, Kaiser GM. Attitude of health care professionals to organ donation: two surveys among the staff of a German university hospital. Transplantation Proceedings. 2010;42(1):126-9.
8. Araujo C, Siqueira M. Brazilian Healthcare Professionals: A Study of Attitudes Toward Organ Donation. Transplantation Proceedings. 2016;48(10):3241-3244.
9. Hu D, Huang H. Knowledge, Attitudes, and Willingness Toward Organ Donation Among Health Professionals in China. Transplantation. 2015;99(7):1379-85.
10. Bedi KK, Hakeem AR, Dave R, Lewington A, Sanfey H, Ahmad N. Survey of the knowledge, perception, and attitude of medical students at the University of Leeds toward organ donation and transplantation. Transplantation Proceedings. 2015;47(2):247–60.
11. Alsaied O, Bener A, Al-Mosalamani Y, Nour B. Knowledge and attitudes of health care professionals toward organ donation and transplantation. Saudi Journal of Kidney Diseases and Transplantation. 2012;23(6):1304-10.
12. Organ Donation and Transplant Ireland (ODTI): Annual Report. 2015. [Cited: 20 Feb. 2018]. Available from: https://www.hse.ie/eng/about/who/organdonation/publications/odtiarjul15.pdf.
13. Abadie A, Gay S. The impact of presumed consent legislation on cadaveric organ donation: A cross-country study. Journal of Health Economics. 2006;25(4):599–620.
14. Schaeffner ES, Windisch W, Freidel K, Breitenfeldt K, Winkelmayer WC. Knowledge And Attitude Regarding Organ Donation Among Medical Students And Physicians. Transplantation. 2004;77(11):1714–8
15. Mcglade D, Pierscionek B. Can education alter attitudes, behaviour and knowledge about organ donation? A pretest–post-test study. BMJ Open. 2013;3(12).
16. Kosieradzki M, Jakubowska-Winecka A, Feliksiak M, Kawalec I, Zawilinska E, Danielewicz R, Czerwinski J, Malkowski P, Rowiński W. Attitude of Healthcare Professionals: A Major Limiting Factor in Organ Donation from Brain-Dead Donors. Journal of Transplantation. 2014;2014:1–6.
17. Whiting JF, Kiberd B, Kalo Z, Keown P, Roels L, Kjerulf M. Cost-Effectiveness of Organ Donation: Evaluating Investment into Donor Action and Other Donor Initiatives. American Journal of Transplantation. 2004;4(4):569–73.
P838
