Attitudes toward Palliative Care and End of Life Issues: A Prospective Survey in Patients with Metastatic Cancer
C Docherty1, L Lester1, S O’Reilly2
1University College Cork Graduate Entry Medicine CUH
2Cork University Hospital/Mercy University Hospital/South Infirmary Victoria University Hospital
Abstract
Palliative care (PC) positively impacts patient outcomes, decreases hospital admissions and improves quality of life. Despite evidence, PC resources are reported as under-utilised. Few studies have explored patient attitudes towards PC. This study evaluated patient attitudes towards PC. It was a prospective study conducted in oncology outpatient clinics. A 26-item questionnaire was distributed to those with metastatic cancer (N = 44). Sixty percent believed PC can make people ‘feel better’, 63.4% believed PC is offered when nothing more can be done. Most were unsure or disagreed that opioids are addictive. Eighty percent reported symptom control is more important than prolonging life. Sixty-one percent strongly agreed or agreed that ‘losing hope makes people die sooner’. Although PC was deemed beneficial, a significant relationship exists between familiarity with PC and thinking it’s offered when ‘nothing more can be done’. Lack of knowledge about opioids, preference for symptom control over life prolonging measures and the importance of hope were also emphasised.
Introduction
End of life care research demonstrates that early introduction to palliative care is beneficial for patients, their families and even their primary care physicians. A study done by Kwon et al (1) illustrates that late referrals to palliative care had a significantly greater number of hospital days in total and a greater number per month than those who had been referred early. Temel et al (2) reported a 25% improvement in quality of life and survival with earlier introduction of palliative care in patients with metastatic non-small cell lung cancer. Other studies have demonstrated lower rates of depression and longer median survival rates.
Although studies have established the many benefits for patients, palliative care and hospice resources are reported as being used less effectively than they could be and are perceived by physicians as underutilized3-5. Surveys of physician and population attitudes towards palliation have attempted to discern this further. A perceived barrier highlighted in several studies from the health care providers’ view point is patients’ and families’ attitude towards palliative care3-5. There is little research exploring patients’ perspectives towards palliative care. No study has investigated these viewpoints in Ireland.
This study evaluates patients’ attitudes towards palliative care and end of life care in metastatic cancer. This information may improve our understanding of patients’ needs and wishes at the end of life and influence referrals to palliative care.
Methods
Ethical approval was received from the Research Ethics Committee of Cork Teaching Hospitals (CREC). This was a quantitative, cross-sectional design that assessed patients from the Cork University Hospital Oncology Outpatient Department. A 26-item anonymous questionnaire was adapted from Manu et al6, Duke University ‘end of life care survey’ and review of the literature7. Patients with metastatic cancer, who had no previous referral to palliative care, were asked to participate. Ethical approval was received in March 2015 and the study was conducted until September 2015. Informed consent was obtained. Data was analysed using the statistical program SPSS.
Results
Sixty individuals were invited to participate. Forty-four patients participated, a 73% response rate. The mean age of the study population was 54 with a range of 32-84. This sample included 16 males and 28 females. Thirty-eight of the participants identified as Roman Catholic and 43 identified as Irish.
Thirty-three out of 44 (75%) participants strongly agreed with the statement ‘dying patients have the right to be free of suffering’. Twenty-four out of 44 (55%) strongly agreed or agreed with the statement ‘talking about death can make people lose hope’. In relation to hope, 27/44 (61%) strongly agreed or agreed with the statement ‘losing hope makes people die sooner’.
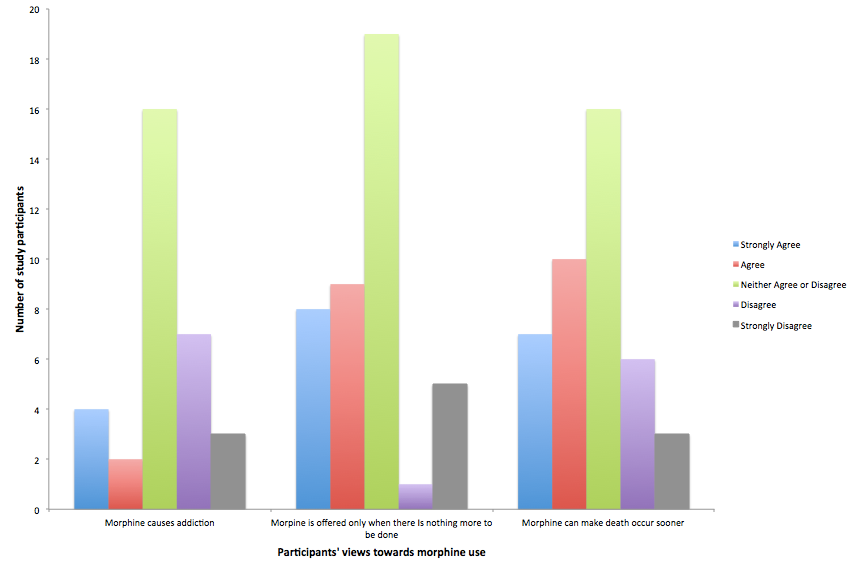
Figure 1 represents participants’ views on opioids. There was no significant relationship found between previous exposure to palliative care (through care of family or friend) and attitudes towards opioid use.
Figure 1: Participants views on morphine use. Participants were asked to respond on a five-point likert scale from strongly agree to strongly disagree to the statements: (a) Morphine causes addiction, (b) Morphine is offered only when there is nothing more to be done, and (c) Morphine can make death occur sooner.
Figure 2 represents participants’ attitudes towards palliative care.
Participants were asked to respond on a five-point likert scale from strongly agree to strongly disagree to the statements (a) Palliative care can make patients feel better and (b) palliative care is offered when nothing more can be done.
In response to the statement ‘palliative care means patients are giving up on living’, 12/44 (27%) strongly agreed or agreed with this statement and 14/44 (32%) responded as ‘unsure’. Thirty-four out of 44 (77%) were familiar with the term palliative care, and 42/44 (95%) were familiar with the term ‘hospice’. Thirteen out of 44 (30%) had previously cared for a dying person. Nine of the 13 (69%) cared for the person in a private home setting. Five of the 13 (38%) reported that the person cared for was offered palliative care. Four of the 13 (31%) were enrolled in palliative care at the time of death.
Twenty-three of the 44 (52%) of the participants reported that they had heard of an advanced care directive (ACD)/living will. Twelve of the 23 (52%) had completed an ACD.
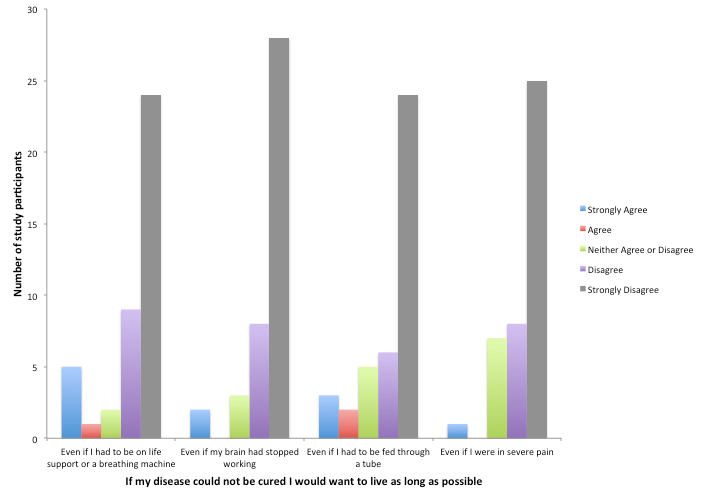
Figure 3 represents participants’ attitudes towards life prolonging measures.
Figure 3: Attitudes towards life prolonging measures. Participants were asked to respond on a five-point likert scale from strongly agree to strongly disagree to the statement; If my disease could not be cured I would want to live as long as possible even if: (a) I had to be on life support or a breathing machine, (b) my brain had stopped working, (c) I had to be fed through a tube, (d) I were in severe pain.
Thirty-three out of 44 (75%) agreed that ‘being comfortable’ and ‘pain free’ would be more important than living as long as possible. Twenty-five of 44 (57%) reported that being at home would be important to them at the end of life. In terms of communication there was a mixed response for comfort level talking about death. Twenty-six out of 44 (59%) reported that they would want their doctor to tell them if they were dying and 32/44 (73%) would tell their family if they were dying.
Using Chi-square analysis, several associations were found to be significant. The relationship between level of education and comfort talking about death was significant with χ2 = 26.982, (p = .042). The relationship between previous care for a dying person and believing palliative care can make you feel better was also significant with χ2 = 10.403, (p = .034). Familiarity with palliative care and thinking it can help you live longer with a χ2 = 10.818, (p = .029). Finally, the relationship between familiarity with palliative care and thinking it is offered when nothing more can be done was also significant with χ2 = 10.095, (p = .039).
Discussion
This study assessed several aspects of palliative and end of life care. Several clinically useful themes emerged providing insight to patients’ opinions.
The majority reported that palliative care is beneficial. Almost all participants were familiar with the term hospice but only 34 were familiar with the term palliative care. A majority believed that palliative care was offered when nothing more could be done. The view that it is a last resort is a barrier to early referral. These results may reflect a lack of understanding or knowledge of palliative care, its role and the resources it offers6. However, a similar number also reported that palliative care could make people feel better. Significant associations were found between previous exposure to palliative care and believing that palliative care could make you feel better and help you live longer. More awareness and education about what palliative care is and its value for patient, their families and other health care providers is needed.
A second theme was attitudes towards opioids. A study, by Conrardy et al8, reported that many patients had misconceptions about opioid addiction. Their perceptions ranged from not knowing if they were addictive or underestimating their personal risk of addiction to overly fearing addiction8. The current survey found that individuals tended to be either unsure of the potential addictive nature of opioids or disagreed with statements indicating that opioids caused addiction. There was no association found between previous exposure to palliative care, through caring for a relative or friend, and opinions on the addictive nature of opioids. More education is needed for patients on the use of opioids in palliative care.
Results show that comfort and symptom control are more important to patients than life prolonging measures. This is important for both health care providers and next of kin to be aware of especially when working with patients whose wishes are unknown9. Few respondents had thought about what medical care they would like at the end of life. The majority wanted to be told by their doctor if they were dying. Interestingly, more responded to wanting to inform their families they were dying than wanting to be informed themselves. This may reflect the age demographic in this largely older, Catholic sample. Good palliative care helps open up discussion with patients and their families about important aspects of end of life care. Those surveyed had no exposure to palliative care which may account for the fact that few had considered the type of medical care they would prefer. Twenty three out of 44 had heard of an advanced care directive/living will and of these only 12 had completed one. Over half reported that their preferred place of death is their own home. Palliative care support enables people to choose to die at home where possible.
The importance of hope was another theme highlighted. More than half reported that talking about death can make people lose hope. More reported that losing hope made people die sooner. This is concordant with literature reports demonstrating that physicians reported a delay or reluctance to refer to palliative care as they were afraid of ‘destroying hope’7,10. In this study, there were mixed reports about how comfortable patients felt talking about death. This is not restricted to the patient population, as several surveys show there is variable physician comfort in talking about death and dying. The study by Dunlay et al11, demonstrated clinicians’ uncertainty about who should initiate end of life discussion. Thirty percent of clinicians reported low or very low confidence in commencing these dialogues.
The main limitation of this study is the small sample size. We cannot be certain if the results are representative of the general population. There was bias and screening present during patient selection, which was not consecutive. Clinic doctors advised that some patients may not be eligible if they had received their cancer diagnosis that day or if it was felt that the survey would be burdensome at that point in time. Finally, the questionnaire used was adapted from previous studies and the validity of the tool is unknown. However, a strength is that there are minimal studies that look at the patient’s perspective on these issues and none to date in Ireland.
This study has helped to gain insight into patients’ attitudes towards palliative and end of life care. It highlights the need for more education and promotion of palliative care. Several factors were identified that may prevent early referral to palliative care including believing palliative care is a last resort and fear of destroying hope by introducing palliative care. Further research and understanding of these factors will be valuable.
Acknowledgements
A special thanks to Shane Singh, Stephen Shannon and Gavin Bock for their assistance in data collection. Also to the staff of the Cork University Hospital Outpatient Department, this project would not have been possible without their support.
References
1 Kwon J, Hui D, Chisholm G, Ha C, Yennurajalingam S, Kang J, Bruera E. Clinical Characteristics of cancer patients referred early to supportive and palliative care. Journal of Palliative Medicine 2013;16(2):148-155.
2 Temel J, Greer J, Muzikansky A, Gallagher E, Admane S, Jackson V, Constance M, Blinderman C, Jacobsen J, Pril W, Billings J, Lynch T. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363:733-742.
3 Brickner L, Scannell K, Marquet S, Ackerson L. Barriers to hospice care and referrals: survey of physicians' knowledge, attitudes, and perceptions in a health maintenance organization. J Palliat Med 2004 Jun;7(3):411-418.
4 Ogle K, Mavis B, Wyatt G. physicians and hospice care: attitudes, knowledge, and referrals. J Palliat Med 2002;5(1):85-92.
5 Friedman B, Harwood M, Shields M. barriers and enablers to hospice referrals: an expert overview. J Palliat Med 2002;5(1):73-84.
6 Manu E, Mack-Biggs TL, Vitale CA, Galecki A, Moore T, Montagnini M. Perceptions and attitudes about hospice and palliative care among community-dwelling older adults. Am J Hosp Palliat Care 2013 Mar;30(2):153-161.
7 Ahluwalia SC, Fried TR. Physician factors associated with outpatient palliative care referral. Palliat Med 2009 Oct;23(7):608-615.
8 Conrardy M, Lank P, Cameron KA, McConnell R, Chevrier A, Sears J, Ahlstrom E, Wolf M, Courtney D, McCarthy D. Emergency department patient perspectives on the risk of addiction to prescription opioids. Pain Med 2015 Sep 1.
9 Ackermann RJ. Withholding and withdrawing life-sustaining treatment. Am Fam Physician 2000 Oct 1;62(7):1555-60, 1562, 1564.
10 Karim KB. Nonwhite ethnicity and the provision of specialist palliative care services: factors affecting doctors' referral patterns. Palliat Med 2000 11;14(6):471-478.
11 Dunlay, Shannon MFoxen, Jilian LCole, TereseFeely, Molly ALoth, Ann RStrand, Jacob JWagner, Jean ASwetz, Keith M Redfield, Margaret M. A survey of clinician attitudes and self-reported practices regarding end-of-life care in heart failure. Palliat Med 2015 03;29(3):260-267.
P405